Abstract
Objectives:
The purpose of this study, as a systematic review and meta-analysis, is to summarize the evidence on the effects of occupational exposure to VOCs on sleep quality.
Methods:
We used five electronic bibliographic databases to identify eligible studies. Three groups of keywords were applied in the search strategy. In evaluating the quality of studies and risk of bias, we utilized the Joanna Briggs Institute tools and the Risk of Bias in Non-randomized Studies of Exposures (ROBINS-E) instruments, respectively. The pooled values were also calculated by meta-analysis.
Results:
37 articles were included in the study. There was a consistent finding that exposure to volatile organic compounds (VOCs) adversely affected sleep in workers across various professions. The pooled value of the odds ratio of sleep problems because of exposure to VOCs was 1.60 [95% CI (1.01, 2.19)].
Conclusion:
Most studies indicated that occupational exposure to VOCs can significantly influence the sleep of workers in various professions. The exposure can be associated with a variety of sleep problems.
Introduction
Atmospheric volatile organic compounds (VOCs) are comprised of thousands of gaseous organic trace species [1]. These compounds have a high vapor pressure and low water solubility. Those can be directly emitted from biogenic and anthropogenic sources [1]. Many VOCs are human-made chemicals that are applied in the manufacture of paints, pharmaceuticals, and refrigerants. VOCs are typically used as industrial solvents and those are often components of petroleum fuels, hydraulic fluids, paint thinners, and dry-cleaning agents. VOCs are common ground-water contaminants. Some known VOCs include benzene, toluene, xylene, and ethylbenzene [2].
There are various professions in which workers are exposed to volatile organic compounds (VOCs). For instance, Jo and Song discovered that individuals working in occupations with exposure to gasoline vapor emissions and motor vehicle exhaust significantly experience exposure to elevated levels of aromatic VOCs during their work. Some of these occupations include service station workers, traffic policemen, and parking garage workers, [3]. Previous studies have also identified other occupations at risk of VOC exposure, such as those in the petroleum industry [4], basic iron and steel manufacturing factory [5], automobile-producing factories [6], painting units of automobile-producing factories [7], and gasoline and Compressed Natural Gas (CNG) stations [8]. Furthermore, there are VOCs exposure in small occupations, such as repair shops laundries, and restaurants continuously emit VOCs [9, 10].
Exposure to VOCs may have adverse health consequences including the effects on the nervous system, skin, and respiratory. Moreover, there is emerging evidence that exposure to VOCs may be associated with sleep problems. In the present systematic review and meta-analysis, VOCs were selected to investigate their effect on sleep problems for several reasons. First, exposure to VOCs are currently found in various workplaces, and those are introduced as one of common indoor and outdoor air pollutants in occupational settings [11]. Second, the findings of various studies demonstrated that exposure to VOCs can be associated with serious physiological and psychological effects [12, 13]. As physiological consequences, exposure to VOCs can lead to neurobehavioral consequences, chronic bronchitis, sleep apnea, and allergic reactions [12, 14–16]. In addition to physiological consequences, psychological effects due to exposure to VOCs such as stress and anxiety can be created because of annoyance and health concerns [13]. These alternations can make neurobehavioral and respiratory disturbances and disrupt circadian rhythms and melatonin secretion, which are related to sleep problems [17–19]. Original studies have investigated the adverse impact of both environmental (indoor and ambient) exposures and occupational exposures to VOCs on sleep issues. However, previous systematic reviews have only investigated the relationships between environmental exposure to air pollutants including VOCs, and sleep [20]. While occupational exposure to VOCs is common in many industries, evidence for the impact of such exposure on sleep health has not been synthesized. The purpose of this study, as a systematic review and meta-analysis, is to summarize the evidence on the effects of occupational exposure to VOCs on sleep quality.
Methods
This systematic review and meta-analysis study has been registered on PROSPERO (CRD42023391106) and has been written based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [21]. Furthermore, the PECO framework, for Population, Exposure, Comparator, and Outcome, has been provided to represent a clearer depiction of the relationship between occupational exposure to VOCs and sleep problems [22]. In this systematic review and meta-analysis study, the PECO framework informed the formulation of the research question, as well as the search strategy and criteria for inclusion and exclusion.
Search Strategy
A systematic search was conducted in five electronic bibliographic databases (Scopus, PubMed, Web of Science, Embase, and Medline) up to 04 March 2024. Three groups of keywords related to occupational exposure to VOCs and sleep problems were used in combination for the search algorithm. The search was conducted without time limitations. The first group of keywords consisted of sleepiness OR sleep OR dyssomnia OR circadian OR parasomnia OR hypersomnia OR Insomnia OR RLS OR restless legs syndrome OR Willis Ekbom Disease OR narcolep OR paroxysmal OR periodic limb movement disorder OR gelineau Syndrome OR nightmare OR somnolence OR nocturnal myoclonus syndrome. The second set of keywords comprised gas OR Vapor OR solvent OR vapour OR VOC OR volatile organic compound. The third set of keywords included industry OR occupation OR industrial OR employee OR workplace OR worker OR workforce.
Inclusion and Exclusion Criteria
This systematic review and meta-analysis study included studies that investigated associations between occupational exposure to VOCs and sleep problems. Studies addressing all types of sleep problems and study designs were included without any time restrictions. Review articles, meta-analyses, conference papers, editorial letters, case reports, and trial studies were excluded from the study. Animal studies were also not included.
Study Selection
To select relevant studies, all identified papers were imported into Endnote and duplicates were omitted. Then, two independent reviewers (S.Y. and A.KH) assessed the papers for eligibility and chose the relevant studies. The remaining studies underwent a thorough review to confirm the criteria.
Quality Assessment
The quality of experimental, cohort, cross-sectional, and case-control studies was assessed using the critical appraisal tools provided by the Joanna Briggs Institute (JBI) [23]. The number of positive responses obtained from each checklist was summed to categorize articles into three groups: low quality, moderate quality, and high quality.
Risk of Bias Assessment
The potential for bias within the chosen studies was assessed using the Risk of Bias in Non-randomized Studies of Exposures (ROBINS-E) instrument by two independent evaluators, S.Y. and A.KH. This process involved an examination of seven distinct factors: confounding variables, selection bias, deviations from intended exposures, accuracy of exposure measurement, outcome measurement, missing data, and the clarity of reported findings. Each study underwent a separate risk of bias (ROB) analysis, with outcomes categorized as “low,” “moderate,” or “high” in terms of bias risk. An overall classification of “high” bias risk was assigned if any single criterion received a “high” rating. Conversely, a study was deemed to have a “low” overall bias risk if all criteria were marked as “low” risk. In cases where these conditions were not met, the study was designated as having a “moderate” overall risk of bias.
Data Extraction
Following the selection of relevant studies, information extraction was performed by the two reviewers. This information consisted of details such as the author’s name, publication year, origin country, sample size, job type, age range, gender distribution, study type, work experience, sources of pollutants, concentration levels of pollutants, types of pollutants, duration of pollutant exposure, sleep-related information, prevalence rates of sleep problems or disorders, tools used for assessment purposes, and outcomes observed in the studies.
Data Analysis
To determine the agreement between the reviewers in the data extraction process, Cohen’s kappa coefficient was utilized [24]. The obtained kappa coefficients for the first and second steps were 0.91 and 0.94 respectively. In this study, the pooled values of odds ratios and prevalence related to sleep problems due to exposure to VOCs were calculated by meta-analysis. To assess heterogeneity in occupational exposure to VOCs, the Cochrane Q-test was applied [25]. Additionally, I2 was computed as the proportion of variability due to heterogeneity [26]. For subgroup analyses, nations were grouped based on economic status from low and middle-income (LMIC) to high-income (HIC) following World Bank classifications [27]. Furthermore, the studies were categorized into five global regions: Europe, East/Southeast Asia/Oceania, the Middle East, North America, and Africa. Based on temporal data, studies were divided into those performed in or before 2010 and after 2010. Data was analyzed by STATA version 14.2.
Results
Search Results and Study Selection
In this systematic review and meta-analysis, a total of 4,097 papers were identified across various databases up to March 4, 2024. From these papers, 2,199 redundant studies were excluded. Subsequently, two investigators meticulously reviewed the titles and abstracts of the remaining 1,898 papers. Through this rigorous screening, an additional 1,861 papers were deemed irrelevant as those did not satisfy the inclusion criteria. Ultimately, 37 papers were entered into the present study [28].
Specification of the Articles
Table 1 presents the specifications of the articles that have been included in this systematic review. Out of the 37 research, 16 research were categorized as cross-sectional studies, 18 research were classified as case-control studies, two research were experimental studies, and one research was a cohort study. Of the studies, two were from South Korea, two from France, one from Australia, two from the United States, one from India, one from Singapore, one from Venezuela, four from Finland, four from Norway, two from Japan, two from Belgium, one from New Zealand, three from Sweden, one from Thailand, three from Turkey, two from Germany, one from Algeria, one from Hungary, one from Czechoslovakia, one from Poland, and one from Malaysia.
TABLE 1
| First author (Year) | Country | Sample size | Study type | Job type | Range/mean age (years) and gender | Work experience (years) | Pollutant sources | Concentration | Type of pollutant | Pollutant exposure duration (hr) | Sleep Information (prevalence) |
Tool of sleep quality | Outcome | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cho and Kang (2022) [29] | South Korea | 36996 | Cohort | General working population | 15 to ≥60 Male and female |
- | - | - | Vapors of solvent | - | Sleep disturbance (6.1%) | Minimal Insomnia Symptom Scale (MISS) | Exposure to vapors of solvent was positively associated with sleep disturbance (OR = 4.1) | Q1 |
| Lucas et al. (2015) [30] | France | 145 | Case-control | Dry-Cleaning Employees | 42 Male-female |
3 | dry-cleaning operations | 7 (ppm, air) and 73.6 (μg/l, blood) | Perchloroethylene | 6 to 10 | Sleepiness | Epworth’s validated scale | The exposed population did not exhibit an abnormal amount of drowsiness | Q2 |
| Jay et al. (2017) [31] | Australia | 2,961 | Cross-sectional | General working population | 20 to ≥55 Male and female |
- | Combustion products and engine emission | - | Vapors of solvents | ≥8 | Sleepiness (People with standard hours: 5.6% and With non-standard hours: 9.6%) | Epworth Sleepiness Scale (ESS) | The workers with non-standard hours are more likely to be at a higher risk of being exposed to workplace hazards and experiencing insufficient sleep and excessive sleepiness | Q2 |
| Gallicchio et al. (2011) [32] | United States | 961 | Cross-sectional | Cosmetologist | 42.95 Female |
- | Cosmetology activities | - | Vapors of solvents | - | Sleep disturbance (33.1%) | Sleep survey | Handling cleaning supplies was found to have a significant correlation with frequent disturbances in sleep (OR = 1.64) | Q1 |
| Tripathi et al. (1989) [33] | India | 95 | Case-control | Painters | 32.75 Male |
10.63 | High-pressure spray painting | 0.59 to 4.63 (mg/m3, air) | Volatile solvents such as mineral spirit, xylene, and thinner | 4 | Sleepiness | Visual analogue scales | Noteworthy negative effects on levels of sleepiness were observed among painters | Q3 |
| Ng et al. (1990) [34] | Singapore | 223 | Case-control | Printing and paint workers | 32.8 Male |
9.9 | - | - | mixture of organic solvents | - | Sleep disturbance (20.5%) | Structured questionnaire | An excess of symptoms of sleep disturbances was seen in the exposed group. | Q2 |
| Escalona et al. (1995) [35] | Venezuela | 149 | Case-control | Workers in adhesive factory | 31.5 Male and female |
7 | immersing into vats of solvent mixtures, drying, and cutting rolls | Toluene = 58 ppm; Xylene = 5.1 ppm; Pentane = 5.6 ppm; Heptane = 2.2 ppm; Hexane = 4.6 ppm; n-Hexane = 2.2 ppm; Benzene = 0.3 ppm |
Vapors of solvents | - | Insomnia (15%) and wakeful sleep (43%) | Self-report questionnaire | The group that was exposed to the stimulus exhibited a higher occurrence of sleep disruptions in comparison to the group that was not exposed | Q1 |
| Antti-Poika et al. (1982) [36] | Finland | 361 | cross-Sectional | Painters, workers in paint factories, carpet workers, workers in furniture factories, and laundry workers | 38.6 Male and female |
10.4 | - | - | Trichloroethylene, perchloroethylene and solvent mixtures | - | Sleep disturbances (22%) | Self-report questionnaire | It was found that the exposure can significantly cause sleep disturbances | Q2 |
| Laine et al. (1993) [37] | Finland | 21 | Experimental | - | 19 to 23 Male |
- | Experimental chamber | 200–400 ppm | m-xylene | - | Poor sleep quality | Static charge sensitive bed (SCSB) device | The effects of exposure to m-xylene at a consistent concentration of 200 ppm on the sleep patterns of subjects were investigated using static charge-sensitive bed recording. It was found that this exposure did not have a significant impact on the ratio of “active” to “quiet” sleep. However, there was a slight decrease in the number of body movements during sleep | Q1 |
| Monstad et al. (1992) [38] | Norway | 85 | Case-control | House painters, car painters, and garage mechanics | 46.8 Male and female |
- | - | - | Organic solvents | - | Sleep apnea (35%) | Polysomnography | Individuals who were no longer exposed to solvents exhibited a significantly lower apnea index compared to those who had recently been exposed (P < 0.05) | Q1 |
| Takeuchi et al. (1975) [39] | Japan | 4 | Cross-sectional | Brocade sashes cleaners | 16 to 34 Male and female |
- | Solvent | 1,250 ppm | Petroleum benzine | 8 to ≥12 | Insomnia | Self-report questionnaire | The findings suggest that benzene may contribute to insomnia | Q3 |
| Vouriot et al. (2005) [40] | France | 43 | Case-control | Workers in serigraphy company | 36.3 Male and female |
6 | - | Benzene hydrocarbons = 80.1 mg/m3; 1-methoxy-2-propyl acetate = 20.4 mg/m3 |
Aromatic hydrocarbons | 8 | Poor sleep quality (9%) | Epworth sleepiness scale (ESS) and Pittsburgh sleep quality index (PSQI) | Workers who were exposed to vapors reported no disturbances in sleep quality when compared to control subjects | Q1 |
| Godderis et al. (2011) [41] | Belgium | 48 | Case-control | Printing plant workers | 33.8 Male |
13 | Cleaners of printing presses | - | Solvents | - | Sleep apnea (67%) | Sleep-related complaints questionnaire and polysomnography | The correlation between the sleep complaint scores and both the exposure index and duration was found to be positive (P = 0.01) in this study. Additionally, the polysomnography results revealed a higher occurrence of central apneas in the workers who were exposed (67%) compared to the referents (30%) | Q1 |
| Kaukiainen et al. (2009) [42] | Finland | 368 | Cross-sectional | General working population | 55.3 Male |
10.8 | - | - | Solvents | - | Sleep disturbance | Euroquest questionnaire | Sleep disturbance was found to be significantly more prevalent in cases of chronic solvent-induced encephalopathy compared to non-exposed cases (P < 0.001) | Q2 |
| Keer et al. (2016) [43] | New Zealand | 581 | Case-control | Vehicle collision repair workers | 36.5 Male |
17 | Paint panel beat and spray painters | Panel Beaters = 0.57 ppm; Spray Painters = 2.26 ppm | Propanols, methyl ethyl ketone, benzenes, hexanes, and ethanol | - | Sleep Disturbance (9.5) | Euroquest questionnaire | The employees involved in collision repair exhibited a considerably higher prevalence of sleep disturbance symptoms compared to the reference workers (OR = 1.8) | Q1 |
| Kraut et al. (2015) [44] | United States | 19 | Cross-sectional | Sewage treatment workers | 43 Male |
8.1 | - | 22–52 mg/L, urinary phenol level | Solvents | 8 | Sleep requirement (26%) | Self-report questionnaire | Fourteen individuals (comprising 74% of the sample) reported experiencing symptoms related to the central nervous system (CNS) that are commonly associated with exposure to solvents. These symptoms include feelings of dizziness, fatigue, an increased need for sleep, and headaches | Q2 |
| Lindelof et al. (2010) [45] | Sweden | 211 | Case-control | House painters, spray finishers, and printers | 52 Male |
- | - | - | Organic solvents | - | Insomnia (22%) |
Questionnaire | The findings demonstrated a greater occurrence of insomnia within the population exposed to solvents | Q2 |
| Tjalvin et al. (2015) [19] | Norway | 284 | Case-control | Industrial harbor area workers | 44.5 Male and female |
- | Chemical explosion | Hydrocarbons | - | Sleep problems | Subjective health complaints inventory | sleep problems were significantly different between exposed employees and controls | Q2 | |
| Monstad et al. (1987) [46] | Norway | 19 (group 1 = 15; group 2 = 8; control = 3) | Cross-sectional | Garage mechanic, vulcanization, offset printer, house painting, dry cleaning, plastic boat factory, gunsmiths | 37.7 Male and female |
- | - | - | Acetone, trichloroethane, toluene, and xylol | - | Sleep apnea (46%) | Polysomnography | The findings indicate that the occurrence of sleep apnea can be attributed to exposure to organic solvents | Q1 |
| Edling et al. (1993) [47] | Sweden | 66 | Cross-sectional | General working population | 53 Male |
24 | - | - | Organic solvents | - | Sleep apnea (19.7%) | Static charge sensitive bed and questionnaire | A high prevalence of sleep apnea was observed among a group of workers who were regularly exposed to organic solvents during their work activities | Q3 |
| Heo et al. (2013) [13] | South Korea | 7,112 | Cross-sectional | Korean workers | <30 to ≥60 Male and female |
<1 to ≥10 | - | - | Organic solvents | ≥8 | Sleep disturbance (28%) | Self-report questionnaire | Exposure to chemical substances has been found to have a substantial correlation with disruptions in sleep patterns (OR = 1.57) | Q2 |
| Thetkathuek et al. (2015) [48] | Thailand | 192 | Case-control | Workers in paint manufacturing | 33.33 Male and female |
6.2 | Xylene = 2.7 ppm, air; toluene = 9.5 ppm, air; methyl hippuric acid = 78 mg/g, urine | Toluene and xylene | - | Sleep disturbances (46.7%) | Interview Form |
The study revealed that individuals exposed to xylene experienced a significant increase in sleep disturbance, with an odds ratio (OR) of 3.9. Similarly, those exposed to toluene showed an even higher likelihood of sleep disturbance, with an OR of 4.4 | Q1 | |
| Sağcan et al. (2018) [49] | Turkey | 32 | Case-control | Street sign painters | 28.5 Male |
7.9 | - | - | Toluene and acetone | 11 | sleep apnea (44%) | Polysomnography and Epworth sleepiness scale (ESS) | A significant number of workers who were regularly exposed to solvents experienced sleep apnea | Q2 |
| Heiskel et al. (2002) [50] | Germany | 443 | Case-control | - | 20 to 89 Male |
- | - | - | Paints and solvents | - | Obstructive sleep apnea | Questionnaire | There was no evidence of a relationship between exposure to solvents and the occurrence of obstructive sleep apnea | Q1 |
| Mandiracioglu et al. (2011) [51] | Turkey | 263 | Cross-sectional | Furniture enterprises workers | 15 to ≥50 Male |
5 to 24 | Painting and varnishing | benzene = 0.11 ppm, blood; toluene = 0.43 ppm, blood | toluene, xylene and benzene | ≥8 | Sleep disturbances | Euroquest questionnaire | There were no observed differences in the mean scores of the neuropsychological symptoms questionnaire between the groups that were exposed and those that were not exposed | Q2 |
| Levy et al. (1997) [52] | Norway | - | Cross-sectional | Painters and workers in the printing industry | - Male and female |
- | - | - | Solvents | - | Sleep Disturbances | Self-report questionnaire | Subjects experienced disruptions in their sleep patterns as a result of their condition known as multiple chemical sensitivity (MCS) | Q2 |
| Laire et al. (1997) [53] | Belgium | 42 | Case-control | Offset printers | 38.1 Male and female |
15 | - | - | Solvents | - | Nocturnal desaturation | Pulse oximeter | The incidence of nocturnal desaturation was significantly elevated among the workers who were exposed to the hazardous conditions | Q1 |
| Sekkal et al. (2016) [54] | Algeria | 500 | Case-control | Handling/distributing petroleum products workers | 41 Male |
14 | handling/distributing petroleum products | - | Hydrocarbons | - | Poor sleep quality (15.6%) | Epworth questionnaire and Berlin questionnaire | The prevalence of sleep disturbances was found to be greater among employees who were exposed to the vapors, as compared to those who were not exposed | Q1 |
| Lovas et al. (2021) [55] | Hungary | 258 | Case-control | Warehouse workers | 39.7 Male and female |
- | Handling cargos | - | Volatile organic compounds (VOCs) | - | Sleep disturbances | European Health Interview survey | The subjects who were exposed to the vapors experienced a higher occurrence of subjective sleep disturbance symptoms compared to those who were not exposed | Q1 |
| Kaukiainen et al. (2009) [56] | Finland | 2,000 | Cross-sectional | Painters and carpenters | 48.7 Male |
11.8 | - | - | Solvents | - | Sleep disturbances | Euroquest-based questionnaire | Sleep disturbances were frequently documented during the clinical assessment | Q1 |
| Ulfberg et al. (1997) [57] | Sweden | 1,348 | Case - control | - | 50.6 Male and female |
- | - | - | Solvents | - | Obstructive sleep apnea syndrome (OSAS) and snoring | Oximetry and respiratory movement monitoring, static charge sensitive bed (SCSB) and questionnaire | The likelihood of developing Obstructive Sleep Apnea Syndrome (OSAS) or snoring was found to increase in correlation with greater levels of exposure | Q1 |
| Saygun et al. (2012) [58] | Turkey | 389 | Case-control | Workers in a gun factory | 41.4 Male |
17.74 | - | - | Solvents | 8 | Daytime sleepiness | Questionnaire | The group exposed to solvents exhibited a greater level of daytime sleepiness | Q2 |
| Kellerova et al. (1985) [59] | Czechoslovakia | 394 | Cross-Sectional | - | - | - | - | - | Organic solvents | - | Sleep phenomena (37.5%) | Electroencephalography | The rapid onset of deeper sleep stages was commonly associated with benzene exposure | Q3 |
| Indulski et al. (1996) [60] | Poland | 418 | Cross-Sectional | Workers in paint and varnish production | 20 to 59 Male and female |
17.34 | - | - | Organic solvent mixtures | - | Sleep disorders and sleepiness during the day | Electroencephalography | Sleep disorders and excessive sleepiness were the prevailing concerns reported by the exposed group throughout the daytime | Q3 |
| Kiesswetter et al. (1997) [61] | Germany | - | Experimental | - | - | - | - | 200–1,000 ppm | Organic solvents | - | Poor sleep quality | Self-report questionnaire | The employees exposed to solvents experienced a decrease in the quality of their sleep when compared to the control group | Q2 |
| Takeuchi et al. (1972) [62] | Japan | 2 | Cross-Sectional | paints industry workers | - Male |
- | - | - | Toluene | - | Insomnia | Self-report questionnaire | The participants expressed dissatisfaction with their inability to fall asleep and stay asleep | Q3 |
| Syazawani Shamsudin (2023) [63] | Malaysia | 42 | Cross-Sectional | Office employees | <40 to ≥40 Male and female |
<2 to ≥2 | - | 0.84 ppm | Volatile organic compounds (VOCs) | 8 | Sleepiness (80.25%) | Self-report questionnaire | The results showed that sleepiness was a symptom of the sick building syndrome because of exposure to pollutants among employees | Q3 |
The specification of the articles included in this systematic review - Iran, 2024.
NOTE:
Epworth sleepiness scale (ESS): Scores >10 are considered to be a sign of moderate and severe sleepiness.
Stop-Bang questionnaire: scores ≥3 are considered to be a sign of moderate and severe risk for OSA.
Among these studies, four research were conducted on the general working population, three on cleaning workers, one on cosmetologists, 15 on painters and workers in paint factories, two on mechanics and car repair workers, and two on furniture factories. Other studied populations included carpet workers, laundry workers, workers in adhesive factories, sewage treatment workers, spray finishers, industrial harbor area workers, handling/distributing petroleum products workers, warehouse workers, workers in gun factories, and office employees.
Of the studies, 16 were carried out among males, one among females, and 20 among both males and females. Of the studies, 12 investigated sleep disturbance, 6 assessed sleepiness, 4 assessed insomnia, 4 assessed poor sleep quality, 7 assessed sleep apnea, and 4 evaluated other sleep problems. Based on the quality assessment, 16 were categorized as high quality (43.24 percent), 14 as moderate quality (37.84 percent), and 7 as low quality (18.92 percent) (Figure 1).
FIGURE 1
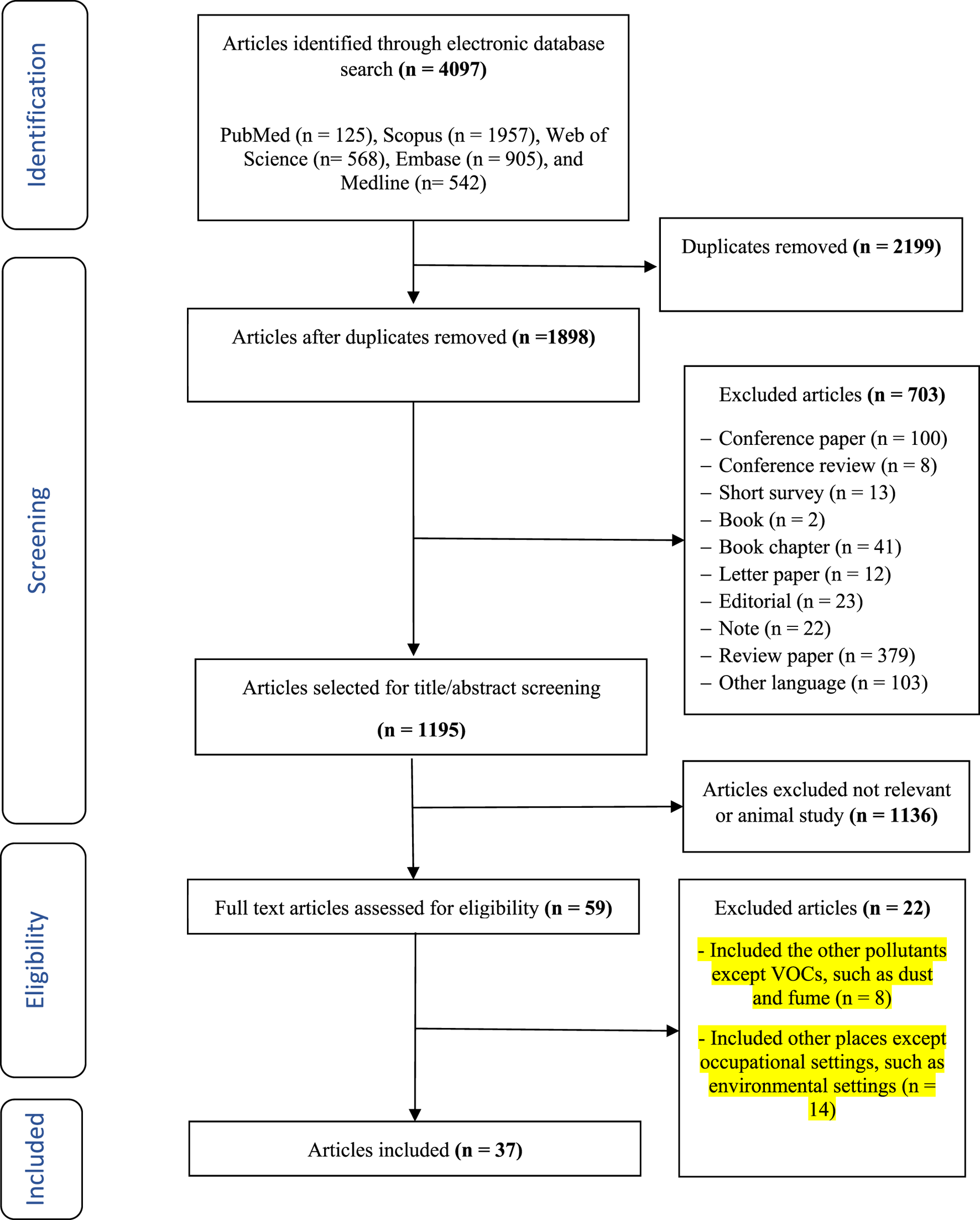
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram - Iran, 2024.
Qualitative Findings
Figure 2 illustrates the global map of the prevalence of sleep problems due to occupational exposure to VOCs. Based on the results, the highest sleep problems due to this exposure were found in Sweden due to exposure to VOCs among the general working population (82.5 percent) and Malaysia due to exposure to VOCs among office employees (80.25 percent), respectively.
FIGURE 2
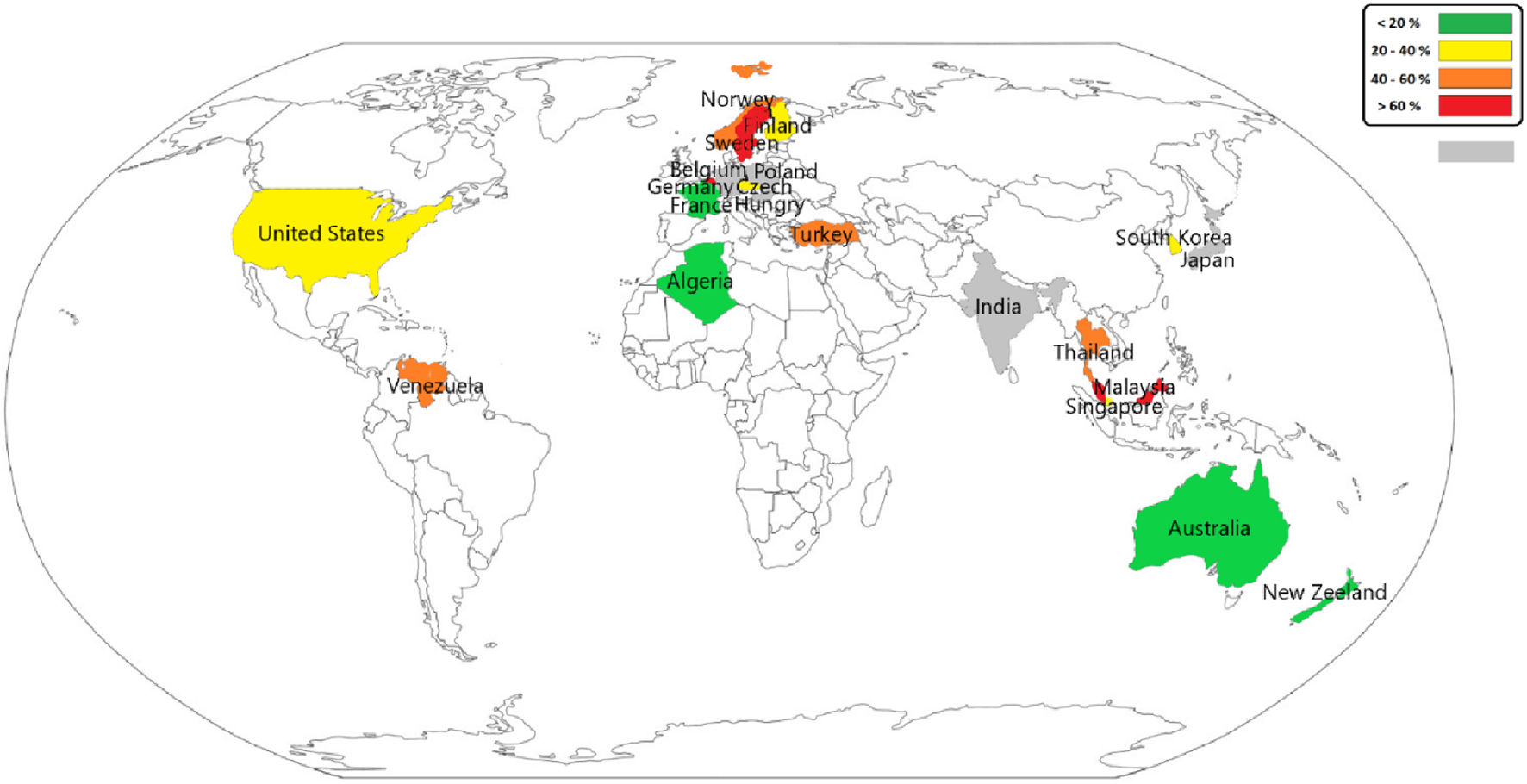
Global map of the prevalence of sleep problems due to occupational exposure to volatile organic compounds - Iran, 2024.
Among 16 articles with high quality, 13 (81.25%) showed that exposure to VOC had a significant negative effect on sleep among workers in various occupations. Among 14 articles with moderate quality, 12 studies (85.71%) showed that exposure to VOC had a significant effect on sleep among workers in various occupations. Among 7 articles with low quality, all (100.00%) indicated that exposure to VOC had a significant effect on sleep among workers in various occupations.
Figure 3; Table 2 show the pooled values of outcomes related to sleep problems due to exposure to VOCs. The results of the meta-analysis revealed that the pooled value of the odds ratio in the studies was 1.60 [95% CI (1.01, 2.19)]. Also, the results of the meta-analysis indicated that the pooled value of the prevalence in the studies was 30.17 [95% CI (25.84, 34.50)]. Moreover, Table 3 completely describes the findings of the subgroup analysis for the odd ratios and prevalences. The pooled values of odds ratios were significantly greater in countries with high incomes {1.70 [95% CI (1.01, 2.40)]} compared to those with low and medium incomes, in the East/Southeast Asia/Oceania {2.00 [95% CI (1.24, 2.77)]} compared to other regions, and in 2010 or earlier {1.68 [95% CI (0.35, 3.02)]} compared to after this time. The pooled values of prevalence were significantly higher in countries with low and medium incomes {39.48 [95% CI (26.49, 52.46)]} compared to those with high incomes, in the Middle East {44.00 [95% CI (36.24, 51.76)]} compared to other regions, and in 2010 or earlier {33.96 [95% CI (26.58, 41.34)]} compared to after this time.
FIGURE 3
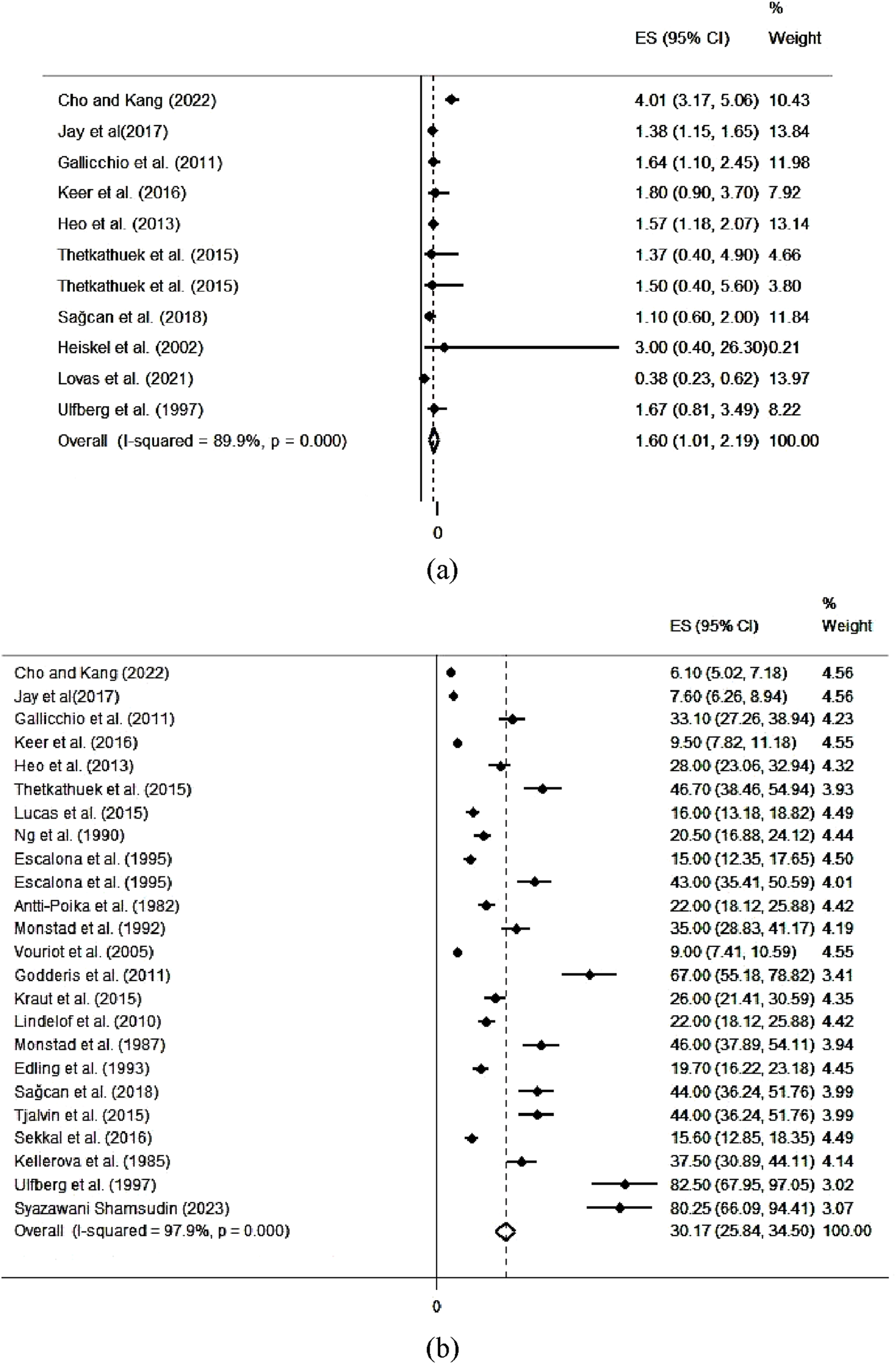
The pooled values of outcomes related to sleep problems due to occupational exposure to volatile organic compounds. (a) odds ratio and (b) prevalence - Iran, 2024.
TABLE 2
| Outcome type | Authors (year) | Effect size | 95% confidence intervals | Weight (%) |
|---|---|---|---|---|
| Odds ratio | Cho and Kang [29] | 4.01 | (3.17–5.06) | 10.43 |
| Jay et al. [31] | 1.38 | (1.15–1.65) | 13.84 | |
| Gallicchio et al. [32] | 1.64 | (1.10–2.45) | 11.98 | |
| Keer et al. [43] | 1.80 | (0.90–3.70) | 7.92 | |
| Heo et al. [13] | 1.57 | (1.18–2.07) | 13.14 | |
| Thetkathuek et al. [48] | 1.37 | (0.40–4.90) | 4.66 | |
| Thetkathuek et al. [48] | 1.50 | (0.40–5.60) | 3.80 | |
| Sagcan et al. (2018) [49] | 1.10 | (0.60–2.00) | 11.84 | |
| Heiskel et al. [50] | 3.00 | (0.40–26.30) | 0.21 | |
| Lovas et al. [55] | 0.38 | (0.23–0.62) | 13.97 | |
| Ulfberg et al. [57] | 1.67 | (0.81–3.49) | 8.22 | |
| Overall | 1.60 | (1.01–2.19) | 100.00 | |
| prevalence | Cho and Kang [29] | 6.10 | (5.02–7.18) | 4.56 |
| Jay et al. [31] | 7.60 | (6.26–8.94) | 4.56 | |
| Gallicchio et al. [32] | 33.10 | (27.26–38.94) | 4.23 | |
| Keer et al. [43] | 9.50 | (7.82–11.18) | 4.55 | |
| Heo et al. [13] | 28.00 | (23.06–32.94) | 4.32 | |
| Thetkathuek et al. [48] | 46.70 | (38.46–54.94) | 3.93 | |
| Lucas et al. [30] | 16.00 | (13.18–18.82) | 4.49 | |
| Ng et al. [34] | 20.50 | (16.88–24.12) | 4.44 | |
| Escalona et al. [35] | 15.00 | (12.35–17.65) | 4.50 | |
| Escalona et al. [35] | 43.00 | (35.41–50.59) | 4.01 | |
| Antti-Poika et al. [36] | 22.00 | (18.12–25.88) | 4.42 | |
| Monstad et al. [38] | 35.00 | (28.83–41.17) | 4.19 | |
| Vouriot et al. [40] | 9.00 | (7.41–10.59) | 4.55 | |
| Godderis et al. [41] | 67.00 | (55.18–78.82) | 3.41 | |
| Kraut et al. [44] | 26.00 | (21.41–30.59) | 4.35 | |
| Lindelof et al. [45] | 22.00 | (18.12–25.88) | 4.42 | |
| Monstad et al. (1987) [46] | 46.00 | (37.89–54.11) | 3.94 | |
| Edling et al. [47] | 19.70 | (16.22–23.18) | 4.45 | |
| Sagcan et al. (2018) [49] | 44.00 | (36.24–51.76) | 3.99 | |
| Tjalvin et al. [19] | 44.00 | (36.24–51.76) | 3.99 | |
| Sekkal et al. [54] | 15.60 | (12.85–18.35) | 4.49 | |
| Kellerova et al. [59] | 37.50 | (30.89–44.11) | 4.14 | |
| Ulfberg et al. [57] | 82.50 | (67.95–97.05) | 3.02 | |
| Syazawani Shamsudin [63] | 80.25 | (66.09–94.41) | 3.07 | |
| Overall | 30.17 | (25.84–34.50) | 100 |
The results of meta-analysis on outcomes related to sleep problems due to occupational exposure to volatile organic compounds - Iran, 2024.
TABLE 3
| Subgroup analysis | Subgroup | Category (number of studies) | Pooled prevalence (%) [95% CI] | I 2 (%) | Q statistic (df) | p of heterogeneity |
|---|---|---|---|---|---|---|
| Odds ratio | Income level | High income (8) LMICs (3) |
1.70 [1.00, 2.40] 1.14 [0.50, 1.79] |
92.9 0.0 |
7 2 |
<0.0001 0.93 |
| Region | Europe (3) East/southeast Asia/Oceania (6) Middle East (1) North America (1) Africa (−) |
0.80 [-0.21, 1.82] 2.00 [1.23, 2.76] 1.10 [0.40, 1.80] 1.64 [0.96, 2.31] - |
45.1 82.1 - - - |
2 5 0 0 - |
0.16 <0.0001 - - - |
|
| Study date | In or before 2010 (2) After 2010 (9) |
1.68 [0.35, 3.01] 1.59 [0.96, 2.22] |
0.0 91.8 |
1 8 |
0.84 <0.0001 |
|
| prevalence | Income level | High income (18) LMICs (6) |
27.39 [22.79, 31.99] 39.47 [26.49, 52.45] |
97.9 97.6 |
17 5 |
<0.0001 <0.0001 |
| Region | Europe (11) East/southeast Asia/Oceania (7) Middle East (1) North America (4) Africa (1) |
34.84 [26.64, 43.05] 23.93 [17.79, 30.08] 44.00 [36.23, 51.76] 28.93 [17.30, 40.56] 15.60 [12.84, 18.35] |
97.6 98.0 - 95.9 - |
10 8 0 3 0 |
<0.0001 <0.0001 - <0.0001 - |
|
| Study date | In or before 2010 (12) After 2010 (12) |
33.95 [26.57, 41.34] 26.96 [21.42, 32.50] |
97.5 98.1 |
11 11 |
<0.0001 <0.0001 |
The results of subgroup analysis for the odd ratios and prevalence related to sleep problems due to occupational exposure to volatile organic compounds - Iran, 2024.
Assessment of Risk of Bias in Studies
The evaluation results of the seven ROB criteria for each of the articles have been reported in Supplementary Table S1. Out of the 37 selected articles, 67.6% (N = 25) had a high ROB rating, 21.6% (N = 8) were rated as moderate, and 10.8% (N = 4) had a low ROB. The highest percentage of high ROB was observed in the criteria of measurement of exposure and departure from exposure with 67.6% (N = 25). Also, selection bias was observed at a low level in 89.2% of studies.
Discussion
To the best of our knowledge, this is the first systematic review and meta-analysis study to investigate the associations between volatile organic compounds and sleep quality. In 81.25% of the high-quality studies (13 out of 16 studies), 85.71% of the moderate-quality studies, (12 out of 14 studies), and all of the low-quality studies (7 out of 7 studies), there was a consistent finding that exposure to volatile organic compounds (VOCs) adversely affected sleep in workers across various professions. It has been proposed that this exposure can affect sleep in three different ways, including neurobehavioral, chronic illnesses, and psychological.
One potential mechanism that can explain the impact of daytime occupational volatile organic compounds (VOC) exposure on sleep is the neurobehavioral effect resulting from chemical exposure. Exposure to VOC mist or vapors can directly or indirectly affect the nervous system, leading to neurobehavioral effects such as sleep problems [12]. This may be attributed to autonomic nervous dysfunction [34]. Extensive documentation exists regarding the neurotoxic effects of solvents, including VOCs, which can have toxic effects on the peripheral and central nervous system (CNS) [35]. Prolonged exposure to aromatic hydrocarbons is well-known to be associated with disruptions in CNS functioning [40]. The specific effects depend on the chemical composition of the VOCs [40]. Numerous studies have investigated this relationship [33, 41–43, 56].
As a second pathway, volatile organic compounds (VOCs) exposure can cause chronic illnesses. These include local inflammation of the airways, difficulty breathing leading to chronic bronchitis, and sleep apnea, which disrupts an individual’s comfort and results in sleep problems [14]. Prolonged exposure to solvents can specifically cause sleep disturbances, particularly sleep apnea syndromes [64]. Exposure to solvents may be associated with the occurrence of obstructive sleep apnea syndrome [40]. Additionally, certain VOCs may be associated with allergic reactions that can also cause sleep apnea [65]. Symptoms resulting from allergic and nonallergic rhinitis are considered agents affecting sleep apnea [66]. Potential mechanisms for this association consisted of the impact of nasal obstruction on the collapsibility of the nasopharynx downstream and inflammation related to increased nasal resistance [67]. Furthermore, exposure to certain VOCs can influence the central nervous system and consequently lead to central sleep apnea [38]. Previous studies have reported the potential impact of inhalational occupational exposures to various VOCs on sleep apnea [38, 41, 46, 47, 49]. Moreover, studies have shown that exposure to solvents such as acetone, methacrylate, and acetonitrile can result in asthma, eye irritation, skin irritation, nasal irritation, throat irritation, and dermatitis, which those can affect sleep quality among exposed people [15, 16].
In addition to the mentioned pathways, exposure to volatile organic compounds (VOCs) can induce stress and anxiety due to the annoyance and health concerns associated with direct exposure to hazardous VOCs in unfavorable working conditions [13]. These stressful conditions can increase stress reactions and activate the hypothalamic-pituitary-adrenal axis and rumination [17]. Stress-induced adrenal secretory activity disruption can disturb the rhythmic release of adrenal cortisol [17]. Like other workplace irritants, occupational exposure to VOCs may also contribute to mental disorders [17]. This effect of VOC exposure on mental health can be stated as “VOC annoyance.” A neurocognitive mechanism can explain this concept of mental health. Predisposing factors such as workplace stressors relate to perpetuating factors like extended time spent in bed due to obstacles in achieving de-arousal caused by cortical arousal [68]. These alterations in the human body can lead to sleepiness and sleep problems. Previous studies have shown that chronic stress has a relationship with sleep problems. Findings from some previous studies propose a mechanism mediated by smell perception and smell annoyance for the health effects resulting from solvent exposure [69–71]. Additionally, concerns about potential health risks have been reported to increase subjective health complaints [18, 19].
The findings of the meta-analysis revealed that the pooled value of the odds ratio related to sleep problems due to exposure to VOCs in the studies was equal to 1.60. On the other harmful factors in occupational settings, Heo et al. determined that physical agents could be associated with sleep disruptions, exhibiting an odds ratio of 1.47. In this research, they found that psychosocial factors might influence the sleep quality of employees, with odds ratios ranging from 1.45 to 2.93 [13]. Virtanen et al. discovered that prolonged work durations might correlate with a higher likelihood of reduced sleep duration and increased early morning awakenings, with odds ratios of 3.24 and 2.23, respectively [72]. Heiskel et al. concluded that solvent exposure could contribute to obstructive sleep apnea, with an odds ratio of 1.2 [50]. These results collectively suggest that chemical solvents, the same as other job hazards, may have a significant association with sleep-related issues.
The findings of the meta-analysis indicated that the pooled value of the prevalence of sleep problems due to exposure to VOCs in the studies was 30.17. The findings of previous research have shown that sleep disturbances among employees occur at a rate of nearly 18 percent in European countries and 23 percent in the United States [73, 74]. Cho et al. noted that sleep disturbances due to physical or chemical exposures had a prevalence between 10 and 26 percent [29]. Bertrais et al. observed that occupational hazards were associated with an increased occurrence of sleep problems (30 percent) in male workers [75]. The prevalence of sleep problems obtained in the current study is consistent with previous studies.
The results of subgroup analysis showed that the pooled values of odds ratios were significantly higher in countries with high incomes, in East/Southeast Asia/Oceania, and in 2010 or earlier. While on the prevalence of sleep problems, the pooled values were higher in countries with low and medium incomes, in the Middle East, and in 2010 or earlier. In nations with lower economic status, outdated industrial equipment often operates at reduced energy efficiency levels, leading to elevated pollutant emissions. Additionally, these countries may depend on less efficient energy sources like coal and mazut, contributing to health issues associated with air pollution. The lack of effective enforcement of environmental regulations, because of the prohibitive costs associated with pollution control, further increases the risk of pollutant exposure [76]. However, it must be stated that high-income and developed countries are not exempt from contributing to high levels of pollutants, which could be attributed to their more intensive industrial operations [77]. These causes might somewhat describe the findings of the present studies.
In this study, 16 articles were classified as high quality, 14 studies as moderate quality, and 7 studies as low-quality studies. Therefore, these results show that a low number of low-quality studies were included in this systematic review and meta-analysis study. However, the results of the bias assessment revealed that 67.6% of the studies had a high ROB rating, 21.6% of the studies were rated as moderate, and 10.8% of the studies had a low ROB. The low number of studies characterized by a low risk of bias (ROB) might be due to different factors. These include dependence on self-reporting tools or questionnaires to collect data [78–80], lack of detailed information on pollutant concentrations and sleep problems [81–83], failure to disclose exposure status [81, 84], use of same methodologies [85, 86], and instances of incomplete results [87–89].
Strengths
As a strength, a comprehensive systematic search was conducted across five electronic databases (Scopus, PubMed, Web of Science, Embase, Medline) with no time restrictions, using three groups of keywords covering sleep problems, VOCs, and occupational contexts. This minimized the risk of missing relevant studies. Moreover, duplicates were removed, and two independent reviewers assessed study eligibility, reducing selection bias.
Limitations
Based on the results, only one cohort study was performed among 37 studies. The prospective type of study design allows greater confidence in examining exposure values to VOCs compared to retrospective studies with the associated problems of recall fallacy. This limitation restricts the ability to draw causal inferences because cross-sectional and case control designs are not examined the temporal sequence between exposure and outcome. In cross-sectional design, exposure and outcome are simultaneously measured. In case-control studies also, previous exposures and outcomes are investigated. So, it is not clear which one happened first. Furthermore, the impact of confounding factors (such as other harmful agents in the workplace) has not been considered in some of the studies, which may affect the effect of exposure to VOCs. Moreover, most of the reviewed studies had no detailed information on pollutant concentrations and sleep problem metrics.
Conclusion
Based on the results of this systematic review, 32 out of 37 studies (86.49%) showed that occupational exposure to VOCs can significantly influence sleep among workers in various occupations. This exposure can cause a variety of sleep problems. There are three pathways for this impact, including the neurobehavioral effect due to exposure to VOCs on nighttime sleep, the effect of chronic illnesses due to exposure to VOCs on nighttime sleep, and the psychological effects due to exposure to VOCs on nighttime sleep. The results of this study can be helpful to plan the decrease of exposure to VOCs, such as decreased use of VOCs, design of general and local ventilations, and use of personal protective equipment, for preventing sleep disorders in the workplace. Also, people with sleep disorders should be prevented from employment in workplaces with high exposure to VOCs.
Statements
Author contributions
AK: Methodology, Formal analysis, Investigation, Writing – original draft, Visualization. SY: Conceptualization, Writing – review and editing, Supervision, Project administration. CD: Writing – original draft, Writing – review and editing, Visualization. JI: Writing – original draft, Writing – review and editing, Visualization. DB: Writing – original draft, Writing – review and editing, Visualization.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that they do not have any conflicts of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/phrs.2025.1608224/full#supplementary-material
References
1.
Mozaffar A Zhang Y-L . Atmospheric Volatile Organic Compounds (VOCs) in China: A Review. Curr Pollut Rep (2020) 6:250–63. 10.1007/s40726-020-00149-1
2.
Yaqub G Hamid A Khan N Ishfaq S Banzir A Javed T . Biomonitoring of Workers Exposed to Volatile Organic Compounds Associated With Different Occupations by Headspace GC-FID. J Chem (2020) 2020:1–8. 10.1155/2020/6956402
3.
Jo W-K Song K-B . Exposure to Volatile Organic Compounds for Individuals with Occupations Associated with Potential Exposure to Motor Vehicle Exhaust And/or Gasoline Vapor Emissions. Sci total Environ (2001) 269(1-3):25–37. 10.1016/s0048-9697(00)00774-9
4.
Khoshakhlagh AH Yazdanirad S Mousavi M Gruszecka-Kosowska A Shahriyari M Rajabi-Vardanjani H . Summer and Winter Variations of BTEX Concentrations in an Oil Refinery Complex and Health Risk Assessment Based on Monte-Carlo Simulations. Scientific Rep (2023) 13(1):10670. 10.1038/s41598-023-37647-3
5.
Omidi F Fallahzadeh RA Dehghani F Harati B Chamgordani SB Gharibi V . Carcinogenic and Non-carcinogenic Risk Assessment of Exposure to Volatile Organic Compounds (BTEX) Using Monte-Carlo Simulation Technique in a Steel Industry. J Health and Saf Work (2018) 8(3).
6.
Khoshakhlagh AH Yazdanirad S Saberi HR Liao P-C . Health Risk Assessment of Exposure to Various Vapors and Fumes in a Factory of Automobile Manufacturing. Heliyon (2023) 9(8):e18583. 10.1016/j.heliyon.2023.e18583
7.
Dehghani F Golbabaei F Abolfazl Zakerian S Omidi F Mansournia MA . Health Risk Assessment of Exposure to Volatile Organic Compounds (BTEX) in a Painting Unit of an Automotive Industry. J Health Saf Work (2018) 8(1):55–64.
8.
Hazrati S Rostami R Fazlzadeh M Pourfarzi F . Benzene, Toluene, Ethylbenzene and Xylene Concentrations in Atmospheric Ambient Air of Gasoline and CNG Refueling Stations. Air Qual Atmosphere and Health (2016) 9:403–9. 10.1007/s11869-015-0349-0
9.
Yang C Qian H Li X Cheng Y He H Zeng G et al Simultaneous Removal of Multicomponent VOCs in Biofilters. Trends Biotechnology (2018) 36(7):673–85. 10.1016/j.tibtech.2018.02.004
10.
Zhang X Gao B Creamer AE Cao C Li Y . Adsorption of VOCs onto Engineered Carbon Materials: A Review. J Hazard Mater (2017) 338:102–23. 10.1016/j.jhazmat.2017.05.013
11.
Çankaya S Pekey H Pekey B Aydın BÖ . Volatile Organic Compound Concentrations and Their Health Risks in Various Workplace Microenvironments. Hum Ecol Risk Assess An Int J (2020). 10.1080/10807039.2018.1539638
12.
Patel AV Mihalik JP Notebaert AJ Guskiewicz KM Prentice WE . Neuropsychological Performance, Postural Stability, and Symptoms after Dehydration. J athletic Train (2007) 42(1):66–75.
13.
Heo Y-S Chang S-J Park S-G Leem J-H Jeon S-H Lee B-J et al Association between Workplace Risk Factor Exposure and Sleep Disturbance: Analysis of the 2nd Korean Working Conditions Survey. Ann Occup Environ Med (2013) 25(1):41–11. 10.1186/2052-4374-25-41
14.
Taylor DJ Mallory LJ Lichstein KL Durrence HH Riedel BW Bush AJ . Comorbidity of Chronic Insomnia with Medical Problems. Sleep (2007) 30(2):213–8. 10.1093/sleep/30.2.213
15.
Roelofs C Azaroff LS Holcroft C Nguyen H Doan T . Results from a Community-Based Occupational Health Survey of Vietnamese-American Nail Salon Workers. J immigrant Minor Health (2008) 10:353–61. 10.1007/s10903-007-9084-4
16.
Sauni R Kauppi P Alanko K Henriks‐Eckerman ML Tuppurainen M Hannu T . Occupational Asthma Caused by Sculptured Nails Containing Methacrylates. Am J Ind Med (2008) 51(12):968–74. 10.1002/ajim.20633
17.
Buckley TM Schatzberg AF . On the Interactions of the Hypothalamic-Pituitary-Adrenal (HPA) axis and Sleep: Normal HPA axis Activity and Circadian Rhythm, Exemplary Sleep Disorders. The J Clin Endocrinol and Metab (2005) 90(5):3106–14. 10.1210/jc.2004-1056
18.
Shusterman D Lipscomb J Neutra R Satin K . Symptom Prevalence and Odor-Worry Interaction Near Hazardous Waste Sites. Environ Health Perspect (1991) 94:25–30. 10.1289/ehp.94-1567940
19.
Tjalvin G Hollund BE Lygre SHL Moen BE Bråtveit M . Subjective Health Complaints Among Workers in the Aftermath of an Oil Tank Explosion. Arch Environ and Occup Health (2015) 70(6):332–40. 10.1080/19338244.2014.918929
20.
Boor BE Spilak MP Laverge J Novoselac A Xu Y . Human Exposure to Indoor Air Pollutants in Sleep Microenvironments: A Literature Review. Building Environ (2017) 125:528–55. 10.1016/j.buildenv.2017.08.050
21.
Moher D Liberati A Tetzlaff J Altman DG Antes G Atkins D et al Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Revista Espanola de Nutricion Humana y Dietetica (2014) 18(3):172–81. 10.1136/bmj.b2535
22.
Morgan RL Whaley P Thayer KA Schünemann HJ . Identifying the PECO: A Framework for Formulating Good Questions to Explore the Association of Environmental and Other Exposures with Health Outcomes. Environ Int (2018) 121(Pt 1):1027–31. 10.1016/j.envint.2018.07.015
23.
Ma L-L Wang Y-Y Yang Z-H Huang D Weng H Zeng X-T . Methodological Quality (Risk of Bias) Assessment Tools for Primary and Secondary Medical Studies: What Are They and Which Is Better?Mil Med Res (2020) 7:7–11. 10.1186/s40779-020-00238-8
24.
Cohen J . A Coefficient of Agreement for Nominal Scales. Educ Psychol Meas (1960) 20(1):37–46. 10.1177/001316446002000104
25.
Higgins JP Thompson SG . Quantifying Heterogeneity in a Meta‐analysis. Stat Med (2002) 21(11):1539–58. 10.1002/sim.1186
26.
Higgins JP Thompson SG Deeks JJ Altman DG . Measuring Inconsistency in Meta-Analyses. Bmj (2003) 327(7414):557–60. 10.1136/bmj.327.7414.557
27.
Yu B Yuan Z Yu Z Xue-song F . BTEX in the Environment: An Update on Sources, Fate, Distribution, Pretreatment, Analysis, and Removal Techniques. Chem Eng J (2022) 435:134825. 10.1016/j.cej.2022.134825
28.
Page MJ McKenzie JE Bossuyt PM Boutron I Hoffmann TC Mulrow CD et al The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. Int J Surg (2021) 88:105906. 10.1016/j.ijsu.2021.105906
29.
Cho S-S Kang M-Y . Association between Occupational Exposure to Chemical or Physical Factors and Sleep Disturbance: An Analysis of the Fifth Korean Working Conditions Survey. Sleep Health (2022) 8(5):521–7. 10.1016/j.sleh.2022.06.004
30.
Lucas D Hervé A Lucas R Cabioch C Capellmann P Nicolas A et al Assessment of Exposure to Perchloroethylene and its Clinical Repercussions for 50 Dry-Cleaning Employees. J Occup Environ Hyg (2015) 12(11):767–73. 10.1080/15459624.2015.1048346
31.
Jay SM Gander PH Eng A Cheng S Douwes J Ellison-Loschmann L et al New Zealanders Working Non-standard Hours Also Have Greater Exposure to Other Workplace Hazards. Chronobiology Int (2017) 34(4):519–26. 10.1080/07420528.2017.1307850
32.
Gallicchio L Miller SR Greene T Zacur H Flaws JA . Somatic Symptoms Among Cosmetologists Compared to Women in Other Occupations. J Women's Health (2011) 20(4):605–15. 10.1089/jwh.2010.2342
33.
Tripathi S Bhattacharya S Chattopadhya P Kasityap S . Neurobehavioural Disturbances in Workers Engaged in High-Pressure Spray Painting. J Hum Ergology (1989) 18(2):191–8.
34.
Ng TP Ong S Lam W Jones G . Neurobehavioural Effects of Industrial Mixed Solvent Exposure in Chinese Printing and Paint Workers. Neurotoxicology and teratology (1990) 12(6):661–4. 10.1016/0892-0362(90)90082-n
35.
Escalona E Yanes L Feo O Maizlish N . Neurobehavioral Evaluation of Venezuelan Workers Exposed to Organic Solvent Mixtures. Am J Ind Med (1995) 27(1):15–27. 10.1002/ajim.4700270103
36.
Antti-Poika M . Prognosis of Symptoms in Patients with Diagnosed Chronic Organic Solvent Intoxication. Int Arch Occup Environ Health (1982) 51(1):81–9. 10.1007/BF00378413
37.
Laine A Savolainen K Riihimäki V Matikainen E Salmi T Juntunen J . Acute Effects of M-Xylene Inhalation on Body Sway, Reaction Times, and Sleep in Man. Int Arch Occup Environ Health (1993) 65(3):179–88. 10.1007/BF00381154
38.
Monstad P Mellgren S Sulg I . The Clinical Significance of Sleep Apnoea in Workers Exposed to Organic Solvents: Implications for the Diagnosis of Organic Solvent Encephalopathy. J Neurol (1992) 239(4):195–8. 10.1007/BF00839139
39.
Takeuchi Y Mabuchi C Takagi S . Polyneuropathy Caused by Petroleum Benzine. Internationales Archiv für Arbeitsmedizin (1975) 34(3):185–97. 10.1007/BF01371740
40.
Vouriot A Hannhart B Gauchard GC Barot A Ledin T Mur J-M et al Long-term Exposure to Solvents Impairs Vigilance and Postural Control in Serigraphy Workers. Int Arch Occup Environ Health (2005) 78(6):510–5. 10.1007/s00420-005-0609-7
41.
Godderis L Dours G Laire G Viaene M . Sleep Apnoeas and Neurobehavioral Effects in Solvent Exposed Workers. Int J Hyg Environ Health (2011) 214(1):66–70. 10.1016/j.ijheh.2010.08.006
42.
Kaukiainen A Hyvärinen HK Akila R Sainio M . Symptoms of Chronic Solvent Encephalopathy: Euroquest Questionnaire Study. Neurotoxicology (2009) 30(6):1187–94. 10.1016/j.neuro.2009.03.010
43.
Keer S Glass B Prezant B McLean D Pearce N Harding E et al Solvent Neurotoxicity in Vehicle Collision Repair Workers in New Zealand. Neurotoxicology (2016) 57:223–9. 10.1016/j.neuro.2016.10.005
44.
Kraut A Lilis R Marcus M Valciukas JA Wolff MS Landrigan PJ . Neurotoxic Effects of Solvent Exposure on Sewage Treatment Workers. Arch Environ Health An Int J (1988) 43(4):263–8. 10.1080/00039896.1988.10545947
45.
Lindelof B Almkvist O Göthe C-J . Sleep Disturbances and Exposure to Organic Solvents. Arch Environ Health An Int J (1992) 47(2):104–6. 10.1080/00039896.1992.10118762
46.
Monstad P Nissen T Sulg I Mellgren S . Sleep Apnoea and Organic Solvent Exposure. J Neurol (1987) 234(3):152–4. 10.1007/BF00314134
47.
Edling C Lindberg A Ulfberg J . Occupational Exposure to Organic Solvents as a Cause of Sleep Apnoea. Occup Environ Med (1993) 50(3):276–9. 10.1136/oem.50.3.276
48.
Thetkathuek A Jaidee W Saowakhontha S Ekburanawat W . Neuropsychological Symptoms Among Workers Exposed to Toluene and Xylene in Two Paint Manufacturing Factories in Eastern Thailand. Adv Prev Med (2015) 2015:183728. 10.1155/2015/183728
49.
Sağcan G Pıhtılı A Bingol Z Okumuş G Kıyan E . Sleep Apnea in Organic Solvent Exposed Workers. jtsm (2018) 5:67–72. 10.4274/jtsm.58077
50.
Heiskel H Gunzenhäuser D Seidler A Volk S Pflug B Kauppinen T et al Sleep Apnea and Occupational Exposure to Solvents. Scand J work, Environ and Health (2002) 28:249–55. 10.5271/sjweh.672
51.
Mandiracioglu A Akgur S Kocabiyik N Sener U . Evaluation of Neuropsychological Symptoms and Exposure to Benzene, Toluene and Xylene Among Two Different Furniture Worker Groups in Izmir. Toxicol Ind Health (2011) 27(9):802–9. 10.1177/0748233711399309
52.
Levy F . Clinical Features of Multiple Chemical Sensitivity. Scand J Work, Environ and Health (1997) 23 Suppl 3:69–73.
53.
Laire G Viaene M Veulemans H Masschelein R Nemery B . Nocturnal Oxygen Desaturation, as Assessed by Home Oximetry, in Long‐term Solvent‐exposed Workers. Am J Ind Med (1997) 32(6):656–64. 10.1002/(sici)1097-0274(199712)32:6<656::aid-ajim12>3.0.co;2-0
54.
Sekkal S Casas L Haddam N Bouhacina L Scheers H Taleb A et al Sleep Disturbances and Neurotoxicity in Workers Exposed to Hydrocarbons. An Observational Study from Algeria. Am J Ind Med (2016) 59(2):129–36. 10.1002/ajim.22561
55.
Lovas S Nagy K Sándor J Ádám B . Presumed Exposure to Chemical Pollutants and Experienced Health Impacts Among Warehouse Workers at Logistics Companies: A Cross-Sectional Survey. Int J Environ Res Public Health (2021) 18(13):7052. 10.3390/ijerph18137052
56.
Kaukiainen A Akila R Martikainen R Sainio M . Symptom Screening in Detection of Occupational Solvent-Related Encephalopathy. Int Arch Occup Environ Health (2009) 82(3):343–55. 10.1007/s00420-008-0341-1
57.
Ulfberg J Carter N Talback M Edling C . Occupational Exposure to Organic Solvents and Sleep-Disordered Breathing. Neuroepidemiology (1997) 16(6):317–26. 10.1159/000109704
58.
Saygun M Ekici A Muluk NB Çakmak A Pinar T Dağ E et al Effects of Long-Term Low-Level Solvent Exposure on Cognitive Function. Clin Invest Med (2012) 35:E190–E205. 10.25011/cim.v35i4.17148
59.
Kellerova V . Electroencephalographic Findings in Workers Exposed to Benzene. J Hyg Epidemiol Microbiol Immunol (1985) 29(4):337–46.
60.
Indulski J Sińczuk-Walczak H Szymczak M Wesołowski W . Neurological and Neurophysiological Examinations of Workers Occupationally Exposed to Organic Solvent Mixtures Used in the Paint and Varnish Production. Int J Occup Med Environ Health (1996) 9(3):235–44.
61.
Kiesswetter E Seeber A Golka K Sietmann B . Solvent Exposure, Shiftwork, and Sleep. Int J Occup Environ Health (1997) 3(Suppl. 2):S61–S66.
62.
Takeuchi Y Nishizaki T Takagi S Mabuchi C . Diencephalic Syndrome in Two Workers Exposed Mainly to Toluene Vapour. Jpn J Ind Health (1972) 14(6):563–71.
63.
Shamsudin S Kamaludin NF Sazali NM Awang N Ithnin A . Indoor Air Quality Assessment in the Office of the Transformer Manufacturing Factory in Selangor, Malaysia. Malaysian J Med and Health Sci (2023) 19(5):24–31. 10.47836/mjmhs.19.5.5
64.
Viaene M Vermeir G Godderis L . Sleep Disturbances and Occupational Exposure to Solvents. Sleep Med Rev (2009) 13(3):235–43. 10.1016/j.smrv.2008.07.003
65.
McNicholas WT Tarlo S Cole P Zamel N Rutherford R Griffin D et al Obstructive Apneas during Sleep in Patients with Seasonal Allergic Rhinitis. Am Rev Respir Dis (1982) 126(4):625–8. 10.1164/arrd.1982.126.4.625
66.
Zheng M Wang X Ge S Gu Y Ding X Zhang Y et al Allergic and Non-allergic Rhinitis Are Common in Obstructive Sleep Apnea but Not Associated with Disease Severity. J Clin Sleep Med (2017) 13(8):959–66. 10.5664/jcsm.6694
67.
Sunderram J Weintraub M Black K Alimokhtari S Twumasi A Sanders H et al Chronic Rhinosinusitis Is an Independent Risk Factor for OSA in World Trade Center Responders. Chest (2019) 155(2):375–83. 10.1016/j.chest.2018.10.015
68.
Riemann D Spiegelhalder K Feige B Voderholzer U Berger M Perlis M et al The Hyperarousal Model of Insomnia: A Review of the Concept and its Evidence. Sleep Med Rev (2010) 14(1):19–31. 10.1016/j.smrv.2009.04.002
69.
Steinheider B . Environmental Odours and Somatic Complaints. Zentralblatt für Hyg Umweltmedizin (1999) 202(2-4):101–19. 10.1016/s0934-8859(99)80011-x
70.
Sucker K Both R Winneke G . Review of Adverse Health Effects of Odours in Field Studies. Water Sci Technology (2009) 59(7):1281–9. 10.2166/wst.2009.113
71.
Shusterman D . Odor-associated Health Complaints: Competing Explanatory Models. Chem senses (2001) 26(3):339–43. 10.1093/chemse/26.3.339
72.
Virtanen M Ferrie JE Gimeno D Vahtera J Elovainio M Singh-Manoux A et al Long Working Hours and Sleep Disturbances: The Whitehall II Prospective Cohort Study. Sleep (2009) 32(6):737–45. 10.1093/sleep/32.6.737
73.
Dregan A Armstrong D . Cross-country Variation in Sleep Disturbance Among Working and Older Age Groups: An Analysis Based on the European Social Survey. Int psychogeriatrics (2011) 23(9):1413–20. 10.1017/S1041610211000664
74.
Kessler RC Berglund PA Coulouvrat C Hajak G Roth T Shahly V et al Insomnia and the Performance of US Workers: Results from the America Insomnia Survey. Sleep (2011) 34(9):1161–71. 10.5665/SLEEP.1230
75.
Bertrais S André N Béque M Chastang JF Niedhammer I . Associations between Multiple Occupational Exposures and Sleep Problems: Results from the National French Working Conditions Survey. J Sleep Res (2021) 30(3):e13101. 10.1111/jsr.13101
76.
Blackman A Harrington W . The Use of Economic Incentives in Developing Countries: Lessons from International Experience with Industrial Air Pollution. The Theor Pract Command Control Environ Policy (2018) 199–238. 10.4324/9781315197296-9
77.
Zhang Y Mu Y Liu J Mellouki A . Levels, Sources and Health Risks of Carbonyls and BTEX in the Ambient Air of Beijing, China. J Environ Sci (China) (2012) 24(1):124–30. 10.1016/s1001-0742(11)60735-3
78.
Matsunaga I Miyake Y Yoshida T Miyamoto S Ohya Y Sasaki S et al Ambient Formaldehyde Levels and Allergic Disorders Among Japanese Pregnant Women: Baseline Data from the Osaka Maternal and Child Health Study. Ann Epidemiol (2008) 18(1):78–84. 10.1016/j.annepidem.2007.07.095
79.
Zhou C Baïz N Banerjee S Charpin DA Caillaud D de Blay F et al The Relationships between Ambient Air Pollutants and Childhood Asthma and Eczema Are Modified by Emotion and Conduct Problems. Ann Epidemiol (2013) 23(12):778–83. 10.1016/j.annepidem.2013.09.004
80.
Pénard-Morand C Raherison C Charpin D Kopferschmitt C Lavaud F Caillaud D et al Long-term Exposure to Close-Proximity Air Pollution and Asthma and Allergies in Urban Children. Eur Respir J (2010) 36(1):33–40. 10.1183/09031936.00116109
81.
Gupta SB Gupta A Shah B Kothari P Darall S Boghara D et al Hand Eczema in Nurses, Nursing Auxiliaries and Cleaners—A Cross-Sectional Study from a Tertiary Hospital in Western India. Contact Dermatitis (2018) 79(1):20–5. 10.1111/cod.13009
82.
Park DW Kim SH Moon JY Song JS Choi J Kwak HJ et al The Effect of Low-Volatile Organic Compounds, Water-Based Paint on Aggravation of Allergic Disease in Schoolchildren. Indoor Air (2017) 27(2):320–8. 10.1111/ina.12301
83.
Xin Z Tsuda T Doi H . Evaluating the Effects of Air Pollution from a Plastic Recycling Facility on the Health of Nearby Residents. Acta Med Okayama (2017) 71(3):209–17. 10.18926/AMO/55203
84.
Ricklund N Bryngelsson I-L Hagberg J . Self-reported Symptoms in Swedish Hairdressers and Association with Exposure to Volatile Organic Compounds (VOCs), Including Aldehydes. BMC Public Health (2023) 23(1):1576. 10.1186/s12889-023-16446-5
85.
Mendes A Madureira J Neves P Carvalhais C Laffon B Teixeira JP . Chemical Exposure and Occupational Symptoms Among Portuguese Hairdressers. J Toxicol Environ Health A (2011) 74(15-16):993–1000. 10.1080/15287394.2011.582027
86.
Mancuso G Reggiani M Berdondini RM . Occupational Dermatitis in Shoemakers. Contact Dermatitis (1996) 34(1):17–22. 10.1111/j.1600-0536.1996.tb02105.x
87.
Herbarth O Fritz GJ Rehwagen M Richter M Röder S Schlink U . Association between Indoor Renovation Activities and Eczema in Early Childhood. Int J Hyg Environ Health (2006) 209(3):241–7. 10.1016/j.ijheh.2006.01.003
88.
Choi HS Suh MJ Hong SC Kang JW . The Association between the Concentration of Heavy Metals in the Indoor Atmosphere and Atopic Dermatitis Symptoms in Children Aged between 4 and 13 Years: A Pilot Study. Children (2021) 8(11):1004. 10.3390/children8111004
89.
Ha EK Kim JH Park D Lee E Lee SW Jee HM et al Personal Exposure to Total VOC Is Associated with Symptoms of Atopic Dermatitis in Schoolchildren. jkms (2022) 37(8):e63–0. 10.3346/jkms.2022.37.e63
Summary
Keywords
systematic review, meta-analysis, sleep, occupational exposure, VOCs
Citation
Khoshakhlagh AH, Yazdanirad S, Drake C, Iqal J and Bui D (2025) Associations Between Occupational Exposures to Volatile Organic Compounds (VOCs) and Sleep Problems. Public Health Rev. 46:1608224. doi: 10.3389/phrs.2025.1608224
Received
06 December 2024
Accepted
04 September 2025
Published
25 September 2025
Volume
46 - 2025
Edited by
Samantha Morais, ICES, Canada
Reviewed by
Two reviewers who chose to remain anonymous
Updates
Copyright
© 2025 Khoshakhlagh, Yazdanirad, Drake, Iqal and Bui.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms. PHR is edited by the Swiss School of Public Health (SSPH+) in a partnership with the Association of Schools of Public Health of the European Region (ASPHER)+
*Correspondence: Saeid Yazdanirad, saeedyazdanirad@gmail.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.