- 1Faculty of Allied Health and Social Care, Anglia Ruskin University, Cambridge, United Kingdom
- 2Centre for Applied Health and Social Care Research, Sheffield Hallam University, Sheffield, United Kingdom
- 3Division of Health Research, Centre for Ageing Research, Lancaster University, Lancaster, United Kingdom
- 4Department of Psychology, School of Social Sciences, Heriot-Watt University, Edinburgh, United Kingdom
- 5Faculty of Social Science & Health, Durham University, Durham, United Kingdom
Cognitive frailty (CF) is defined as the clinical syndrome of the combination of physical frailty and cognitive impairment, without dementia. Numerous risk factors for CF have been previously identified but this scoping review focusses on the critical need for social engagement and the association with cognition. The focus of this scoping review on the opportunity for social engagement rather than on perception or experience of loneliness. Based on the results of 55 studies were synthesised into four social engagement categories, namely participation, household, network, and habitat. Social engagement is associated with maintaining or improving cognition, particularly through active participation in social roles. Habitat (i.e., rural or urban settings) also influences cognition and the challenge is to enable social participation.
Introduction
CF is defined as the conjunction of physical frailty with cognitive impairment but without dementia [1]. Mild cognitive impairment (MCI) has been widely conceptualized as an intermediate phase between cognitive ageing and overt dementia [2]. CF is a phenomenon of older adult population health and may affect 1.0%–12% community-dwelling older adults [3]. CF is differentiated from MCI because it is not necessarily an intermediate stage between normal ageing and dementia and is a potentially reversible condition [3] but can represent deficits including depression, decreased function, social and physical frailty [4].
Behavioural risk factors are common to MCI and CF, including prolonged sedentary behaviours, inactivity, and manifest alongside diabetes and neurological disorders [5, 6]. The Cochrane review, “Prevention of Dementia and Cognitive Decline” [7] suggests that sustained implementation of multi-modal interventions would have a preventative impact at population level, but considerable research is needed to evidence the best diet [8], exercise [9] and prevention strategies [10]. The association between cognitive and physical decline interact [11], resulting in slower cognitive processing speed along with reduced walking speed and grip strength [12].
The World Health Organisation (WHO) Age friendly environments strategy recognises that the loss of physical and cognitive function may relate to environment and reflect limited opportunities for older adults to participate at a community level, where there are inadequate facilities or municipal services [13]. The UN General Assembly declared 2021–2030 highlighted the importance for policymakers to improve the lives of older people [14]. Global variation in expected community participation is reflected in cultural norms for older lifestyles. Intergenerational households may not mitigate cognitive changes, in spite of assumed benefits to safety and company [15]. A consideration of the environmental factors alongside more recognised behavioural/lifestyle interventions is well justified [16].
Targeting health inequalities in relation to CF and identifying environmental risks is important and necessary to achieve the required public health response at community or societal level. CF varies across demographic, social and economic groups in the older adult population and indeed there is considerable variation in reporting of morbidity [14]. Where social activities are well established in communities, they provide instrumental and/or emotional support [17]. Safe and high-quality amenities; inclusive spaces in the neighbourhood may be a requisite factor in enabling social participation [18]. Social engagement has been defined as “the maintenance of social connections and participation in social activities” [19], but it has also been used as an umbrella concept for the variety of components of an individual’s social behaviour and social structure [20]. Older populations are particularly affected by the availability of social activities and pursuits, with variation in cognitive ageing recognised as an outcome [10]. The decline in cognitive health is associated with lower socio-economic status [21]. Both racial and economic disparities also intensify barriers to engagement for more marginalised older people [22].
Compared to previous generations, older adults in democracies with market-based economies (Organization for Economic Co-operation and Development- OECD countries) are active, healthier, wealthier and educated [23]. Networks of family and friends are a source of support and are generally associated with higher life satisfaction values [24] but older adults are also more often single and childless. Factoring in retirement or age-related losses (e.g., death of a partner or friends), along with declining health and increasing mobility limitations, it is more common for older adults to live in relative isolation [25].
The aim of this study was to scope the literature to identify associations between social engagement and cognitive frailty. The review was selected to clarify concepts and make a preliminary assessment of how different contexts and demographic factors related to cognitive frailty.
Methods
This scoping review follows the guidelines by Arksey and O’Malley [26] that recommend a broad search of the literature on a specific topic which can then be subject to consultation and become useful to policymakers, practitioners, and service users. The research question was “what impact does social engagement have on older adult cognitive frailty?” and searches were undertaken using a specific limited database search that identified relevant studies.
Scopus was selected as a single database based on pragmatic need to complete the study within a timeframe and evidence an inclusive cross-disciplinary literature [27]. The terms cogniti* AND resilience AND “social engagement” and cogniti* AND ageing AND “social engagement” were searched. Scopus pilot searches resulted in the decision to exclude the term “frailty” as they resulted in many findings on physical frailty only (even when including cogniti*) and often did not touch on cognitive decline or impairment. The focus on cogniti* was most useful and enabled review of the findings for age groups/older adults and cognitive frailty in the title and abstract screenings.
The study selection involved i) removing duplicates, ii) title screenings and iii) abstract screening, and using inclusion and exclusion criteria to identify the final selection of studies. Inclusion: the impact of social engagement on cognition, referenced older adults, or reported on observational data or longitudinal cohort investigations, in English. Exclusion: focus solely on physical frailty or dementia, books, reviews and commentaries and if they were associated with lifestyle or behaviour change interventions or particular therapeutic methods that are used to enhance individual capabilities in either healthy or diseased populations.
As suggested by Arksey and O’Malley [26], coding and charting was used to identify multiple types of social engagement, and these were collated into categories which summarised different social environments. Charting was used to synthesise and interpret the coded data into themes according to Ritchie and Spencer’s method in framework analysis [28]. Charting involved sifting and sorting coded texts according to key issues and themes. This was undertaken using the software package Quirkos, that is commonly used in qualitative inquiry, and which allowed the collation and summarising of results. Data regarding the type of study, country, main findings, and type of social engagement were extracted from the papers. The data categories also related to the demographic features of gender and socio-economic status. The outcome is the categorisation of the literature associated with social environments that enable engagement or inhibit social engagement for older adults.
Results
Overall, 6,296 titles were found in the literature, of which 6,100 were excluded after the title screening. The title and abstract screenings were undertaken by CB and SFD. The abstracts of the remaining 196 studies were screened using the same inclusion criteria, at which point a further 141 were excluded leaving 55 studies included in the analysis. All studies were quantitative. The PRISMA diagram (see Figure 1) identifies the outcome of screening and selection of papers.
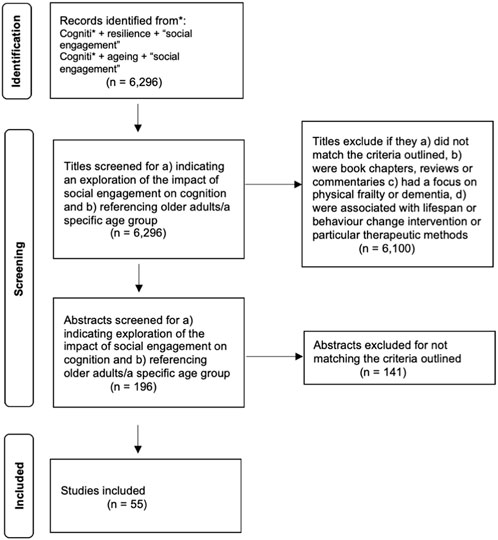
FIGURE 1. PRISMA Diagram [29] (2023, UK).
Framework Analysis
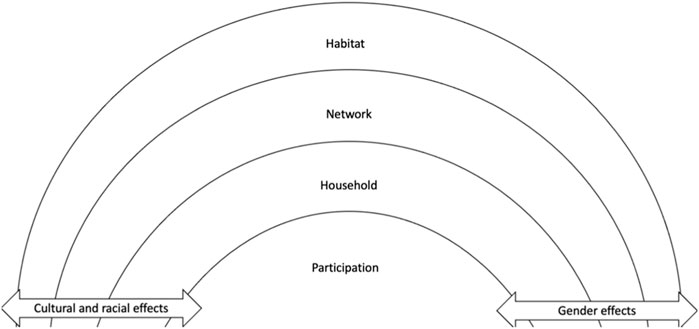
Four categories were derived from the analysis of collated papers, with some papers reporting results on more than one category [28]. The intention was to differentiate the opportunities for sustained social engagement and cognitive resilience or risk of cognitive decline, as indicated in the outcomes for different groups of older adults. The named categories suggest different context in which older people achieve social engagement and the relative effects on cognitive frailty. These can be defined as follows:
• Participation refers to participant’s use of community based social activities and the impact this has on cognitive frailty; 22 papers.
• Household refers to the immediate living situation and ‘home’ circumstances of an individual; 12 papers.
• Network refers to the characteristics of the network in which an individual operates such as its diversity, frequency of contacts, complexity, and size; 26 papers.
• Habitat, includes the wider neighbourhood for example, urban or rural context as a place of residence; six papers.
The tables selected for analysis are charted in Table 1. This provides information about which category the study falls in as well as the country of origin and type of study.
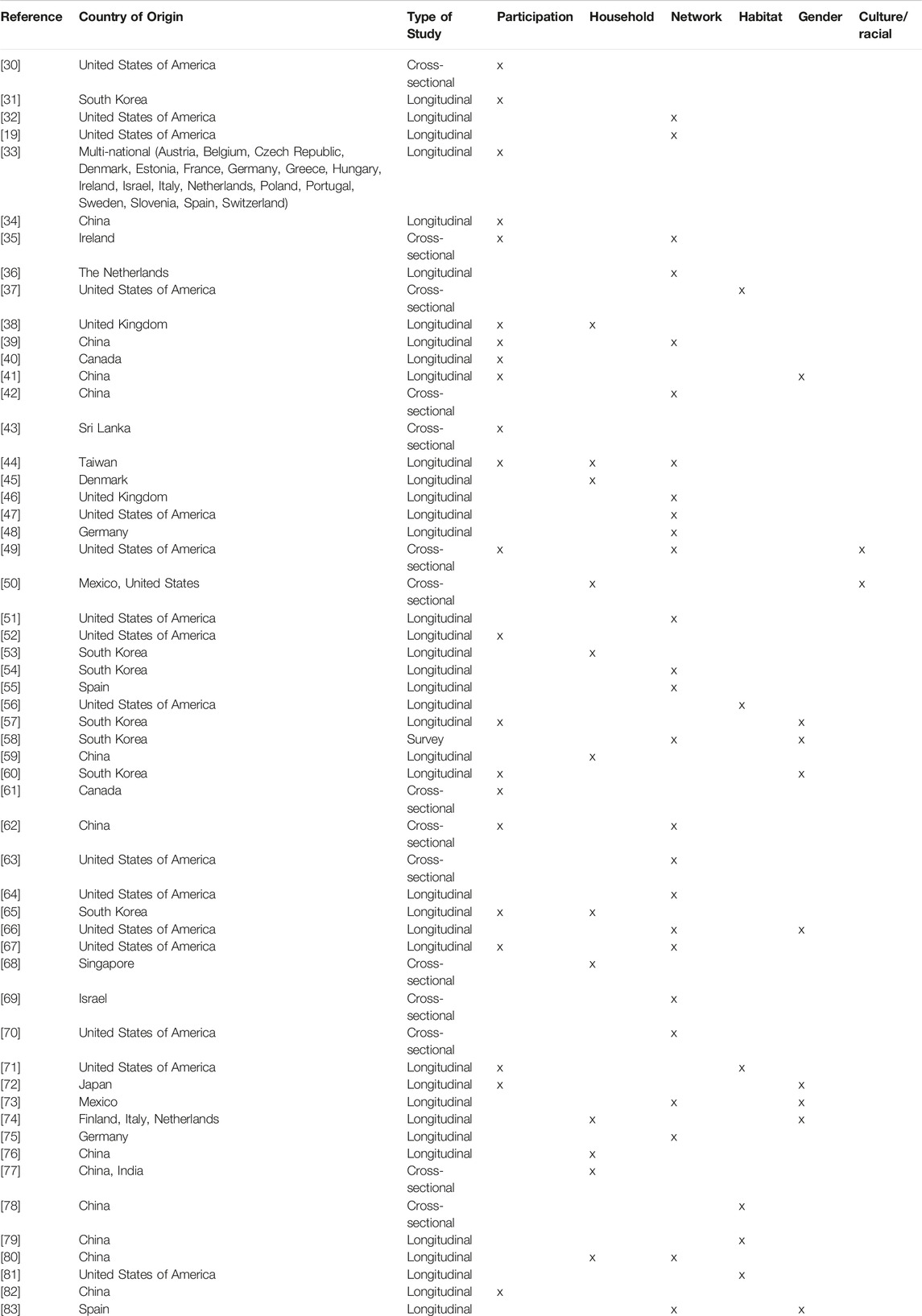
TABLE 1. Scoping review, cognitive frailty and social environment, country of origin, type of study and study categorisation (2023, UK).
Some evidence suggests that the social categories influence each other and that categories are not mutually exclusive in their effect on an individual [79]. But the differentiated contexts demonstrate how different environmental circumstances mediate opportunities and limitations to social engagement and enable and sustain cognitive health. The findings are in four categories and discussed below but there are some clear overarching benefits to older adults who manage to sustain social engagement. Social functioning is positively related to an initial level of cognitive function and a reduced rate of cognitive decline [32]. Social engagement protected against cognitive decline [40], and memory and executive function was predicted by social participation [33]. Conversely, not engaging socially had a negative impact on cognition. Social disengagement predicted the risk of cognitive decline in older individuals [83], and boredom from a lack of social engagement was associated with reduced cognitive function [35]. Further, demographic characteristics such as gender and culture intersect with environment or context [74].
Participation
Participating in social activity, whether of religious or leisurely nature, including hobby and sport groups, had a positive association with cognitive functioning [34, 41, 43, 57, 67, 61 and 84]. One study specifically found that the rate of global cognitive (calculated based on a test battery that included episodic memory, semantic memory, working memory, perceptual speed and visuospatial ability) decline was reduced by 70% for those frequently active compared to those infrequently active [52, 39]. Participation in one or two social activities improved performance on cognitive tasks compared to those who participated in no social activities, and, if this was increased to three or more activities per week, they performed even better [44]. Maintaining a socially-active lifestyle enhanced cognitive reserve and benefitted cognitive function [38]. A change from no social participation to more variety in social participation was associated with improvements in cognitive function [85]. Engagement in more social activities was associated with better baseline cognitive function, though this effect disappeared over time [86].
Conversely, little participation in group activities was related with cognitive impairment [62], not being part of a senior centre was associated with decreased cognitive function [65], and infrequent participation, poor social connections and social disengagement predicted the risk of cognitive decline in older individuals [83]. Additionally, participants were found to be at higher odds for self-diagnosed memory problems if they had low cultural participation and low social engagement [30]. Thus, there is consistent evidence that participating in socially engaging activities has a positive association with cognitive functioning for the individual.
Household
Marriage, co-habitation and home-based relationships and the loss of relationships appears to be contested and strongly influenced by gender. Living alone was not associated with poorer cognitive function at baseline and follow-up [38]. In line with this, older adults who transitioned to living alone (due to death of or divorce from spouse) had a lower risk of cognitive impairment, compared to those who continued to live with others [59]. However, men who lived alone in old age were twice as likely to experience cognitive decline compared to those married or living with someone [74], (see detail on gender influence below). Living arrangements were found to be one of the factors more strongly associated with cognitive ability in older people [45]. Older people living in multigenerational family household often had poorer cognitive function than those living with a spouse or non-relatives [59]. Data collected in Taiwan found that social participation outside the family may have a larger effect on cognition than the social contracts within the family [44, 68]. While individuals did experience more isolation from family and more loneliness than those living with others, they were often more engaged in social activities.
Being married or the presence of a partner may also affect cognition. Unmarried individuals had lower cognitive function than married individuals [76], and married participants experienced less cognitive decline [46]. Never married or divorced individuals were more disadvantaged compared to married individuals when it came to cognitive health [53]. During a nine-year follow-up, married participants had a 16% lower risk of developing cognitive impairment compared to those widowed; however when controlled for all types of social support this was no longer significant [80]. Older, single Chinese men had poorer cognitive function compared to those married, an association not found in women [77]. Another study reported that marital status was also a significant predictor of cognitive ability in women [65].
Network
There seems to be clear evidence that a diverse or complex social network has a positive association with cognition. A diverse social network lowered the risk of cognitive decline and promoted health and survival [54]. Some evidence suggested that enhanced complexity had a buffering effect on cognitive decline [36]. Good quality social networks seem to protect against cognitive decline [63], and a higher number of networks had a positive correlation with initial cognitive function and reduced rate of cognitive decline [32].
The characteristics of the networks and their relative value to an individual seem to influence cognitive functioning. Generally speaking, having an ‘adequate’ network was associated with less cognitive impairment [62], a lower risk of cognitive decline [39], and structural elements (being married/partnered, the number of social networks and contact frequency) and functional elements (support, strain, loneliness) were associated with episodic memory [51]. However, the results regarding network size are mixed. While one study found worse perceptual speed associated with larger social networks [67], another reported that a larger network was associated with better perceptual speed and verbal fluency [75]. Individuals with no social ties were at increased risk of cognitive decline compared to those with five or six social ties [19]. Some studies also found no effect of network size on cognition [64].
The association of cognition with presence of family in an individual’s social network provided mixed results. One study found that a higher frequency of visual contact with family was associated with a lower probability of cognitive decline [83], but other studies found that relationships with family [42] and children’s visits [80] could be associated with an increased risk of cognitive impairment. Social participation outside the family network may have a larger impact on cognitive function [52], and networks with a greater proportion of friends were associated with better global cognition compared to those with a greater proportion of family [70].
More frequent contact with networks seems to have positive association with cognition [39, 69]. Alternatively, not being in a social network and experiencing social isolation a generally been to have a negative association with cognitive functioning [47, 48 and 55]. Loneliness associated with social isolation had also consistently been linked to lower cognitive functioning [46, 55], though one study reported it to be associated with better semantic memory [67].
Habitat
One study explored how living in rural or urban places, as well as migration, influences cognition in Chinese and Indian samples [87]. For women, living in rural areas or migrating from rural-to-rural areas was associated with poorer cognition in both samples. For men in China, rural residents had worse cognitive functioning than urban residents, and those who migrated from an urban area to another urban area had the highest cognitive scores. In India, men had the poorest cognition in the migrated rural-to-rural sample. Women were consistently affected worse by migration in terms of cognitive function, compared to men, in both countries. Living in a town was associated with worse cognitive function than living in a city, and living rurally was associated with worse cognition than living in a town [79]. However, it is important to note that the characteristics of cities, towns and rural areas will differ widely between countries and these findings will not necessarily translate to all countries.
Neighbourhood characteristics also have an impact on cognition. Older Hispanic/Latina women living in a neighbourhood with the lowest perceived problems had higher global cognition and memory [37]. In the study, high perceived social cohesion in the neighbourhoods was associated with lower global cognition, as well lower verbal learning, verbal fluency and processing speed. No association between men and any perceived neighbourhood characteristics were found. Other research found that living in a cohesive neighbourhood promoted social activities and through this benefited cognitive function [86]. Neighbourhood social cohesion was also independently associated with most domains of cognitive function [81].
Other Factors Associated With Cognition
The research evidence suggests that the different categories intersect and even contradict one another. For example, living in a cohesive neighbourhood promotes social activities and therefore benefits cognitive function, suggesting that habitat level has an influence on social participation [86]. Similarly, poor housing conditions had a negative impact on cognition because a place of residence mediates social participation [79]. A small social network also limits participation [56] although living alone can be advantageous where enabled by cultural cohesion and social activity beyond the family that builds cognitive reserve [38].
Experiencing a loss, and the connected psychological effect, has been associated with a modest decline in cognitive function [50] and loneliness is associated with network [34, 67 and 84] and household [43]. Another study found that, while loneliness is associated with aspects of cognitive ability, symptoms of depression account for this association [61], suggesting that presence of depression symptoms may be more significant for cognition than loneliness.
Gender Differences
The impact of social engagement, as well as the type of social engagement and its connection to cognition, seemed to differ between genders, though the research is not yet conclusive. One study found that volunteering significantly aids cognitive functioning in women but not in men [41]. While religious group activities were found to be beneficial for women but not men, an inability to work was detrimental to men’s cognition but not for women [57]. Additionally, social activities were likely to maintain good cognitive functioning in older age for men, and for women with lower education, social engagement particularly protected against cognitive decline [60]. Another study found that men in neighbourhood associations and local events groups and women engaged in hobby and volunteer groups experienced less cognitive decline [72].
Women’s cognition was influenced by the number of members they considered friends [58], and their engagement with friends was protective against cognitive decline [83]; this was not found in men [83]. For men, high perceived support at baseline was associated with increased risk of cognitive impairment, an effect not found in women [66]. Additionally, for women who remained in Mexico while their children emigrated to the US, this led to a stronger decline in overall cognitive performance whereas there was no impact on men [73].
As mentioned above, men who lost a partner, were unmarried or started to live alone in old age had at least two times subsequent stronger cognitive decline compared to those married or living with someone [74].
Racial and Cultural Differences
Racial and cultural demographics and differences also impact cognitive decline. Cultural effects of social participation were also found where social participation was positively associated with memory in non-Hispanic White peoples but not in non-Hispanic Black peoples [49]. This may suggest some cultural groups are less likely to participate in enough social activity to yield cognitive benefits.
Cultural and gender effects were also found when it came to comparing the cognition of wives in Mexico and the United States. In Mexico, the wives’ social engagement benefited their own cognitive function, as well as their husbands, and this effect was found this direction only. In the United States, no effects of one’s spouse engagement were found, from which the authors suggest that if there is a more traditional social role of women there might be more co-dependency within the couple [50].
Strengths and Limitations
This study used a single search engine to scope a vast literature and categorise environmental factors that promote social engagement. It does not reflect the literature related to loneliness as a key indicator of cognitive frailty. Loneliness as a personal psychological phenomenon has been widely studied and the negative effects on cognitive health and wellbeing are associated not with isolation but rather the perception of being alone.
Similarly, this scoping review does not address historic socio-environmental factors. For example, some evidence suggests that childhood connections have an impact on cognition in later life, with adverse childhood events and negative friendship experiences significantly associated with lower initial cognitive status and the rate of decline in cognitive functioning [52].
The search did not specifically include “frailty” for reasons described in the methods section. The inclusion of English only studies presents a risk of a dominant Eurocentric view in spite of international cohorts included and analysed.
Discussion
There are multiple correlates of cognitive ability level and change in later life, many of which have small effects [88]. But a cumulative effect of small environmental improvements in old age may significantly mitigate the negative effects of sparse social contact without necessitating complex social or lifestyle behaviour change interventions that are difficult and costly to deliver through services [89].
An initial framework for considering the factors that mitigate the risks to cognitive decline in very limited social environments is represented in Figure 2. It may offer a useful way to think about and promote an approach to planning more socially enabling environments, particularly for those in the most deprived and vulnerable communities.
WHO use the term “participation” within the International Classification of Functioning (ICF) as a person’s involvement in a life situation and involves engagement in life roles, such as employment, education, or relationships [Disability and Health Overview | CDC]. It is suggested that technology, support and relationships, services, policies, or the beliefs of others all reflect in participation achieved within an environment. The environment informs and sometimes compensates for individual characteristics including municipal or household measures to compensate for ageing.
This evidence suggests that the presence of family support (for example, personal care in a multigenerational family home) is insufficient to prevent cognitive decline. The studies undertaken in Asia, where family care is more pervasive demonstrates that care, in and of itself does not prevent cognitive frailty [53]. The absence of friendship, engagement beyond an immediate family group and the inability to participate with neighbours, acquaintances and in group activities can be a cause or a consequence of cognitive decline and may have a causal relationship in older adult populations.
There are cross-cutting drivers associated with environmental factors including gender effects; men appear to be more specifically affected by community and household isolation, irrespective of household, providing there is access to external social networks [76, 48]. In addition, cultural differences, particularly associated with the global diversity of the literature can be seen, with different norms in relation to expectations of families to offer care and support for older relatives. The absence of information about the effects of migration, multi-cultural neighbourhoods and the impact on social networks is evident, with this being a much more pervasive situation in poorer communities and requiring specific development at community level.
The presence or absence of an “anchor organisation” (church communities, charity and third sector organisations) at community level, may be important to address local participation, and facilitate population health and wellbeing. These organisations operate in neighbours with specific knowledge of critical cultural factors, enabling local areas to challenge the difficulties associated with social isolation. Cognitive frailty may be particularly prone to social avoidance, if safety, comfort and practical requirements are inadequate and fail to compensate for personal disability [90]. Further investigation is needed into the likelihood of cognitive frailty given cognitive decline [91].
Conclusions
This review investigated how older people experience cognitive outcomes in relation to context. The analysis presents a complex and diverse range of influences on cognitive health and frailty.
The paper demonstrates that contextual factors should be a consideration for older people and that there is a need to address vulnerability to pervasive cognitive frailty due to isolation and sub-optimal opportunities for social connection and engagement.
Interventions that constitute a community-based prevention strategy for those at risk may be indicated. Health and social care commissioners and town planners may consider cognitive frailty as a specific population health risk and apply wide-ranging asset-based development programmes to enable communities to address the critical needs across neighbourhoods.
Funded and conceived of within the Cognitive Frailty Network (CFIN), the project aligns to further investigations of air quality and access to green space that are also associated with risks to cognitive decline in older adults.
Author Contributions
CB data sourcing and management and drafting. CH Drafting paper and review of data. CC Drafting paper and review of data. AG Drafting paper and review of data. SF Conceptualisation, data analysis and supervision. All authors contributed to the article and approved the submitted version.
Funding
This project was part funded and initiated through an international transdisciplinary network funded by BBSRC/MRC RCUK namely, Harnessing knowledge of lifespan biological, health, environmental and psychosocial mechanisms of cognitive frailty for integrated interventions as part of the UK ageing network (UKAN Network - UKAN (ukanet.org.uk)). Grant number grant number: BB/W018322/1.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
References
1. Kelaiditi, E, Cesari, M, Canevelli, M, van Kan, GA, Ousset, PJ, Gillette-Guyonnet, S, et al. Cognitive Frailty: Rational and Definition From an (I.A.N.A./I.A.G.G.) International Consensus Group. J Nutr Health Aging (2013) 17:726–34. doi:10.1007/s12603-013-0367-2
2. Winblad, B, Palmer, K, Kivipelto, M, Jelic, V, Fratiglioni, L, Wahlund, L-O, et al. Mild Cognitive Impairment--Beyond Controversies, Towards a Consensus: Report of the International Working Group on Mild Cognitive Impairment. J Intern Med (2004) 256:240–6. doi:10.1111/j.1365-2796.2004.01380.x
3. Sugimoto, T, Sakurai, T, Ono, R, Kimura, A, Saji, N, Niida, S, et al. Epidemiological and Clinical Significance of Cognitive Frailty: A Mini Review. Ageing Res Rev (2018) 44:1–7. doi:10.1016/j.arr.2018.03.002
4. Garner, IW, Burgess, AP, and Holland, CA. Developing and Validating the Community-Oriented Frailty Index (COM-FI). Arch Gerontol Geriatr (2020) 91:104232. doi:10.1016/j.archger.2020.104232
5. Lu, Y, Liu, C, Fawkes, S, Wang, Z, and Yu, D. Knowledge, Attitudes, and Practice of General Practitioners Toward Community Detection and Management of Mild Cognitive Impairment: A Cross-Sectional Study in Shanghai, China. BMC Prim Care (2022) 23:114. doi:10.1186/s12875-022-01716-9
6. Vatanabe, IP, Pedroso, RV, Teles, RHG, Ribeiro, JC, Manzine, PR, Pott-Junior, H, et al. A Systematic Review and Meta-Analysis on Cognitive Frailty in Community-Dwelling Older Adults: Risk and Associated Factors. Aging Ment Health (2022) 26:464–76. doi:10.1080/13607863.2021.1884844
7. Hafdi, M, Hoevenaar-Blom, MP, and Richard, E. Multi-Domain Interventions for the Prevention of Dementia and Cognitive Decline. Cochrane Database Syst Rev (2021) 11:CD013572. doi:10.1002/14651858.CD013572.pub2
8. Dalile, B, Kim, C, Challinor, A, Geurts, L, Gibney, ER, Galdos, MV, et al. The EAT-Lancet Reference Diet and Cognitive Function Across the Life Course. Lancet Planet Health (2022) 6:e749–e759. doi:10.1016/S2542-5196(22)00123-1
9. Theou, O, Stathokostas, L, Roland, KP, Jakobi, JM, Patterson, C, Vandervoort, AA, et al. The Effectiveness of Exercise Interventions for the Management of Frailty: A Systematic Review. J Aging Res (2011) 2011:569194. doi:10.4061/2011/569194
10. Miquel, S, Champ, C, Day, J, Aarts, E, Bahr, BA, Bakker, M, et al. Poor Cognitive Ageing: Vulnerabilities, Mechanisms and the Impact of Nutritional Interventions. Ageing Res Rev (2018) 42:40–55. doi:10.1016/j.arr.2017.12.004
11. Malmstrom, TK, and Morley, JE. Frailty and Cognition: Linking Two Common Syndromes in Older Persons. J Nutr Health Aging (2013) 17:723–5. doi:10.1007/s12603-013-0395-y
12. Starr, JM, and Deary, IJ. Socio-Economic Position Predicts Grip Strength and its Decline Between 79 and 87 Years: The Lothian Birth Cohort 1921. Age Ageing (2011) 40:749–52. doi:10.1093/ageing/afr070
13. WHO. Age-Friendly Environments (2024). Available from: https://www.who.int/teams/social-determinants-of-health/demographic-change-and-healthy-ageing/age-friendly-environments (Accessed January 5, 2023).
14. Chen, X, Giles, J, Yao, Y, Yip, W, Meng, Q, Berkman, L, et al. The Path to Healthy Ageing in China: A Peking University-Lancet Commission. Lancet Lond Engl (2022) 400:1967–2006. doi:10.1016/S0140-6736(22)01546-X
15. Krzeczkowska, A, Spalding, DM, McGeown, WJ, Gow, AJ, Carlson, MC, and Nicholls, LAB. A Systematic Review of the Impacts of Intergenerational Engagement on Older Adults’ Cognitive, Social, and Health Outcomes. Ageing Res Rev (2021) 71:101400. doi:10.1016/j.arr.2021.101400
16. Gow, AJ. Opportunities for Enhancing Brain Health Across the Lifespan. BJPsych Adv (2022) 28:102–111. doi:10.1192/bja.2021.26
17. Seeman, TE, and Berkman, LF. Structural Characteristics of Social Networks and Their Relationship With Social Support in the Elderly: Who Provides Support. Soc Sci Med (1988) 26:737–49. doi:10.1016/0277-9536(88)90065-2
18. Kemperman, A, van den Berg, P, Weijs-Perrée, M, and Uijtdewillegen, K. Loneliness of Older Adults: Social Network and the Living Environment. Int J Environ Res Public Health (2019) 16:406. doi:10.3390/ijerph16030406
19. Bassuk, SS, Glass, TA, and Berkman, LF. Social Disengagement and Incident Cognitive Decline in Community- Dwelling Elderly Persons. Ann Intern Med (1999) 131:165–73. doi:10.7326/0003-4819-131-3-199908030-00002
20. Mendes de Leon, CF. Social Engagement and Successful Aging. Eur J Ageing (2005) 2:64–6. doi:10.1007/s10433-005-0020-y
21. Deary, IJ, Johnson, W, Gow, AJ, Pattie, A, Brett, CE, Bates, TC, et al. Losing One’s Grip: A Bivariate Growth Curve Model of Grip Strength and Nonverbal Reasoning From Age 79 to 87 Years in the Lothian Birth Cohort 1921. J Gerontol B Psychol Sci Soc Sci (2011) 66:699–707. doi:10.1093/geronb/gbr059
22. Gauthier, GR, Smith, JA, García, C, Garcia, MA, and Thomas, PA. Exacerbating Inequalities: Social Networks, Racial/Ethnic Disparities, and the COVID-19 Pandemic in the United States. J Gerontol B Psychol Sci Soc Sci (2020) 76:e88–e92. doi:10.1093/geronb/gbaa117
23. Patterson, I. Baby Boomers and Adventure Tourism: The Importance of Marketing the Leisure Experience. World Leis J (2002) 44:4–10. doi:10.1080/04419057.2002.9674265
24. Tomini, F, Tomini, SM, and Groot, W. Understanding the Value of Social Networks in Life Satisfaction of Elderly People: A Comparative Study of 16 European Countries Using SHARE Data. BMC Geriatr (2016) 16:203. doi:10.1186/s12877-016-0362-7
25. Pino, L, González-Vélez, AE, Prieto-Flores, M-E, Ayala, A, Fernandez-Mayoralas, G, Rojo-Perez, F, et al. Self-Perceived Health and Quality of Life by Activity Status in Community-Dwelling Older Adults. Geriatr Gerontol Int (2014) 14:464–73. doi:10.1111/ggi.12119
26. Arksey, H, and O’Malley, L. Scoping Studies: Towards a Methodological Framework. Int J Soc Res Methodol (2005) 8:19–32. doi:10.1080/1364557032000119616
27. Harzing, AW, and Alakangas, S. Google Scholar, Scopus and the Web of Science: A Longitudinal and Cross-Disciplinary Comparison. Scientometrics (2016) 106:787–804. doi:10.1007/s11192-015-1798-9
28. Ritchie, J, and Spencer, L. Qualitative Data Analysis for Applied Policy Research. In: A Bryman, and R Burgess, editors. Analyzing Qualitative Data. London: Routledge (1994). ISBN 978-0-203-41308-1.
29. McGowan, J, Straus, S, Moher, D, Langlois, EV, O'Brien, KK, Horsley, T, et al. Reporting Scoping Reviews—PRISMA ScR Extension. J Clin Epidemiol (2020) 123:177–9. doi:10.1016/j.jclinepi.2020.03.016
30. Adamsen, C, Manson, SM, and Jiang, L. The Association of Cultural Participation and Social Engagement With Self-Reported Diagnosis of Memory Problems Among American Indian and Alaska Native Elders. J Aging Health (2021) 33:60S–67S. doi:10.1177/08982643211014971
31. Bae, SM. The Mediating Effect of Physical Function Decline on the Association Between Social Activity and Cognitive Function in Middle and Older Korean Adults: Analyzing Ten Years of Data Through Multivariate Latent Growth Modeling. Front Psychol (2020) 11. doi:10.3389/fpsyg.2020.02008
32. Barnes, LL, Mendes De Leon, CF, Wilson, RS, Bienias, JL, and Evans, DA. Social Resources and Cognitive Decline in a Population of Older African Americans and Whites. Neurology (2004) 63:2322–6. doi:10.1212/01.WNL.0000147473.04043.B3
33. Bourassa, KJ, Memel, M, Woolverton, C, and Sbarra, DA. Social Participation Predicts Cognitive Functioning in Aging Adults Over Time: Comparisons With Physical Health, Depression, and Physical Activity. Aging Ment Health (2017) 21:133–46. doi:10.1080/13607863.2015.1081152
34. Cai, S. Does Social Participation Improve Cognitive Abilities of the Elderly? J Popul Econ (2022) 35:591–619. doi:10.1007/s00148-020-00817-y
35. Conroy, RM, Golden, J, Jeffares, I, O’Neill, D, and McGee, H. Boredom-Proneness, Loneliness, Social Engagement and Depression and Their Association With Cognitive Function in Older People: A Population Study. Psychol Health Med (2010) 15:463–73. doi:10.1080/13548506.2010.487103
36. Ellwardt, L, Van Tilburg, TG, and Aartsen, MJ. The Mix Matters: Complex Personal Networks Relate to Higher Cognitive Functioning in Old Age. Soc Sci Med (2015) 125:107–15. doi:10.1016/j.socscimed.2014.05.007
37. Estrella, ML, Durazo-Arvizu, RA, Gallo, LC, Isasi, CR, Perreira, KM, Vu, T-HT, et al. Associations Between Perceived Neighborhood Environment and Cognitive Function Among Middle-Aged and Older Women and Men: Hispanic Community Health Study/Study of Latinos Sociocultural Ancillary Study. Soc Psychiatry Psychiatr Epidemiol (2020) 55:685–96. doi:10.1007/s00127-019-01829-0
38. Evans, IEM, Llewellyn, DJ, Matthews, FE, Woods, RT, Brayne, C, Clare, L, et al. Social Isolation, Cognitive Reserve, and Cognition in Healthy Older People. PLoS ONE (2019) 13:e0201008. doi:10.1371/journal.pone.0201008
39. Fan, Z, Lv, X, Tu, L, Zhang, M, Yu, X, and Wang, H. Reduced Social Activities and Networks, But Not Social Support, Are Associated With Cognitive Decline Among Older Chinese Adults: A Prospective Study. Soc Sci Med (2021) 289:114423. doi:10.1016/j.socscimed.2021.114423
40. Freeman, S, Spirgiene, L, Martin-Khan, M, and Hirdes, JP. Relationship Between Restraint Use, Engagement in Social Activity, and Decline in Cognitive Status Among Residents Newly Admitted to Long-Term Care Facilities. Geriatr Gerontol Int (2017) 17:246–55. doi:10.1111/ggi.12707
41. Fu, C, Li, Z, and Mao, Z. Association Between Social Activities and Cognitive Function Among the Elderly in China: A Cross-Sectional Study. Int J Environ Res Public Health (2018) 15:231. doi:10.3390/ijerph15020231
42. Fung, AWT, Lee, ATC, Cheng, S-T, and Lam, LCW. Loneliness Interacts With Family Relationship in Relation to Cognitive Function in Chinese Older Adults. Int Psychogeriatr (2019) 31:467–75. doi:10.1017/S1041610218001333
43. Gamage, MWK, Hewage, C, and Pathirana, KD. Associated Factors for Cognition of Physically Independent Elderly People Living in Residential Care Facilities for the Aged in Sri Lanka. BMC Psychiatry (2019) 19:10. doi:10.1186/s12888-018-2003-5
44. Glei, DA, Landau, DA, Goldman, N, Chuang, Y-L, Rodríguez, G, and Weinstein, M. Participating in Social Activities Helps Preserve Cognitive Function: An Analysis of a Longitudinal, Population-Based Study of the Elderly. Int J Epidemiol (2005) 34:864–71. doi:10.1093/ije/dyi049
45. Gow, AJ, Corley, J, Starr, JM, and Deary, IJ. Which Social Network or Support Factors Are Associated With Cognitive Abilities in Old Age? Gerontology (2013) 59:454–63. doi:10.1159/000351265
46. Gow, AJ, and Mortensen, EL. Social Resources and Cognitive Ageing Across 30 Years: The Glostrup 1914 Cohort. Age Ageing (2016) 45:480–6. doi:10.1093/ageing/afw070
47. Griffin, SC, Mezuk, B, Williams, AB, Perrin, PB, and Rybarczyk, BD. Isolation, Not Loneliness or Cynical Hostility, Predicts Cognitive Decline in Older Americans. J Aging Health (2020) 32:52–60. doi:10.1177/0898264318800587
48. Hajek, A, Riedel-Heller, SG, and König, H-H. Perceived Social Isolation and Cognitive Functioning. Longitudinal Findings Based on the German Ageing Survey. Int J Geriatr Psychiatry (2020) 35:276–81. doi:10.1002/gps.5243
49. Hamlin, AM, Kraal, AZ, Sol, K, Morris, EP, Martino, AG, Zaheed, AB, et al. Social Engagement and its Links to Cognition Differ Across Non-Hispanic Black and White Older Adults. Neuropsychology (2022) 36:640–50. doi:10.1037/neu0000844
50. Howrey, B, Avila, JC, Downer, B, and Wong, R. Social Engagement and Cognitive Function of Older Adults in Mexico and the United States: How Universal Is the Interdependence in Couples? J Gerontol - Ser B Psychol Sci Soc Sci (2021) 76:S41–S50. doi:10.1093/geronb/gbaa025
51. Hülür, G. Structural and Functional Aspects of Social Relationships and Episodic Memory: Between-Person and Within-Person Associations in Middle-Aged and Older Adults. Gerontology (2022) 68:86–97. doi:10.1159/000514949
52. James, BD, Wilson, RS, Barnes, LL, and Bennett, DA. Late-Life Social Activity and Cognitive Decline in Old Age. J Int Neuropsychol Soc (2011) 17(6):998–1005. doi:10.1017/S1355617711000531
53. Kim, Y. Gender Differences in the Link Between Marital Status and the Risk of Cognitive Impairment: Results From the Korean Longitudinal Study of Aging. Int J Aging Hum Dev (2022) 94:415–35. doi:10.1177/00914150211024181
54. Kim, YB, and Lee, SH. Social Network Types and Cognitive Decline Among Older Korean Adults: A Longitudinal Population-Based Study. Int J Geriatr Psychiatry (2019) 34:1845–54. doi:10.1002/gps.5200
55. Lara, E, Caballero, FF, Rico-Uribe, LA, Olaya, B, Haro, JM, Ayuso-Mateos, JL, et al. Are Loneliness and Social Isolation Associated With Cognitive Decline? Int J Geriatr Psychiatry (2019) 34:1613–22. doi:10.1002/gps.5174
56. Lee, H. Disorder, Networks, and Cognition: Do Social Networks Buffer the Influence of Neighborhood and Household Disorder on Cognitive Functioning? Aging Ment Health (2022) 26:1010–8. doi:10.1080/13607863.2021.1922600
57. Lee, H, and Ang, S. Productive Activities and Risk of Cognitive Impairment and Depression: Does the Association Vary by Gender? Sociol Perspect (2020) 63:608–29. doi:10.1177/0731121419892622
58. Lee, S, Lee, S, Lee, E, Youm, Y, Cho, HS, and Kim, WJ. Gender Differences in Social Network of Cognitive Function Among Community-Dwelling Older Adults. Geriatr Gerontol Int (2020) 20:467–73. doi:10.1111/ggi.13906
59. Lee, Y-H, Lin, C-H, Chang, J-R, Liu, C-T, Shelley, M, and Chang, Y-C. Transition of Living Arrangement and Cognitive Impairment Status Among Chinese Older Adults: Are They Associated? Med Lith (2021) 57:961. doi:10.3390/medicina57090961
60. Lee, Y, and Jean Yeung, W-J. Gender Matters: Productive Social Engagement and the Subsequent Cognitive Changes Among Older Adults. Soc Sci Med (2019) 229:87–95. doi:10.1016/j.socscimed.2018.08.024
61. Levasseur, M, Naud, D, Bruneau, J-F, and Généreux, M. Environmental Characteristics Associated With Older Adults’ Social Participation: The Contribution of Sociodemography and Transportation in Metropolitan, Urban, and Rural Areas. Int J Environ Res Public Health (2020) 17:8399–15. doi:10.3390/ijerph17228399
62. Li, J, Li, J, Wang, Z, Lian, Z, Zhu, Z, and Liu, Y. Social Networks, Community Engagement, and Cognitive Impairment Among Community-Dwelling Chinese Older Adults. Dement Geriatr Cogn Disord Extra (2019) 9:330–7. doi:10.1159/000502090
63. Li, M, and Dong, X. Is Social Network a Protective Factor for Cognitive Impairment in US Chinese Older Adults? Findings From the PINE Study. Gerontology (2018) 64:246–56. doi:10.1159/000485616
64. Meister, LM, and Zahodne, LB. Associations Between Social Network Components and Cognitive Domains in Older Adults. Psychol Aging (2021) 37:591–603. doi:10.1037/pag0000672
65. Oh, SS, Cho, E, and Kang, B. Social Engagement and Cognitive Function Among Middle-Aged and Older Adults: Gender-Specific Findings From the Korean Longitudinal Study of Aging (2008–2018). Sci Rep (2021) 11:15876. doi:10.1038/s41598-021-95438-0
66. Pillemer, S, Ayers, E, and Holtzer, R. Gender-Stratified Analyses Reveal Longitudinal Associations Between Social Support and Cognitive Decline in Older Men. Aging Ment Health (2019) 23:1326–32. doi:10.1080/13607863.2018.1495178
67. Pugh, E, De Vito, A, Divers, R, Robinson, A, Weitzner, DS, and Calamia, M. Social Factors That Predict Cognitive Decline in Older African American Adults. Int J Geriatr Psychiatry (2021) 36:403–10. doi:10.1002/gps.5435
68. Roystonn, K, Abdin, E, Shahwan, S, Zhang, Y, Sambasivam, R, Vaingankar, JA, et al. Living Arrangements and Cognitive Abilities of Community-Dwelling Older Adults in Singapore. Psychogeriatrics (2020) 20:625–35. doi:10.1111/psyg.12532
69. Schwartz, E, Khalaila, R, and Litwin, H. Contact Frequency and Cognitive Health Among Older Adults in Israel. Aging Ment Health (2019) 23:1008–16. doi:10.1080/13607863.2018.1459472
70. Sharifian, N, Manly, JJ, Brickman, AM, and Zahodne, LB. Social Network Characteristics and Cognitive Functioning in Ethnically Diverse Older Adults: The Role of Network Size and Composition. Neuropsychology (2019) 33:956–63. doi:10.1037/neu0000564
71. Tang, X, Houzé de l’Aulnoit, S, Buelow, MT, Slack, J, Singer, BC, and Destaillats, H. Performance of a CO2 Sorbent for Indoor Air Cleaning Applications: Effects of Environmental Conditions, Sorbent Aging, and Adsorption of Co-Occurring Formaldehyde. Indoor Air (2020) 30:1283–95. doi:10.1111/ina.12695
72. Tomioka, K, Kurumatani, N, and Hosoi, H. Social Participation and Cognitive Decline Among Community-Dwelling Older Adults: A Community-Based Longitudinal Study. J Gerontol - Ser B Psychol Sci Soc Sci (2018) 73:799–806. doi:10.1093/geronb/gbw059
73. Torres, JM, Sofrygin, O, Rudolph, KE, Haan, MN, Wong, R, and Maria Glymour, M. US Migration Status of Adult Children and Cognitive Decline Among Older Parents Who Remain in Mexico. Am J Epidemiol (2020) 189:761–9. doi:10.1093/aje/kwz277
74. Van Gelder, BM, Tijhuis, M, Kalmijn, S, Giampaoli, S, Nissinen, A, and Kromhout, D. Marital Status and Living Situation During a 5-Year Period Are Associated With a Subsequent 10-Year Cognitive Decline in Older Men: The FINE Study. J Gerontol - Ser B Psychol Sci Soc Sci (2006) 61:P213–9. doi:10.1093/geronb/61.4.P213
75. Windsor, TD, Ghisletta, P, and Gerstorf, D. Social Resources as Compensatory Cognitive Reserve? Interactions of Social Resources With Education in Predicting Late-Life Cognition. J Gerontol - Ser B Psychol Sci Soc Sci (2020) 75:1451–61. doi:10.1093/geronb/gby143
76. Xiong, Y, Zhang, Y, Zhang, F, Wu, C, Huang, X, Qin, F, et al. Risks and Subgroups of Cognitive Impairment Under Different Marital Status Among Older Adults: A Latent Profile Analysis. J Mens Health (2021) 17:234–42. doi:10.31083/jomh.2021.092
77. Xu, P-R, Wei, R, Cheng, B-J, Wang, A-J, Li, X-D, Li, H-B, et al. The Association of Marital Status With Cognitive Function and the Role of Gender in Chinese Community-Dwelling Older Adults: A Cross-Sectional Study. Aging Clin Exp Res (2021) 33:2273–81. doi:10.1007/s40520-020-01743-5
78. Xu, X, Dong, D, Wang, Y, and Wang, S. The Impacts of Different Air Pollutants on Domestic and Inbound Tourism in China. Int J Environ Res Public Health (2019) 16. doi:10.3390/ijerph16245127
79. Yang, L, Cheng, J, and Wang, H. Place of Residence and Cognitive Function in Older Adults in China: The Mediating Role of Social Participation. Int J Environ Res Public Health (2022) 19:13. doi:10.3390/ijerph19010013
80. Yin, S, Yang, Q, Xiong, J, Li, T, and Zhu, X. Social Support and the Incidence of Cognitive Impairment Among Older Adults in China: Findings From the Chinese Longitudinal Healthy Longevity Survey Study. Front Psychiatry (2020) 11:254. doi:10.3389/fpsyt.2020.00254
81. Zhang, W, Liu, S, Sun, F, and Dong, X. Neighborhood Social Cohesion and Cognitive Function in U.S. Chinese Older Adults—Findings From the PINE Study. Aging Ment Health (2019) 23:1113–21. doi:10.1080/13607863.2018.1480705
82. Zhou, G, Li, C, Liu, Y, and Zhang, J. Complexity of Functional Urban Spaces Evolution in Different Aspects: Based on Urban Land Use Conversion. Complexity (2020) 2020. doi:10.1155/2020/9741203
83. Zunzunegui, M-V, Alvarado, BE, Del Ser, T, and Otero, A. Social Networks, Social Integration, and Social Engagement Determine Cognitive Decline in Community-Dwelling Spanish Older Adults. J Gerontol - Ser B Psychol Sci Soc Sci (2003) 58:S93–S100. doi:10.1093/geronb/58.2.S93
84. Bae, S-M. The Association Between Health-Related Factors, Physical and Mental Diseases, Social Activities, and Cognitive Function in Elderly Koreans: A Population-Based Cross-Sectional Study. Psychogeriatrics (2020) 20:654–62. doi:10.1111/psyg.12561
85. Zhou, Y, Chen, Z, Shaw, I, Wu, X, Liao, S, Qi, L, et al. Association Between Social Participation and Cognitive Function Among Middle- and Old-Aged Chinese: A Fixed-Effects Analysis. J Glob Health (2020) 10:020801–11. doi:10.7189/jogh.10.020801
86. Tang, F, Zhang, W, Chi, I, Li, M, and Dong, XQ. Importance of Activity Engagement and Neighborhood to Cognitive Function Among Older Chinese Americans. Res Aging (2020) 42:226–35. doi:10.1177/0164027520917064
87. Xu, H, Vorderstrasse, AA, Dupre, ME, McConnell, ES, Østbye, T, and Wu, B. Gender Differences in the Association Between Migration and Cognitive Function Among Older Adults in China and India. Arch Gerontol Geriatr (2019) 81:31–8. doi:10.1016/j.archger.2018.11.011
88. Corley, J, Cox, SR, and Deary, IJ. Healthy Cognitive Ageing in the Lothian Birth Cohort Studies: Marginal Gains Not Magic Bullet. Psychol Med (2018) 48:187–207. doi:10.1017/S0033291717001489
89. Presseau, J, Hawthorne, G, Sniehotta, FF, Steen, N, Francis, JJ, Johnston, M, et al. Improving Diabetes Care Through Examining, Advising, and Prescribing (IDEA): Protocol for a Theory-Based Cluster Randomised Controlled Trial of a Multiple Behaviour Change Intervention Aimed at Primary Healthcare Professionals. Implement Sci (2014) 9:61. doi:10.1186/1748-5908-9-61
90. Centre for Thriving Places. A Wellbeing Future, Now - Centre for Thriving Places (2023). Available from: https://www.centreforthrivingplaces.org/ (Accessed March 27, 23).
Keywords: social determinants, older adults, population health, cognitive frailty, social engagement
Citation: Fowler Davis S, Benkowitz C, Holland C, Gow A and Clarke C (2024) A Scoping Review on the Opportunities for Social Engagement and Cognitive Frailty in Older Adults. Public Health Rev 45:1606494. doi: 10.3389/phrs.2024.1606494
Received: 10 August 2023; Accepted: 15 January 2024;
Published: 08 February 2024.
Edited by:
Ana Ribeiro, University Porto, PortugalReviewed by:
Three reviewers who chose to remain anonymousCopyright © 2024 Fowler Davis, Benkowitz, Holland, Gow and Clarke. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
PHR is edited by the Swiss School of Public Health (SSPH+) in a partnership with the Association of Schools of Public Health of the European Region (ASPHER)+
*Correspondence: Sally Fowler Davis, sally.fowler-davis@aru.ac.uk
This Mini Review is part of the PHR Special Issue “Neighbourhood Influences On Population Health”
 Sally Fowler Davis
Sally Fowler Davis Charlotte Benkowitz2
Charlotte Benkowitz2 Alan Gow
Alan Gow