Abstract
Objective: This study aims to understand the trend of research conducted on issues of maternal health in India considering data provided in five rounds of National Family Health Survey (NFHS).
Methods: Systematic review of literature has been conducted using multi-stage search and review process adapted from Page et al.’s (2021) PRISMA. Initially 14,570 studies were identified and only 134 articles meeting selection criterion were considered in this study.
Results: Approximately 32% studies have focused on regional and state variation of maternal health status; while 27% dealt with utilization of maternal healthcare services; and 19% the socio-economic determinants of maternal health. While few studies have discussed the place of delivery, antenatal care and post-natal care visits, only five studies focus on issues related to women’s autonomy, including their health-seeking behaviour, knowledge, attitude and practices related to maternal health.
Conclusion: Non-communicable diseases and its role in maternal health still remains an unexplored domain of research on maternal health in India. Moreover, there exists geographical skewness in the number of studies conducted, focusing especially on few provinces while none on few others.
Introduction
Maternal health, defined as the health of women during pregnancy, childbirth and the postpartum period, is an important indicator of development. Maternal mortality is considered to be a key measure of maternal health. As per the Sample Registration System (SRS) report by Registrar General of India (RGI), Maternal Mortality Ratio (MMR) in India was 113 per 100,000 live births during 2016–18, which is high compared to other developing nations. Some of the basic maternal health parameters include institutional deliveries, deliveries conducted by health personnel, antenatal care (ANC), postnatal care (PNC), and pregnancy outcomes [1]. There has been significant number of studies on maternal health and most of them have examined perspective of utilization and factors impacting maternal health. Few articles depicted background factors like education, maternal age, birth order, availability, accessibility and affordability of health care, wealth index, non-communicable diseases (NCDs), maternal infections, nutrition and lifestyle, strongly impact pregnancy outcomes in developing countries [2–7].
Millennium Development Goals (MDGs) adopted by United Nations in 2000 is one of the dominant reasons to focus research on maternal health. Out of the 18 goals, goal 5 has emphasised on improving maternal health. Later on, the failure of reaching MDG target instigated further research on maternal health. Apart from MDGs, few health policies and programmes in India, like National Health Mission (NHM), National Population Policy (NPP) in 2000 also retaliated discrepancies in maternal health and emphasised on reducing maternal mortality to improve maternal health. Sustainable Development Goals (SDGs) were launched in 2015 with broader goals and targets than MDGs. All these attracted large volume of research on maternal health in India. Thus, maternal health remains a major public health concern in India and there have been large disparities noticed at the provincial level as well as among various social groups.
Several health surveys are conducted in India, such as, Annual Health Survey (AHS), Indian Human Development Surveys (IHDS), District Level Household Survey (DLHS), National Family Health Survey (NFHS). These provide useful data on various indicators of maternal health. However, there is lack of consistency of data in these surveys. A study on review of national health surveys in India explicitly discussed that all these surveys cannot be compared due to several reasons [8]. First, not all indicators of maternal health were included in each survey. Second, many did not provide data for all provinces of India, for instance, AHS was conducted for the nine empowered action group (EAG) provinces. Third, none of these surveys have been conducted over same time period and many were discontinued after a couple of rounds of survey. Thus, a study suggested implementing one comprehensive survey that provides detailed information on relevant health indicators [9]. NHFS is considered to be robust and has been collecting data on all indicators of maternal health for entire geographical region of India since 1992 till 2021. Hence, in this review, studies based only on NFHS data have been analysed. There is a lack of review publications that collate evidences and highlight the issues on utilization of NFHS data for understanding maternal health situation.
Numerous studies have been published on maternal health. Most of the research have focused only on few aspects of maternal health such as, determinants and utilization of maternal health, delivery complications, etc. Though some health challenges like cultural issues, delaying obstetric care and service influences maternal health [10]. Either studies have been oriented only to examine ANC, PNC, and other determinants or conducted comparative regional analysis focusing on few provinces, lacking holistic approach to understand and analyse the scenario of maternal health in India. Therefore, through a systematic review of literature this study aims to focus on an overall understanding of which domains have been over-emphasised and which have been overlooked while discussing maternal health in India.
Methods
To proceed with systematic review approach, multi-stage search and review process from Page et al.’s (2021) PRISMA flow diagram as explained in Figure 1 was adopted. Literature was searched in organized steps on various online databases, including PUBMED, JSTOR, and Google Scholar. Initially 14,570 studies were identified. Due to the Covid pandemic, articles that are available only on digital platforms have been considered. Moreover, articles using specifically NFHS data have been examined in this study. NFHS is considered to be the Indian version of Demographic and Health Surveys (DHS). The first round of NFHS was conducted in 1992–1993, followed by four subsequent rounds- NFHS 2 (1998–1999), NFHS 3 (2005–2006), NFHS 4 (2015–16), and NFHS 5 (2019–2021).
FIGURE 1
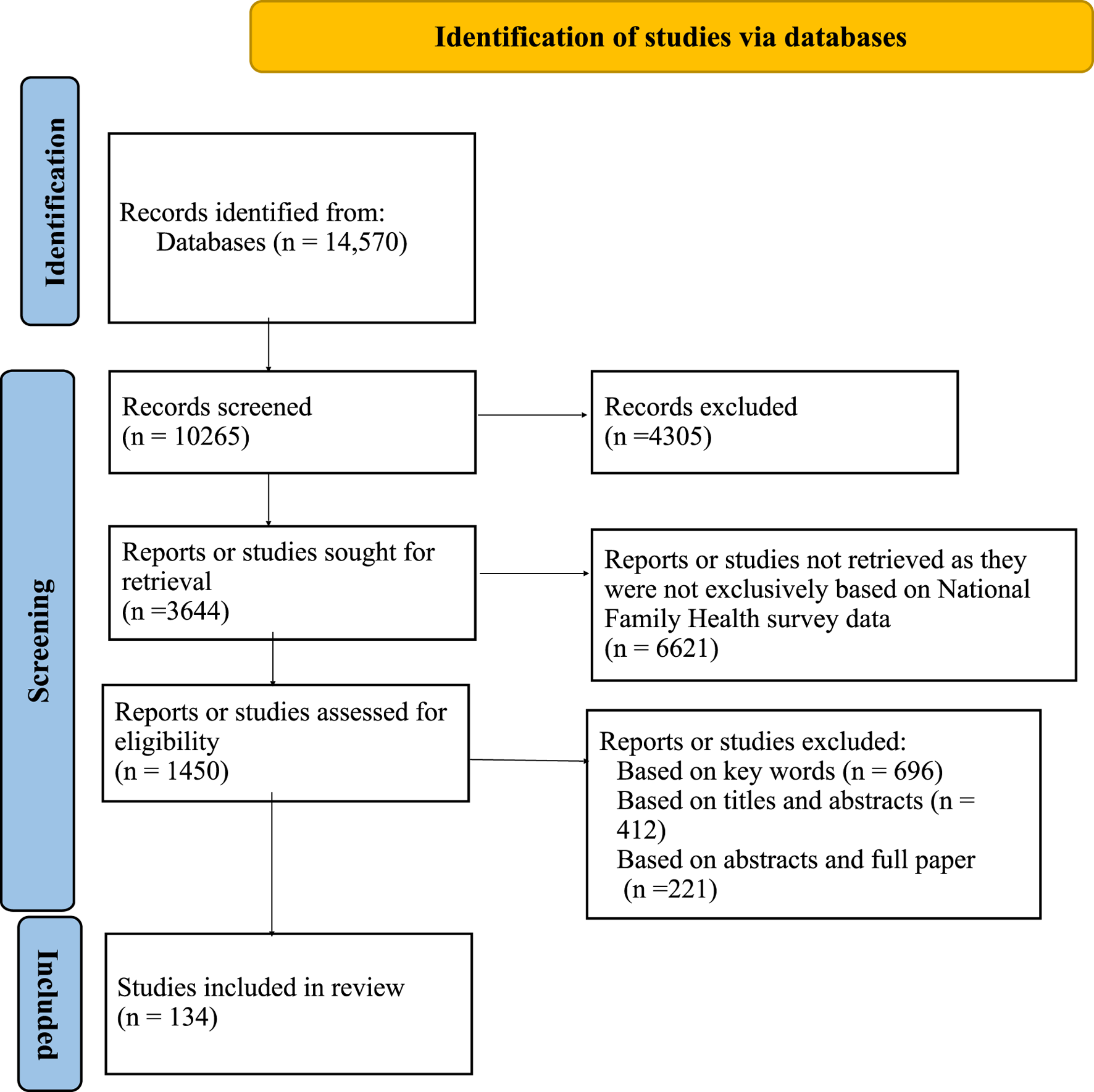
PRISMA flow diagram for articles selection (India, 1992–2022).
After preliminary screening 10,265 studies were found and 4,305 studies were rejected based on several selection criterion. Studies that have used only NFHS data for analyzing maternal health and were published between 1992 and September 2022 are considered for this review. Based on this criterion 3,644 studies were sought for retrieval. Literature was searched and included in three stages. Total 1,450 studies were assessed for eligibility. In the first stage combinations of some generic keywords were used, such as, maternal health, NFHS, India. Few other words were added, like, utilization of maternal healthcare, maternal health outcomes (pregnancy), ANC, PNC, Iron Folic Acid (IFA) tablets consumption. In the second stage of literature search, to make the search more robust another set of keywords were included, for example, pregnancy, institutional delivery, maternal complications and morbidity, breastfeeding. Based on keywords, 696 studies were excluded. In the third stage title and abstracts of these articles were shortlisted. Then articles for which full texts were available were further reviewed. Thus, 412 studies were excluded based on titles and abstracts. While 221 studies were not included as full paper was not available. Using these inclusion and exclusion criterion, this paper is based on systematic review of 134 studies. Since only three studies have been published (until September 2022) using NFHS 5, therefore these three studies are not included in figures, as it would not depict the actual scenario.
Results
All literature were arranged based on specific rounds of NFHS for which data had been considered in that study. This information enabled us to comprehend the trend of data analysis. Figure 2A (Studies published on maternal health using NFHS data) diagrammatically represents the trend of these data analysis. It is evident from the line graph that publications using NFHS data sets have increased since its inception. The peak in publication is noticed between NFHS 3 and NFHS 4. Considering the inclusive criteria, keywords and other factors, this review depicted only six studies on maternal health using NFHS 1, 15 studies using NFHS 2, 31, and 45 studies using NFHS 3 and NFHS 4 data, respectively. Only three studies have been reviewed using NFHS 5 data which is published until September 2022.
FIGURE 2
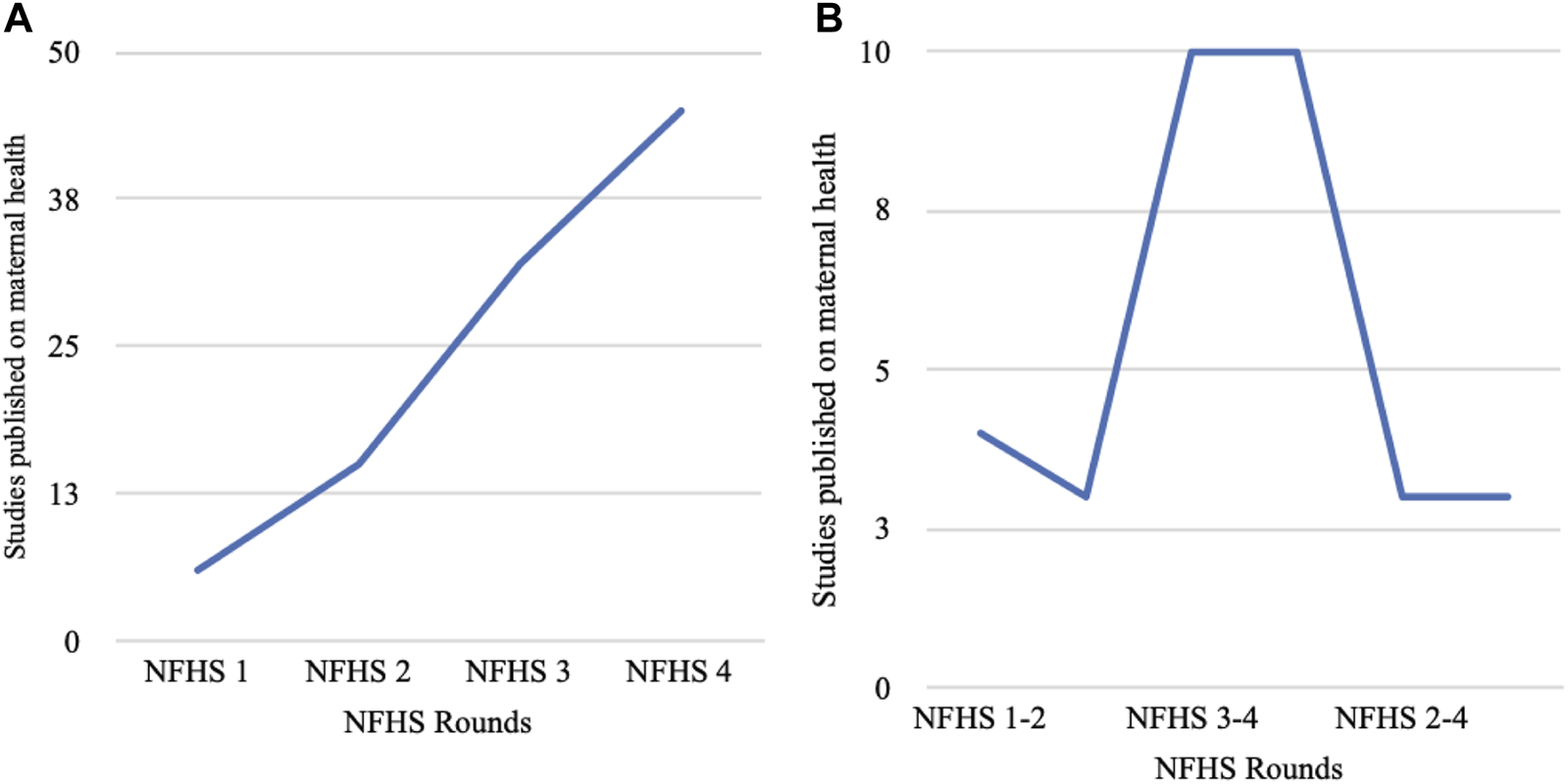
Studies published on maternal health using National Family Health Survey data (India, 1992–2022). (A) Studies based on single round of NFHS surveys. (B) Studies based on combined rounds of NFHS surveys.
Certain contextual situations that shaped this trend with an increasing number of studies on maternal health can be explained by various changes in the policies on health, at global and national levels, that brought maternal health at forefront of health research. In the early 1990’s focus on reproductive and child health was not very profound in India. However, in the International Conference on Population Development (ICPD) in 1994 which also inspired NPP 2000 in India, women’s health was prioritized with special focus on reproductive and child health. This inspired academicians to conduct studies on these issues and maternal health being the most important component of reproductive health in India, surfaced as an integral part of such studies. Moreover, inception of the MDGs (2000) and SDGs (2015) listed improving maternal health as an important goal to achieve development. Thereafter several programs and policies that Indian government implemented implicated to improve maternal health and reduce maternal mortality. Due to this there has been a sharp increase in published articles from NFHS 3. This necessitated and encouraged more research on maternal health, especially analyzing trend and improvement in maternal health in India. Apart from policy changes, academicians and public health researchers in India got more familiarized with the rich source of NFHS data. In the initial rounds of NFHS researchers were still getting used to the enormous amount of information provided on maternal health on various indicators that were not earlier accessible in public domain. Nevertheless, over a period of time NFHS data were widely publicized and there was an increase in the amount of research conducted using these data sets.
Indicators on RMNCH + A
This review has explored the perspective of maternal healthcare utilization based on five indicators (mothers who had full ANC, mothers who had three or more ANC, institutional delivery, skilled birth attendance, and PNC) given in RMNCH + A [1]. It is explicitly explained in Table 1, that 15 studies have specifically looked into all these five indicators of maternal health as per RMNCH + A, while ANC and institutional delivery have been specifically explored in nine and five studies, respectively. Among these, three studies were conducted using NFHS 3 [11–13], and five studies using NFHS 4 [14–18], other five studies using several combined rounds of NFHS [19–23]. It is evident from Table 1 that studies which have included PNC are mostly conducted during NFHS 3 and NFHS 4. However, it also needs to be noted that 17 studies have looked into the indicators of maternal health except for PNC. Out of 17 studies, four studies used NFHS 1 [24–27], and five studies used NFHS 2 [28–32], one study used NFHS 3 [33] and two used NFHS 4 data [34, 35]. Combined rounds of NFHS were used in four studies [36–39]. Five studies have specifically focused on institutional delivery including C-section delivery, in which three studies were conducted using NFHS 1 [40], NFHS 2 [41], and NFHS 4 [42], respectively. While two studies used both NFHS 4 and 5 [43, 44], nine studies have exclusively looked into ANC. Out of these nine studies, three studies are based on NFHS 2 [45–47], while one study on NFHS 3 [48] and four studies on NFHS 4 [49–52]. One study used NFHS 3–4 [53] for understanding the socioeconomic and geographical inequalities of ANC. The role of skilled birth attendees in maternal health has been examined in one study using NFHS 3 [54]. Two studies have focused on maternal health through the reproductive health index using NFHS 1 [24] and NFHS 3 [55] data. Two other studies have focused on pregnancy complications and adverse pregnancy outcomes on NFHS 4 [56] and all four rounds of NFHS [57].
TABLE 1
| Indicators | NFHS rounds | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| NFHS 1 | NFHS 2 | NFHS 3 | NFHS 4 | NFHS 3–4 | NFHS 1–2 | NFHS 2–4 | NFHS 1–3 | NFHS 1–4 | NFHS 4-5 | |
| All five indicators of maternal health (RMNCH + A) | 0 | 0 | 3 | 7 | 1 | 0 | 2 | 1 | 1 | 0 |
| All indicators of maternal health except post-natal care | 4 | 5 | 1 | 2 | 1 | 1 | 0 | 2 | 1 | 0 |
| Institutional delivery (including C-section) | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 2 | |
| ANC (three or more and full) | 0 | 3 | 1 | 4 | 1 | 0 | 0 | 0 | 0 | 0 |
| Skilled birth attendees | 1 | |||||||||
| Maternal health through reproductive health index | 1 | 1 | ||||||||
| Pregnancy complications and adverse pregnancy outcomes | 1 | 1 | ||||||||
Frequency of studies based on specific maternal health indicators based on Reproductive, Maternal, Newborn Child plus Adolescent Health (India, 1992–2022).
Age of Women
The review suggests that majority of articles include women belonging to 15–49 years. However, four studies [13, 14, 23, 33] have specifically analysed the age group of 15–19 years, other four studies examined 15–24 years [36, 55, 58, 59] and one study considered 20–24 years [60]. The age group of 15–24 years is considered to be vulnerable and maternal health behaviour at an early age ultimately affects pregnancy outcomes and reproductive health of women in later years. Studies on early pregnancy between 15–24 years have examined indicators like ANC and skilled birth attendees.
A study based on NFHS 1- NFHS 3 described the socio-economic disparities of maternity care among adolescent (15–19 years) women in India. It stated that proportion of adolescent women availing skilled birth attendees and full ANC has increased from 1990 to 2006 though 43% of women were married before the legal age [23]. Studies using NFHS 3 data on maternal care utilization among married adolescent (15–19 years) women depicted early childbearing and poor maternal health experiences are intimately linked to their educational and economic status [12, 33]. A similar study on NFHS 3 detected young women are less likely to have institutional delivery. Adolescent women (15–19 years), mostly in rural areas, lack autonomy and pregnancy related knowledge, resulting in lower maternal health service utilization [13].
Another study analysing four rounds of NFHS data (NFHS 1- NFHS 4) focused on maternal healthcare utilization in India among young women (15–24 years) [36]. This study contended that skilled birth attendees have increased since NFHS 1 among young women. However, a significant proportion of young women have not opted for full ANC during pregnancy. A study on mis-timed and unwanted pregnancies based on NFHS 3 found women in younger age group (15–24 years) are more likely to have mis-timed pregnancies whereas the likelihood of unwanted pregnancy is more among older women [59]. Another study on early marriage and its impact on reproductive health on NFHS 3 revealed women marrying early (before 18 years of age) were more likely to have poor reproductive health, experience child loss, and poor anthropometric indicators among children born [55]. This study has divided the age group into 10–19 years (adolescent), 20–24 years (young adulthood) and 25 years or older (adulthood). Lower education, poor living conditions, and less access to healthcare services result in adverse adolescent pregnancy outcomes [58]. Another study elaborated a significant association between unwanted pregnancies, pregnancy termination, and sterilization with lower age of marriage [60].
Against this backdrop, Figures 2A,B (Studies published on maternal health using various rounds of NFHS data) depicts the trend of how data from several rounds of NFHS were considered for understanding maternal health issues. This line graph is curvilinear in nature and shows nine studies have used NFHS 1–3 and NFHS 3–4. The publication increases in NFHS 3–4 and NFHS 1–3. However, only two studies have all four rounds of NFHS data. Majority of the articles have been published using NFHS 2–3 and NFHS 1–3. However, it should be noted that due to inclusion of new maternal health indictors in NFHS 4, sometimes research using combined rounds of all NFHS might be difficult. The following sections provide a nuanced analysis of maternal health conditions in each of the rounds of NFHS.
National Family Health Survey 1 (1992–93)
Though only six studies were conducted on NFHS 1, yet they covered a range of issues. A study analysed the impact of caste on reproductive health variation among women and computed the Reproductive Health Index (RHI) in the eastern provinces of Bihar (including Bihar and Jharkhand), Orissa and West Bengal [24]. This study depicted caste to be an important predictor of reproductive health. Women belonging to upper caste are likely to have high RHI as compared to lower caste, due to better socio-economic status influencing their reproductive choices. Another study established similar findings, where women belonging to the scheduled caste (SC) are likely to have more complications due to caste influence on healthcare provisions [25]. Women belonging to economically, socially, and educationally weaker sections receive less maternal healthcare services in the southern states [26]. Education, parity, religion, caste, and place of residence impact breastfeeding activity of women [61]. Three articles have examined aspects of unmet need, breastfeeding, and C-section [14, 40, 62]. Maternal healthcare utilization is also influenced by type of health services [27]. However, there was major focus on various social determinants of maternal health, but family planning aspects, maternal mortality and morbidity were not covered in any of these studies. This might be attributed to the ongoing trend in research that gave more emphasis on factors influencing maternal health rather than outcome health status. There had been more emphasis on regional studies. Such studies allowed us to contextualize the broader framework for analysing maternal health scenario in India.
National Family Health Survey 2 (1998–99)
Studies using NFHS 2 data on reproductive and maternal health have increased and included new aspects in research. Based on our inclusion criterion, 15 articles have primarily used NFHS 2 data for their analysis. It has been noticed that studies in NFHS 2 focused on ANC, PNC, service care utilization, C-section, and socio-economic determinants impacting maternal health. Out of 15 studies, seven studies have analyzed maternal healthcare utilization and socio-economic factors impacting maternal health [28, 29, 31, 32, 45, 47]. A study revealed that if socioeconomic and demographic factors were controlled then household type influences utilization of maternal health services [63]. This study stated women living in nuclear family have higher chances of utilizing maternal health services like ANC, PNC, etc. than those living in non-nuclear households. Another study was conducted in Bihar, Madhya Pradesh, Rajasthan, and Uttar Pradesh on ANC and indicated uneducated and poor pregnant women with at least one child were least likely to receive ANC and other services in these provinces [46]. Similar study was conducted in Uttar Pradesh looking into the pregnancy complications and health-seeking behaviour among married women. This study found nutritional status of women influences health problems during pregnancy [30]. Socio-demographic factors including place of residence, religion and caste, educational status of woman, woman’s work status, standard of living of the household, media exposure, age of mother at time of childbirth, birth order and birth interval impact pregnancy complications and their health seeking behaviour. Women belonging to rural areas and higher birth order have higher chances of delivering at home than in a public facility [41]. Factors, like availability of doctors, waiting time, cleanliness and affordability enhances the probability of reproductive healthcare uses [31]. It is evident from the above discussion that articles using NFHS 2 data have not examined aspects of family planning and role of skilled birth attendants. Compared to NFHS 1, there has been an increase in regional studies on maternal health, though there were no studies on provinces of Chhattisgarh, Goa, Gujarat, Haryana, Himachal Pradesh, Odisha, Sikkim, West Bengal, Punjab, and Tripura.
National Family Health Survey 3 (2005–06)
There was a steady rise in number of publications based on NFHS 3 with a total of 31 articles. Three articles examined maternal healthcare utilization at provincial level [26–28] while two articles analysed child health and fertility [60, 64]. Like in the previous rounds of NFHS, in round three also some common areas have been focused on, such as ANC, PNC, safe delivery, C-section, role of economic factor and women’s autonomy. However maximum studies (23 studies) have pointed that there is a strong relationship between education and maternal health. Place of residence has emerged as another important factor in maternal health. In 2011 one study reported that women living in urban areas are more likely to use skilled birth attendants and stated about several financial, social, regional, and cultural barriers affecting availability and utilization of skilled birth attendant in India [54]. A study initiated that spousal violence likely affects maternal and child health (MCH) care. They depicted women experiencing any kind of spousal violence were less likely to use full ANC than those who did not experience any violence [35]. Women in the early ages are less likely to utilize maternal and child health services compared to those in the late age groups [33]. In a similar study it was established there has been a detrimental effect on reproductive health due to early marriage that often results in unplanned pregnancies, early motherhood, and abortions [55]. Articles using NFHS 3 data sets primarily focused on well-defined role of socio-demographic factors, regional differentials, nature of the household, ANC, C-section, spousal violence and women’s autonomy. Knowledge, attitude, adolescent motherhood, unwanted pregnancies and spousal violence were studied using NFHS 3 datasets which were not considered earlier.
National Family Health Survey 4 (2015–16)
Based on inclusion criteria 45 articles on maternal health using NFHS 4 data were considered. It is evident from the published articles many common areas (such as determinants of maternal health, rural- urban differentials, and maternal health utilization, delivery care) have been over-emphasised like in the earlier rounds of NFHS. Articles have examined role of ANC and its influencing factors, C-section and regional disparities. Four studies have used spatial analysis in understanding maternal health care utilization [14, 15, 42, 65]. Studies established a strong association between mass media and maternal health in India [14–16, 42, 49, 56]. Usage of phone is positively associated with skilled birth attendance, PNC, usage of modern contraceptives but it is negatively associated with early ANC [17]. Utilization of Integrated Child Development Services (ICDS), registration of pregnancy and health insurance coverage increases the odds of full ANC utilisation [50]. Two studies highlighted men’s presence during ANC visits influences institutional deliveries [51, 66]. Poor sanitation practices adversely affect pregnancy outcomes [52]. Informed choice plays a pivotal role in use of modern contraceptive methods and may result in lower post-natal health problems, unmet need for contraceptives, unintended pregnancies, induced abortions, which adversely affect women’s health [34]. Articles have analysed role of women’s autonomy and found significant association with increasing odds of maternal healthcare services [18]. Decreased ANC, PNC, and institutional deliveries during Covid 19 pandemic are also noticed [67]. There have been considerable research in India on maternal health using NFHS 4 wherein socioeconomic factors along with utilization of maternal health care services have been overstated. New research areas like women’s autonomy, abortion, miscarriage and adverse pregnancy outcomes, use of contraception, role of skilled birth attendant was discussed in the studies based on NFHS 4. However, role of men and NCDs in maternal health need more attention for future research.
National Family Health Survey 5 (2019–21)
The NFHS 5 data was released in May 2022, therefore only few studies have been published based on these data and only three studies have met the inclusion criteria. One of the studies analyzed changing scenario of C-section delivery [43]. It depicted that more than one-fifth of the institutional deliveries are C-section in most Indian provinces with maximum prevalence in southern provinces of Telangana, Kerala, and Andhra Pradesh. Another study was conducted on geographic and economic inequalities in C-section in the various districts of Bihar and reported that C-section delivery rate has increased from NFHS 4 to NFHS 5 [44]. Both these studies contend that increasing age of women, literacy of women, and economic strata are positively associated with C-section delivery in India [43, 44]. Critical appraisal of NFHS 5 data on maternal health indicator revealed prevalence of anaemia during pregnancy has increased from 15 to 17 provinces as compared to NFHS- 4 [68]. It was interesting to note that out of the three studies, two of them have emphasized on increasing C-section deliveries in India. Does this indicate that institutional delivery is promoting C-section? However, it needs to be mentioned that these three studies have used factsheets rather than raw data for analysis.
Combined Rounds of National Family Health Survey
There are nine articles that have been published using NFHS round 1–3 and 11 using NFHS 3–4. However, only two articles have been published on maternal health using all four rounds of NFHS data [19, 36]. Study based on all the four rounds of NFHS datasets evaluated trends and determinants of maternal health care service utilization among young married women from 1992 to 2016 [36]. They stated that use of full ANC has increased from NFHS 1 to NFHS 4. Spousal violence has been an impounding factor impacting maternal health and studies show women experiencing physical violence from their husbands are less likely to adopt contraception and often experience unwanted pregnancy [57]. Several articles have inspected the differentials and determinants of maternal healthcare utilization [21, 22, 37–39, 53, 69]. A study scrutinized into this aspect using pooled data from 1998 to 1999 to 2015–2016, wherein illiteracy, women having five or more children, belonging to scheduled tribes, living in rural areas were associated with significantly low utilization of maternal health care services [21]. Two articles highlighted the importance of National Health Mission and Janani Suraksha Yojana for understanding maternal health in India [20, 70]. Articles published using data from NFHS 1–2 focused on broad aspects of breastfeeding, ANC- PNC care, and regional variation. A study based on NFHS 3–4 revealed socio-economic characteristics especially wealth status is a significant predictor of full ANC visits and institutional delivery in West Bengal [71]. Our review revealed that articles using more than one round of NFHS have basically analysed the change and trend of maternal health over the years focusing on time-series analysis.
Based on this systematic review a graphical representation about distribution of areas focused on maternal health has been presented in Figure 3 (Areas focused on maternal health using NFHS data). For preparing this pie diagram, the title and keywords of literature included in the review were considered. On basis of it, broad 15 categories of research areas were identified. Articles with common areas of interest have been included in multiple categories depending on their main focus. From the pie diagram it can be deduced that maximum articles have focused on regional and provincial variations (40 articles) of maternal health status followed by utilization of maternal healthcare services (32 articles). 24 studies have examined socio-economic determinants of maternal health. Eight studies have emphasised adolescent pregnancy, majorly on ANC and skilled birth attendees. This highlights the need to look into role of teenage and adolescent pregnancy and utilization of all-round maternal health services as well as pregnancy outcomes. It is evident from literature that socio-demographic factors are being illustrated in most of the studies either explicitly or indirectly. Delivery and pregnancy complications, ANC, PNC visits have been described in few studies. Women’s autonomy, particularly their role in maternal health, including their health-seeking behaviour, knowledge, attitude, and practices have been discussed in four to five articles. With new rounds of NFHS, spatial analysis is being used thoroughly. But articles considering knowledge, attitude and practices, pregnancy outcomes, role of men in maternal health, NCDs were scarce and needs more attention in future research. Therefore, this representative diagram gives us a snapshot of areas that have been researched since NFHS 1 till NFHS 4.
FIGURE 3
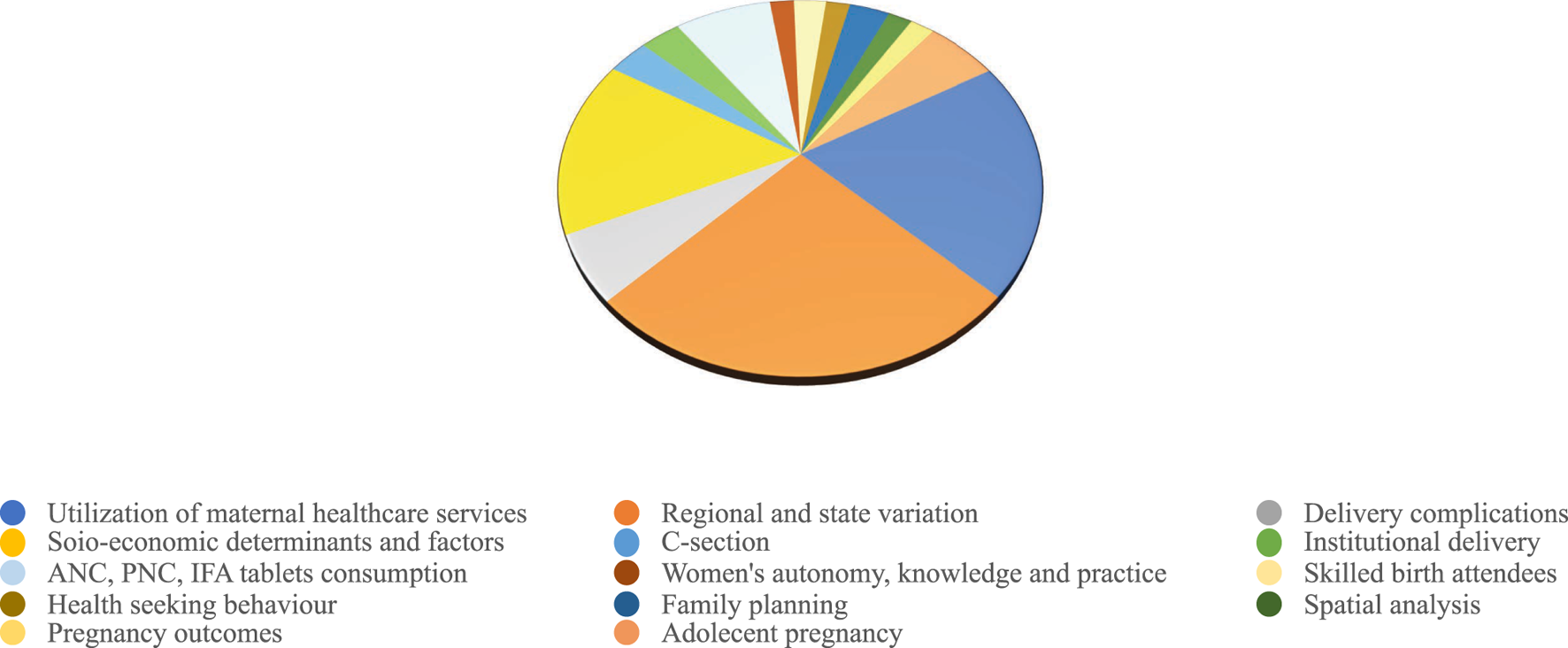
Areas focused on maternal health using National Family Health Survey data (India, 1992–2022).
Table 2 (Geographical variation of areas focused on maternal health using NFHS data) shows the geographical variation of areas focused on maternal health using NFHS data. Studies covering entire country has increased since NFHS 1, the probable reason could be due to implication of policies and programmes focusing on maternal health. With the availability of district level data EAG provinces especially Bihar (14), Madhya Pradesh (9) and Uttar Pradesh (13) have been focused most. However, we could not find any study on Himachal Pradesh, Gujarat, Punjab. Among the North-Eastern provinces, Manipur (3) has maximum studies.
TABLE 2
| States | NFHS 1 | NFHS 2 | NFHS 3 | NFHS 4 | NFHS 5 | NFHS 2 &3 | NFHS 1–3 | NFHS 1& 2 | NFHS 3& 4 | NFHS 2–4 | NFHS 1–4 | Total (n) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| India | 3 | 6 | 17 | 31 | 2 | 2 | 7 | 3 | 6 | 3 | 2 | 82 |
| Andhra Pradesh | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 4 |
| Arunachal Pradesh | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| Assam | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Bihar | 1 | 3 | 1 | 5 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 14 |
| Chhattisgarh | 0 | 0 | 0 | 2 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 3 |
| Goa | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| Gujarat | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Haryana | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| Himachal Pradesh | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Jammu and Kashmir | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Jharkhand | 0 | 2 | 0 | 2 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 6 |
| Karnataka | 1 | 1 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 |
| Kerala | 1 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 4 |
| Madhya Pradesh | 0 | 2 | 1 | 5 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 9 |
| Maharashtra | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 |
| Manipur | 0 | 1 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 |
| Meghalaya | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| Mizoram | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| Nagaland | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| Odisha | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| Punjab | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Rajasthan | 0 | 2 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 5 |
| Sikkim | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| Tamil Nadu | 2 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 7 |
| Telangana | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Tripura | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Uttar Pradesh | 0 | 3 | 4 | 3 | 0 | 0 | 2 | 0 | 1 | 0 | 0 | 13 |
| Uttarakhand | 0 | 2 | 1 | 2 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 6 |
| West Bengal | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 3 |
Geographical variation of areas focused on maternal health using National Family Health Survey data (India, 1992–2022).
Bold indicate studies that covered entire India, while other studies have focused on particular provinces in India.
Discussion
In India, maternal health is one of the pinnacles of public health discussions and debates by academicians, researchers, and policy makers. This review attempts to indicate the use of NFHS data for understanding maternal health situation in India. The findings suggest quite a lot of studies have been published on maternal health using NFHS datasets. Studies have analysed maternal health on wide spectrum at national, provincial, and district levels. Several aspects of maternal health, such as service utilization and health seeking behaviour (ANC, PNC, consumption of IFA tablets), regional variation, and role of socio-economic determinants have been studied excessively since the inception of NFHS 1 till NFHS 5. Few studies have examined unintended pregnancies and its impact on pregnancy outcomes as well as family planning methods. One of the most significant findings based on this systematic review is that out of 134 articles, 58 have highlighted the importance of education and its association in influencing maternal health. This reiterates that education is one of the most important social determinants, especially influencing maternal health. Literacy or community level education of pregnant mothers is important for understanding the effects of pregnancy, taking care of themselves, the role of midwives and nurses for experiencing healthy pregnancy [72]. This review has found that scholarly work using NFHS data has extensively exaggerated socio-economic and demographic factors, health seeking behaviour along with other co-health issues. There has been a focus to look into the geographical variation, in this EAG provinces have been emphasised the most. The review also highlighted that the role of NCDs on impacting maternal health, pregnancy complications have not been addressed rigorously, though few studies have focused on this issue partially. Therefore, this review will be insightful in the forthcoming research, so that more priority can be given in the domains that are having scarce research.
Statements
Author contributions
PR: PI of the project on which the study is based; conceptualised the paper; designed the literature search and review; decided on the screening criterion for the literature; thematically categorised the analysis; edited and prepared final draft of the paper. NG: initiated the draft of the paper; conducted the literature search; prepared all tables, diagrams, and references.
Funding
This is a part of a project (Project No. P3593/100) that was funded by Indian Council of Social Science Research (ICSSR) under IMPRESS scheme and Ministry of Education.
Acknowledgments
Authors would like to acknowledge their contribution in carrying out this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.
Ministry of Health and Family Welfare, Government of India. A Strategic Approach to Reproductive, Maternal, Newborn, Child, and Adolescent Health (RMNCH+A) in India. New Delhi: Ministry of Health & Family Welfare, Government of India (2013).
2.
Urassa E Lindmark G Nystrom L . Maternal Mortality in Dar Es Salaam, Tanzania: Socio-Economic, Obstetric History and Accessibility of Health Care Factors. Afr J Health Sci (1995) 2(1):242–9. 10.1186/1471-2393-14-320
3.
Mbizvo MT Fawcus S Lindmark G Nyström L , Maternal Mortality Study Group. Maternal Mortality in Rural and Urban Zimbabwe: Social and Reproductive Factors in an Incident Case-Referent Study. Soc Sci Med (1993) 36(9):1197–205. 10.1016/0277-9536(93)90240-5
4.
MacLeod J Rhode R . Retrospective Follow‐up of Maternal Deaths and Their Associated Risk Factors in a Rural District of Tanzania. Trop Med Int Health (1998) 3(2):130–7. 10.1046/j.1365-3156.1998.00174.x
5.
Lakew D Tesfaye D Mekonnen H . Determinants of Stillbirth Among Women Deliveries at Amhara Region, Ethiopia. BMC Pregnancy Childbirth (2017) 17(1):375–7. 10.1186/s12884-017-1573-4
6.
Singh A . Sterilization Regret Among Married Women in India: Trends, Patterns and Correlates. Int Perspect Sex Reprod Health (2018) 44(4):167–76. 10.1363/44e7218
7.
Shekhar C Paswan B Singh A . Prevalence, Sociodemographic Determinants and Self-Reported Reasons for Hysterectomy in India. Reprod Health (2019) 16(1):118–6. 10.1186/s12978-019-0780-z
8.
Dandona R Pandey A Dandona L . A Review of National Health Surveys in India. Bull World Health Organ (2018) 94(4):286–96A. 10.2471/BLT.15.158493
9.
Rathi K Kamboj P Bansal PG Toteja GS . A Review of Selected Nutrition & Health Surveys in India. Indian J Med Res (2018) 148(5):596–611. 10.4103/ijmr.IJMR_1808_18
10.
Karvande S Sonawane D Chavan S Mistry N . What Does Quality of Care Mean for Maternal Health Providers from Two Vulnerable States of India? Case Study of Bihar and Jharkhand. J Health Popul Nutr (2016) 35(1):6–10. 10.1186/s41043-016-0043-3
11.
Chimankar DA Sahoo H . Factors Influencing the Utilization of Maternal Health Care Services in Uttarakhand. Stud Ethno-Medicine (2011) 5(3):209–16. 10.1080/09735070.2011.11886411
12.
Singh PK Rai RK Alagarajan M Singh L . Determinants of Maternity Care Services Utilization Among Married Adolescents in Rural India. PloS one (2012) 7(2):e31666. 10.1371/journal.pone.0031666
13.
Kavitha N . Are Young Mothers in India Deprived of Maternal Health Care Services? A Comparative Study of Urban and Rural Areas. J Health Manage (2015) 17(2):204–20. 10.1177/0972063415575809
14.
Singh KJ Kadian S Kaur A Saini K Kuchhal P Kashyap D et al Spatial Pattern of Maternal Health in Northeastern States, India: Evidence from National Family Health Survey 4 (2015-16. Asian Pac J Health Sci (2017) 4(2):147–56. 10.21276/apjhs.2017.4.2.25
15.
Tiwari R Gupta S . Spatial Inequalities in Maternal Health Care Utilization in Madhya Pradesh. J. Rural Dev. Rev. (2018) V(5).
16.
Ali B Debnath P Anwar T . Inequalities in Utilisation of Maternal Health Services in Urban India: Evidences from National Family Health Survey-4. Clin Epidemiol Glob Health (2021) 10:100672. 10.1016/j.cegh.2020.11.005
17.
Mohan D Bashingwa JJH Tiffin N Dhar D Mulder N George A et al Does Having a mobile Phone Matter? Linking Phone Access Among Women to Health in India: An Exploratory Analysis of the National Family Health Survey. PloS one (2020) 15(7):e0236078. 10.1371/journal.pone.0236078
18.
Mondal D Karmakar S Banerjee A . Women’s Autonomy and Utilization of Maternal Healthcare in India: Evidence from a Recent National Survey. PLoS One (2020) 15(12):e0243553. 10.1371/journal.pone.0243553
19.
Ghosh A Ghosh R . Maternal Health Care in India: A Reflection of 10 years of National Health Mission on the Indian Maternal Health Scenario. Sex Reprod Healthc (2020) 25:100530. 10.1016/j.srhc.2020.100530
20.
Ali B Dhillon P Mohanty SK . Inequalities in the Utilization of Maternal Health Care in the Pre-and post-National Health Mission Periods in India. J Biosoc Sci (2020) 52(2):198–212. 10.1017/S0021932019000385
21.
Yadav AK Sahni B Jena PK Kumar D Bala K . Trends, Differentials, and Social Determinants of Maternal Health Care Services Utilization in Rural India: An Analysis from Pooled Data. Womens Health Rep (2020) 1(1):179–89. 10.1089/whr.2019.0022
22.
Yadav AK Jena PK . Maternal Health Outcomes of Socially Marginalized Groups in India. Int J Health Care Qual Assur (2020) 33(2):172–188. 10.1108/IJHCQA-08-2018-0212
23.
Kumar C Rai RK Singh PK Singh L . Socioeconomic Disparities in Maternity Care Among Indian Adolescents, 1990–2006. PloS one (2013) 8(7):e69094. 10.1371/journal.pone.0069094
24.
Raj P Raj A . Caste Variations in Reproductive Health Status of Women: a Study of Three Eastern States. Sociological Bull (2004) 53(3):326–47. 10.1177/0038022920040302
25.
Govindasamy P Ramesh BM . Maternal Education and Utilization of Maternal and Child Health Services in India. National Family Health Survey Subject Reports (1997)
26.
Sivakami M Kulkarni PM . Are Socially and Economically Weaker Sections Deprived of Maternal Health Care in Tamil Nadu, India?J Health Popul Developing Countries (2003) 113.
27.
Navaneetham K Dharmalingam A . Utilization of Maternal Health Care Services in Southern India. Soc Sci Med (2002) 55(10):1849–69. 10.1016/S0277-9536(01)00313-6
28.
Chakrabarti A . Factors Governing Maternal Health Care Utilisation: Evidence from Rural India. Available at SSRN 389280 (2004). 10.2139/ssrn.389280
29.
Pandey A Roy N Sahu D Acharya R . Maternal Health Care Services: Observations from Chhattisgarh, Jharkhand and Uttaranchal. Econ Polit Wkly (2004) 39(4):713–20. 10.2307/4414646
30.
Raj P . Pregnancy Complications and Health-Seeking Behaviour Among Married Women in Uttar Pradesh, India. Res Pract Soc Sci (2005) 1(1):48.
31.
Anand S Sinha RK . Quality Differentials and Reproductive Health Service Utilisation Determinants in India. International Journal of Health Care Quality Assurance (2010). 10.1108/09526861011081859
32.
Ghosh S . Socio-economic Factors Influencing Utilisation of Maternal Health Care in Uttar Pradesh: An Analysis of NFHS-2 Data. Soc Change (2004) 34(4):61–73. 10.1177/004908570403400405
33.
Singh L Rai RK Singh PK . Assessing the Utilization of Maternal and Child Health Care Among Married Adolescent Women: Evidence from India. J Biosoc Sci (2012) 44:1, 10.1017/S0021932011000472
34.
Pradhan MR Patel SK Saraf AA . Informed Choice in Modern Contraceptive Method Use: Pattern and Predictors Among Young Women in India. J Biosoc Sci (2020) 52(6):846–59. 10.1017/S0021932019000828
35.
Sinha A Chattopadhyay A . Utilization of Maternal and Child Health Care Services in North and South India: Does Spousal Violence Matter?Int J Popul Stud (2016) 2(2):107–22. 10.18063/IJPS.2016.02.001
36.
Singh P Singh KK Singh P . Maternal Health Care Service Utilization Among Young Married Women in India, 1992–2016: Trends and Determinants. BMC Pregnancy Childbirth (2021) 21(1):122–13. 10.1186/s12884-021-03607-w
37.
Nagdeve D Bharati D . Urban-rural Differentials in Maternal and Child Health in Andhra Pradesh, India. Rural Remote Health (2003) 3(1):146. 10.22605/RRH146
38.
Arokiasamy P Pradhan J . Maternal Health Care in India: Access and Demand Determinants. Prim Health Care Res Dev (2013) 14(4):373–93. 10.1017/S1463423612000552
39.
Yadav J Kumar J Gautam S Yadav RJ . Differential in Utilization of Maternal Care Services in Empowered Action Group States, India (1990-2006). Indian J Community Health (2016) 28(1):19.
40.
Mishra US Ramanathan M . Delivery-related Complications and Determinants of Caesarean Section Rates in India. Health Policy Plan (2002) 17(1):90–8. 10.1093/heapol/17.1.90
41.
Thind A Mohani A Banerjee K Hagigi F . Where to Deliver? Analysis of Choice of Delivery Location from a National Survey in India. BMC public health (2008) 8(1): 29. 10.1186/1471-2458-8-29
42.
Srivastava S Chaurasia H Singh K Chaudhary P . Exploring the Spatial Patterns of Cesarean Section Delivery in India: Evidence from National Family Health Survey-4. Clin Epidemiol Glob Health (2020) 8(2):414–22. 10.1016/j.cegh.2019.09.012
43.
Roy N Mishra PK Mishra VK Chattu VK Varandani S Batham SK . Changing Scenario of C-Section Delivery in India: Understanding the Maternal Health Concern and its Associated Predictors. J Fam Med Prim CareCare (2021) 10(11):4182–8. 10.4103/jfmpc.jfmpc_585_21
44.
Shukla M Mohan M van Duinen A Gadgil A Bakker J Bhushan P et al Assessing Geographical and Economic Inequalities in Caesarean Section Rates between the Districts of Bihar, India: a Secondary Analysis of the National Family Health Survey. BMJ open (2022) 12(1): e055326. 10.1136/bmjopen-2021-055326
45.
Chakrabarti A Chaudhuri K . Antenatal and Maternal Health Care Utilization: Evidence from Northeastern States of India. Appl Econ (2007) 39(6):683–95. 10.1080/00036840500439036
46.
Pallikadavath S Foss M Stones RW . Antenatal Care: Provision and Inequality in Rural north India. Soc Sci Med (2004) 59(6):1147–58. 10.1016/j.socscimed.2003.11.045
47.
Rani M Harvey S . Differentials in the Quality of Antenatal Care in India. Int J Qual Health Care (2008) 20(1):62–71. 10.1093/intqhc/mzm052
48.
Rejoice PR Ravishankar AK . Differentials in Maternal Health Care Service Utilization: Comparative Study between Tamilnadu and Karnataka. World Appl Sci J (2011) 14:1661
49.
Dhawan D Pinnamaneni R Bekalu M Viswanath K . Association between Different Types of Mass media and Antenatal Care Visits in India: a Cross-Sectional Study from the National Family Health Survey (2015–2016). BMJ open (2020) 10(12):e042839. 10.1136/bmjopen-2020-042839
50.
Kumar G Choudhary TS Srivastava A Upadhyay RP Taneja S Bahl R et al Utilisation, Equity and Determinants of Full Antenatal Care in India: Analysis from the National Family Health Survey 4. BMC Pregnancy Childbirth (2019) 19(1):327–9. 10.1186/s12884-019-2473-6
51.
Chattopadhyay A Govil D . Men and Maternal Health Care Utilization in India and in Selected Less-Developed States: Evidence from a Large-Scale Survey 2015–16. J Biosoc Sci (2020) 53:724–44. 10.1017/S0021932020000498
52.
Patel R Gupta A Chauhan S Bansod DW . Effects of Sanitation Practices on Adverse Pregnancy Outcomes in India: a Conducive Finding from Recent Indian Demographic Health Survey. BMC Pregnancy Childbirth (2019) 19(1):378–12. 10.1186/s12884-019-2528-8
53.
Lee HY Oh J Kim R Subramanian SV . Long‐term Trend in Socioeconomic Inequalities and Geographic Variation in the Utilization of Antenatal Care Service in India between 1998 and 2015. Health Serv Res (2020) 55(3):419–31. 10.1111/1475-6773.13277
54.
Hazarika I . Factors that Determine the Use of Skilled Care during Delivery in India: Implications for Achievement of MDG-5 Targets. Matern Child Health J (2011) 15(8):1381–8. 10.1007/s10995-010-0687-3
55.
Prakash R Singh A Pathak PK Parasuraman S . Early Marriage, Poor Reproductive Health Status of Mother and Child Well-Being in India. J Fam Plann Reprod Health Care (2011) 37(3):136–45. 10.1136/jfprhc-2011-0080
56.
Kumar P Dhillon P . Structural Equation Modeling on the Relationship between Maternal Characteristics and Pregnancy Complications: A Study Based on National Family Health Survey. J Obstet Gynaecol Res (2021) 47(2):592–605. 10.1111/jog.14566
57.
Stephenson R Koenig MA Acharya R Roy TK . Domestic Violence, Contraceptive Use, and Unwanted Pregnancy in Rural India. Stud Fam Plann (2008) 39(3):177–86. 10.1111/j.1728-4465.2008.165.x
58.
Nguyen PH Scott S Neupane S Tran LM Menon P . Social, Biological, and Programmatic Factors Linking Adolescent Pregnancy and Early Childhood Undernutrition: a Path Analysis of India's 2016 National Family and Health Survey. Lancet Child Adolesc Health (2019) 3(7):463. 10.1016/S2352-4642(19)30110-5
59.
Dutta M Shekhar C Prashad L . Level, Trend and Correlates of Mistimed and Unwanted Pregnancies Among Currently Pregnant Ever Married Women in India. PLoS ONE (2015) 10(12):e0144400. 10.1371/journal.pone.0144400
60.
Raj A Saggurti N Balaiah D Silverman JG . Prevalence of Child Marriage and its Effect on Fertility and Fertility-Control Outcomes of Young Women in India: a Cross-Sectional, Observational Study. Lancet (2009) 373(9678):1883–9. 10.1016/S0140-6736(09)60246-4
61.
Singh R Tripathi V Singh K Ahuja RK Vani MK Dwivedi SN . Breastfeeding as a Time-varying-time-dependent Factor for Birth Spacing: Multivariate Models with Validations and Predictions. World Health Popul (2012) 13(3):28–51. 10.12927/whp.2012.22857
62.
Ravindran TS Mishra US . Unmet Need for Reproductive Health in India. Reprod Health Matters (2001) 9(18):105–13. 10.1016/S0968-8080(01)90097-7
63.
Saikia N Singh A . Does Type of Household Affect Maternal Health? Evidence from India. J Biosoc Sci (2009) 41(3):329–53. 10.1017/S0021932008003209
64.
Kulathinal S Säävälä M . Fertility Intentions and Early Life Health Stress Among Women in Eight Indian Cities: Testing the Reproductive Acceleration Hypothesis. J Biosoc Sci (2015) 47(5):632–49. 10.1017/S0021932014000261
65.
Chauhan BG Verma RK Alagarajan M Chauhan SK . Effect of Maternal Healthcare Utilization on Early Neonatal, Neonatal and Post-Neonatal Mortality in India. Community Health Equity Res Pol (2022) 43(1):31–43. 10.1177/0272684X211004925
66.
Paul PL . Male Partners' Role in Maternal Health Service Utilization : a Secondary Analysis Using 2015-16 National Family Health Survey (NFHS) Data. Midwifery (2022) 113:103423. 10.1016/j.midw.2022.103423
67.
Anis T Akram M . Maternal Health in India during Covid-19 : Major Issues and Challenges. Int J Appl (2022) 12(1):1–8. 10.5923/j.ijas.20221201.01
68.
Kulkarni R Begum S . A Critical Appraisal of NFHS-5 Data on Maternal Health Indicators: Trends and Implications for India. Indian Pract (2021) 74(2):23
69.
Ali B Chauhan S . Inequalities in the Utilisation of Maternal Health Care in Rural India: Evidences from National Family Health Survey III & IV. BMC Public Health (2020) 20(1):369–13. 10.1186/s12889-020-08480-4
70.
Mishra PS Veerapandian K Choudhary PK . Impact of Socio-Economic Inequity in Access to Maternal Health Benefits in India: Evidence from Janani Suraksha Yojana Using NFHS Data. Plos one (2021) 16(3):e0247935. 10.1371/journal.pone.0247935
71.
Debsarma D Karmakar R Saha J . Trends and Determinants in the Utilization of Maternal Healthcare Services in West Bengal, India: Findings from the 3rd and 4th Round National Family and Health Survey. Midwifery (2022) 112:103387. 10.1016/j.midw.2022.103387
72.
Mojoyinola JK . Influence of Maternal Health Literacy on Healthy Pregnancy and Pregnancy Outcomes of Women Attending Public Hospitals in Ibadan, Oyo State, Nigeria. Afr Res Rev (2011) 5(3). 10.4314/afrrev.v5i3.67336
Summary
Keywords
maternal health, systematic review, women, India, National Family Health Survey
Citation
Raj P and Gupta N (2022) A Review of the National Family Health Survey Data in Addressing India’s Maternal Health Situation. Public Health Rev 43:1604825. doi: 10.3389/phrs.2022.1604825
Received
06 February 2022
Accepted
17 October 2022
Published
31 October 2022
Volume
43 - 2022
Edited by
Rajesh Kumar Rai, Society for Health and Demographic Surveillance, India
Reviewed by
Prashant Kumar Singh, ICMR-National Institute of Cancer Prevention and Research, India
Updates
Copyright
© 2022 Raj and Gupta.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms. PHR is edited by the Swiss School of Public Health (SSPH+) in a partnership with the Association of Schools of Public Health of the European Region (ASPHER)+
*Correspondence: Papia Raj, papia.raj@gmail.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.