Abstract
Objectives:
Comprehensively map and summarize digital health initiatives for the elderly and caregivers.
Methods:
Scoping review between April and May 2022 based on Joanna Briggs methodology. Databases used included PubMed, Cochrane Library, CINAHL Plus, and Web of Science, along with grey literature and hand searches. Two reviewers independently conducted screening and eligibility phases, with a third resolving disagreements. Data were thematically analyzed.
Results:
The review included 421 documents. Most documents were published between 2013 and 2022, with a recent increase. Most studies, originating from high-income countries, focused on home applications and were mainly in the testing and validation stages. Telephones and computers were the predominant devices. Health objectives included monitoring, prevention, and treatment, with interventions utilizing directed communication and personal health monitoring for individuals, and telemedicine and decision support for healthcare providers.
Conclusion:
Increasing integration of technology in older adults’ lives, along with their increasing proficiency, is driving a significant rise in digital health interventions. Despite this growth, further research in middle- and low-income countries, for caregivers and evaluating effectiveness and feasibility of these technological interventions is needed.
Introduction
Population aging is a worldwide phenomenon, and it is estimated that by 2050, two billion people will be 60 years of age and older (22% of the population). Eighty percent of them will be living in low- and middle-income countries [1].
Population aging signifies improved living conditions and health status in countries; however, it also presents a series of health and social challenges that need to be addressed. Moreover, due to physical and functional limitations, some elderly individuals require a caregiver, a key figure who provides care, makes decisions, and connects them with the healthcare system [2–4].
When examining equity in healthcare access, disparities become evident as certain populations encounter unmet health needs due to factors such as limited-service availability, administrative and cultural barriers, substandard service quality, high costs, and extended waiting times. The implementation of digital health technologies can partially alleviate these disparities by enhancing the interaction between healthcare providers and the population [5].
Digital health is defined as “the use of information and communication technology (ICT) in support of health and related areas” [5]. Technologies provide concrete opportunities to address health system challenges and offer possibilities to improve access, coverage and quality of services [6]. Their use, especially in low-resource settings, could enable progress toward universal health coverage (UHC), with a more equitable and resource-efficient model of care [7].
Digital health technologies have emerged as a significant area of development and research aimed at addressing various health needs [5]. In 2018, the World Health Assembly formally recognized their potential in advancing towards Universal Health Coverage (UHC). In its resolution [8], the Assembly called upon health ministries to evaluate the use of digital health technologies and prioritize their development, assessment, implementation, scaling up, and increased use. Furthermore, the resolution tasked the World Health Organization (WHO) with providing policy guidance in this field [5].
The utilization of digital health technologies has been extensively acknowledged for its applicability across various target groups, including patients, healthcare professionals, and decision-makers. This technology encompasses a broad range of functionalities such as electronic health records, emergency alert systems, fall detection sensors, and remote patient monitoring, all of which are continually advancing due to the dynamic nature of the field [5].
The SARS-CoV-2 pandemic has notably accelerated the adoption and development of health technologies. However, there is a pressing need for systematic evidence, particularly regarding vulnerable populations like the elderly, to inform effective development and implementation strategies. Seniors possess diverse healthcare needs but frequently encounter difficulties in utilizing these technologies. Therefore, it is crucial to design digital health solutions that are user-friendly and tailored to their specific needs and preferences, ensuring that healthcare services remain accessible, efficient, and effective. Digital health innovations can enhance care quality for seniors by improving service delivery, optimizing data management, and facilitating better communication between patients and healthcare providers [5, 9].
The aim of this scoping review is to comprehensively map and summarize digital health initiatives, strategies, programs, innovations or policies for the elderly or their caregivers.
Methods
The scoping review was conducted following the Joanna Briggs Institute (JBI) Guidance for conducting systematic scoping reviews [10] and the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) [11].
Review Question
What initiatives, strategies, programs, innovations, or digital health policies are aimed at older adults or their caregivers?
Inclusion Criteria
The inclusion criteria were formulated based on the components of the Population, Concept, and Context (PCC) framework as outlined by the JBI [
10]:
− Population: elderly or their caregivers (formal and informal). Elderly is defined as individuals at a stage of life characterized by biological, psychological, and social changes associated with aging. For this study, the population aged 60 years and older was considered, in accordance with the definition established by the World Health Organization [12].
− Concept: the core topic or phenomenon of interest are digital health initiatives, strategies, programs, innovations, policies, oriented to older people or their caregivers. Digital health is understood as “the use of information and communication technology in support of health and related areas.” They are considered those with which the elderly person or caregiver interacts, or that fulfill the function of being a facilitator in their daily life related to some area of health.
− Context: regarding geographic location and specific settings, the scoping considers initiatives implemented in any country or setting, including hospitals, primary care facilities, community health services, elder care centers and residences, other healthcare services, private homes, and both rural and urban settings.
Exclusion Criteria
Documents were excluded if they were interviews, opinion letters, or other types that did not contain their own methods and results; related exclusively at other age groups, surgical practices or pathology diagnosis; inquired exclusively into aspects of acceptability (i.e., the degree to which population or specific social groups accept the technology and the factors that increase or decrease the likelihood of their use); contained terms as ICT (which is not the subject of this review: intensive chemotherapy, intracranial tumors, Islamabad Capital Territory, among others); were clinical trial protocols, or only described the technology (or its development) without having been tested or used by elderly or caregivers.
Included terms like ICT (that, in our context, means Information and Communication Technology) with meanings unrelated to this review, such as “intensive chemotherapy,” “intracranial tumors,” or “Islamabad Capital Territory,” were excluded. This approach allowed to comprehensively capture studies aligned with our focus while filtering out unrelated documents using the same acronym.
Databases and Search Strategy
The following biomedical data sources were consulted: PubMed (NCBI), CINAHL Plus with Full Text (EBSCO), Academic Search Ultimate (EBSCO), Cochrane Library (free access by Ministry of Health, Chile), Rehabilitation and Sports Medicine (EBSCO), Web of Science (Clarivate), Scielo.org and Emerald.
Also, grey literature (manuals, technical documents, scientific conference reports and conference presentations) was reviewed in World Health Organization and Pan American Health Organization.
Finally, a hand search was performed in OpenAire/Explore, Working with Older People, Smart Homecare Technology and TeleHealth, Journal of Assistive Technologies and Quality in Ageing and Older Adults and Google Scholar.
To identify relevant studies, a seasoned biomedical librarian (AJ) and four researchers specialized in public health and epidemiology (XM, MTA, MM, and MHA) conducted a comprehensive literature search following the stages recommended by the JBI [13].
Firstly, an initial pilot study search was conducted in PubMed (MHA and AJ) using keywords and Medical Subject Headings (MeSH) terms associated with “elderly,” “frail,” “senior,” “frail elderly,” “digital health,” “e-Health,” “telemedicine,” “telehealth,” “digital therapeutics,” “virtual medicine,” “information and communication technology,” “ICT,” “silver economy,” “mhealth,” “mobile application.” In this study, MeSH terms were not used in the final search as they did not effectively discriminate between relevant and non-relevant articles. Instead, free terms were utilized in the titles and abstracts of the documents, allowing for a more precise and targeted search. This approach detected a broader range of relevant studies and sought to ensure no pertinent research was overlooked. Using free terms refined the search criteria to better match the specific context and nuances of the research focus.
The search strategy was implemented across additional databases to ensure the results aligned consistently with the research question. Subsequently, the keywords identified from the relevant articles in the initial search were utilized to formulate a comprehensive and planned search strategy (Appendix search strategy).
A language filter was applied to include documents in English, French, Portuguese, and Spanish, and only studies in humans were included. There was no restriction by publication year. Finally, a review of the references of the included documents was conducted.
The search was conducted from 4 to 15 April 2022, for indexed literature, and 25 April to 26 May 2022, for grey literature and hand search. Reference management software was used to organize the reference database. Additionally, the search results were managed in Microsoft Excel v.2108, with separate sheets created for the search and review processes.
The titles and abstracts of the documents obtained from the identification phase were screened, selecting those to be reviewed in full text during the eligibility phase. Each document, at both stages, was reviewed by two independent researchers, and disagreements were resolved by a third reviewer, all from the research team (IM, CCL, AJ, CA, AO, PR, XM, MM, MHA, OU, TA, FS, and SE). Most of the reviewers have extensive experience in public health research, epidemiology, and literature reviews.
Full text was searched through open access, by requesting assistance from the Biomedical Library of our university or asking directly from the authors. The entire selection process was diagrammed in a flow chart identifying each stage (identification, screening, and eligibility) (Figure 1).
FIGURE 1
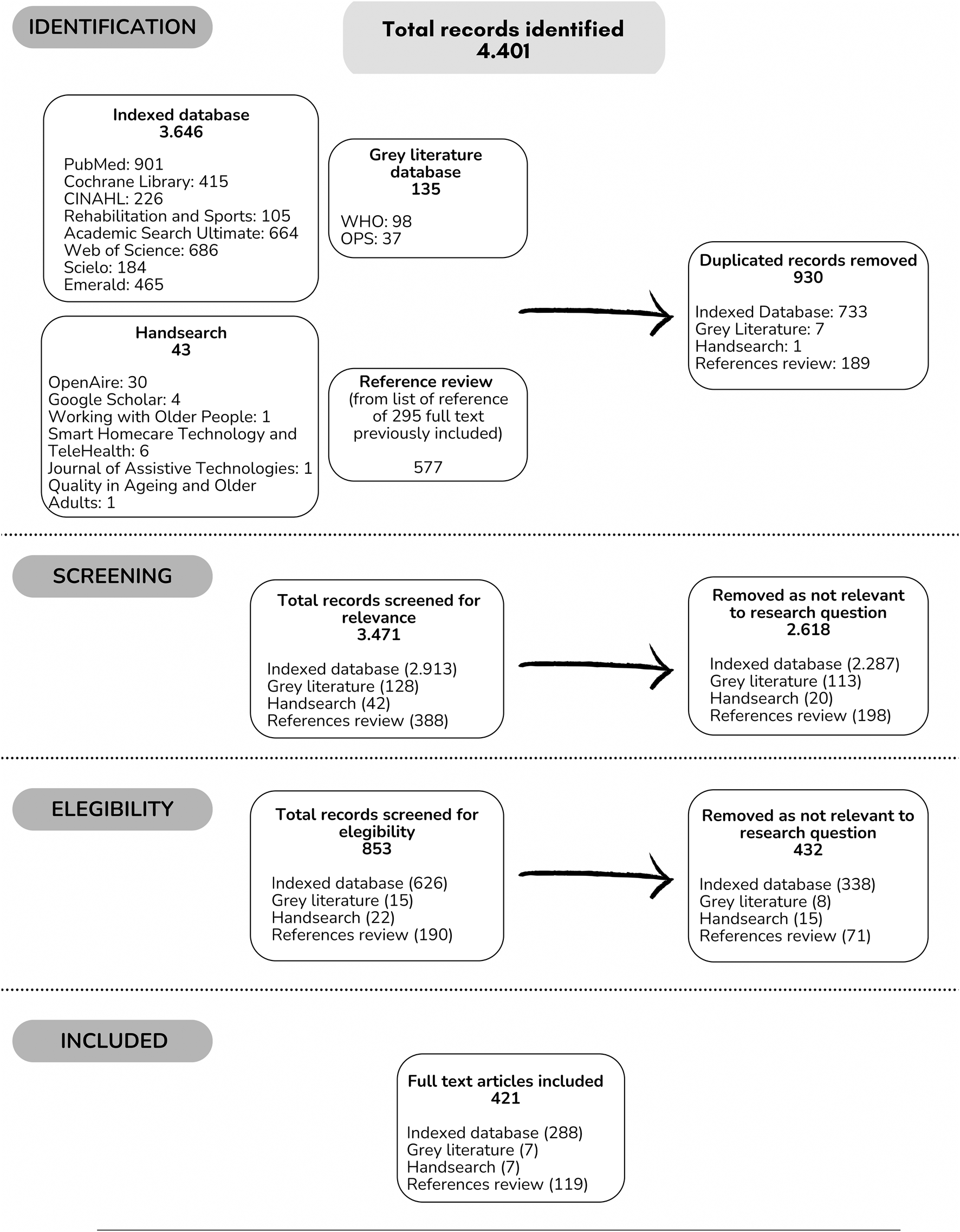
Flowchart of study selection according to scoping review process (Worldwide, 2022).
Data Extraction
Data extraction from the selected studies followed the methodology outlined by Peters et al. [13]. The research team initially piloted and implemented the extraction process, testing the designed matrix and refining it based on received feedback. This approach facilitated the standardization of criteria for the final data extraction. Upon completion, six researchers (CCL, CA, AO, XM, IM, MHA) reviewed this phase, validating the information extracted from the documents and adjusting as needed.
Data were compiled in a single spreadsheet (Supplementary Material), containing the articles’ main characteristics, along with specific aspects of the review question. Data extraction categories included a detailed overview of each study’s bibliographic information, context, objectives, research design, outcomes, and key findings related to this scoping review [10]. To classify digital health interventions, the WHO’s classification of interventions, services, and applications in health was used [14], and was considered those aimed at person and healthcare providers. Three stages were considered for the level of technological development: conceptualization and design (focus on the generation and initial formulation of the intervention, ranging from the initial idea to the design of a functional prototype), testing and validation (includes pilot tests and clinical evaluations aimed at testing the intervention in controlled settings or with small groups to validate its efficacy, usability, and safety), and implementation and scaling (cover both small and large-scale implementation, commercialization, and post-implementation evaluation, focusing on bringing the intervention into wider use and evaluating its impact and effectiveness in real-world, long-term settings) [15].
Analysis and Presentation of Results
Data from the selected studies and documents were synthesized by four researchers (CCL, CA, XM, MHA) through an iterative process, according to the research question.
Results
Overview
A total of 4,401 records were identified, obtaining 3,471 (78.8%) after eliminating duplicates. Those 3,471 were reviewed in title and abstract (screening). Of them, 853 (24.6%) were selected to continue with the full-text review (eligibility). Finally, 421 (49.4%) documents were included in the analysis and came from: indexed databases 288 (68.4%); grey literature 7 (1.7%); hand search 7 (1.7%) and references review 119 (28.3%) [3, 4, 16–434].
When categorized according to indexed articles or grey literature, 97.6% (n = 411) and 2.4% (n = 10) were identified, respectively. Documents published from 1988 to 2022 (the year the review was in progress), with almost 90% of the publications since 2008 (Table 1).
TABLE 1
| Characteristic of included documents (n = 421)* | ||
|---|---|---|
| Characteristic | N | % |
| Publication year | ||
| 1988–2002 | 13 | 3.1 |
| 2003–2007 | 33 | 7.8 |
| 2008–2012 | 86 | 20.4 |
| 2013–2017 | 136 | 32.3 |
| 2018–2022 | 153 | 36.3 |
| Publication type | ||
| Indexed (n = 411) | ||
| Research article | 398 | 96.8 |
| Congress abstract | 8 | 1.9 |
| Poster | 1 | 0.2 |
| PhD thesis | 1 | 0.2 |
| Special communication | 2 | 0.5 |
| Dissertation | 1 | 0.2 |
| Grey literature (n = 10) | ||
| Technical report | 6 | 60.0 |
| Recommendations | 2 | 20.0 |
| Country report | 1 | 10.0 |
| Position paper | 1 | 10.0 |
| Study design (n = 411) | ||
| Clinical trials, Experimental and Quasi experimental | 210 | 51.1 |
| Report, review or discussion article | 33 | 8.0 |
| Systematic review (with or without metanalisis) and scoping review | 27 | 6.6 |
| Case series | 26 | 6.3 |
| Cross-sectional study | 25 | 6.1 |
| Literature review or Narrative review | 25 | 6.1 |
| Cohort study | 17 | 4.1 |
| Mixed method | 15 | 3.6 |
| Qualitative study | 12 | 2.9 |
| Case-control study | 9 | 2.2 |
| Observational not specified | 6 | 1.5 |
| Othera | 6 | 1.5 |
| Corresponding author sex (n = 411) | ||
| Female | 194 | 47.2 |
| Male | 217 | 52.8 |
Summary of characteristics of the included documents (Worldwide, 2022).
For the 411 indexed articles, the sex of the corresponding author and the study design were recorded. Grey literature was excluded from this analysis due to the nature of the authorships and the type of scientific communication. In this regard, it was found that 47.3% (n = 194) of the corresponding authors were female. About the study design, 51.1% (n = 210) were clinical trials or experimental and 20.2% (n = 83) were observational (Table 1).
Population
The interventions were primarily aimed at the elderly population (93.3%, n = 393), followed by healthcare professionals (48.0%, n = 202), and caregivers (33.0%, n = 139). Among the interventions focused on caregivers, the most studied group were family or informal caregivers (52.5%, n = 73) (Table 2).
TABLE 2
| Characteristic of included documents (n = 421)* | ||
|---|---|---|
| Characteristic | N | % |
| Population | ||
| Elderly | 393 | 93,3 |
| Healthcare professionals | 202 | 48,0 |
| Caregivers (n = 139) | ||
| Family/Informal | 73 | 52,5 |
| Formal | 52 | 37,4 |
| Not specified | 54 | 38,8 |
| Disease or condition | ||
| Chronic disease (hypertension, diabetes, cancer, obesity, chronic obstructive pulmonary disease, chronic pain, musculoskeletal, etc.) | 218 | 51,8 |
| Fragility (low grip strength, falls, balance disorders, etc.) | 114 | 27,1 |
| Neurological (Alzheimer’s, dementia, etc.) | 101 | 24,0 |
| Mental health (depression, anxiety, social isolation, loneliness, etc.) | 75 | 17,8 |
| Healthy ageing and quality of life | 55 | 13,1 |
| Othera | 21 | 5,0 |
| Sensory impairment | 8 | 1,9 |
| Infectious disease | 6 | 1,4 |
| Context | ||
| Region of Country (World Bank Region) | ||
| Europe and Central Asia | 149 | 35,4 |
| North America | 114 | 27,1 |
| East Asia and Pacific | 78 | 18,5 |
| Otherb | 22 | 5,2 |
| Middle East and North Africa | 6 | 1,4 |
| Latin America and the Caribbean | 5 | 1,2 |
| Sub-Saharan Africa | 3 | 0,7 |
| South Asia | 1 | 0,2 |
| Worldwide | 39 | 9,3 |
| Not specified | 4 | 1,0 |
| Income of Country (World Bank Income) | ||
| High | 337 | 80,0 |
| Upper-middle | 28 | 6,7 |
| Lower-middle | 4 | 1,0 |
| Low | 1 | 0,2 |
| Otherc | 8 | 1,9 |
| Worldwide | 39 | 9,3 |
| Not specified | 4 | 1,0 |
| Setting | ||
| Home | 320 | 76,0 |
| Nursing home (Retirement home, Community care Veterans’ home, Senior living centers, Day care) | 120 | 28,5 |
| Healthcare facility | 111 | 26,4 |
| Otherd | 13 | 3,1 |
| Healthcare level (n = 111) | ||
| Primary | 71 | 64,0 |
| Secondary | 61 | 55,0 |
| Tertiary | 53 | 47,7 |
| Concept | ||
| Health objective of the digital tool | ||
| Monitoring or follow-up | 265 | 62,9 |
| Prevention | 201 | 47,7 |
| Therapy or treatment | 200 | 47,5 |
| Promotion | 86 | 20,4 |
| Diagnosis | 80 | 19,0 |
| Rehabilitation | 70 | 16,6 |
| Digital health interventions for persons | ||
| Targeted communication to Persons | 259 | 61,5 |
| Personal health tracking | 190 | 45,1 |
| On demand communication with persons | 97 | 23,0 |
| Person to Person communication | 81 | 19,2 |
| Othere | 38 | 9,0 |
| Digital health interventions for healthcare providers | ||
| Telemedicine | 239 | 56,8 |
| Healthcare provider decision support | 200 | 47,5 |
| Prescription and medication management | 113 | 26,8 |
| Referral coordination | 78 | 18,5 |
| Otherf | 13 | 3,1 |
| Healthcare technologies results | ||
| Positive | 366 | 86,9 |
| No differences | 36 | 8,6 |
| Partially positive | 11 | 2,6 |
| Negative | 8 | 1,9 |
| Type of digital health tools | ||
| Hardware or physical devices | ||
| Telephone (cell phone, smart phone, landline phone) | 216 | 51,3 |
| Desktop or laptop computer | 166 | 39,4 |
| Wearable activity monitors (wrist-worn devices, or step counters) | 98 | 23,3 |
| Tablet | 91 | 21,6 |
| Sensors and positioning system | 89 | 21,1 |
| Video game consoles, exergames, balance board, dance mat, handheld remotes, fitness board, buzz controller, force platforms, cameras with gesture recognition, virtual environment non-immersive and immersive | 55 | 13,1 |
| Telehealth devices (with or without health measurement) | 50 | 11,9 |
| Otherg | 37 | 8,8 |
| Interactive TV | 34 | 8,1 |
| Robots, social robots, robotic rollators, industrial and service robots, assistive telepresence robot | 11 | 2,6 |
| Radio RX/TX with interaction | 2 | 0,5 |
| Software, platforms | ||
| Videoconference platforms | 153 | 36,3 |
| Text/Audio Messaging (SMS, Chat, etc.) | 110 | 26,1 |
| Digital health portals | 91 | 21,6 |
| Health and fitness apps | 81 | 19,2 |
| Video game | 63 | 15,0 |
| Electronic mail | 50 | 11,9 |
| Digital community or groups | 35 | 8,3 |
| Otherh | 34 | 8,1 |
Summary of characteristics of included documents according to PCC model (Population, Context, Concept) (Worldwide, 2022).
*[3, 4, 16–434].
aMedication problems, acute illnesses, nutrition and dietary status, specific pathologies, medical and hospital care, and health awareness and education.
bCombination of region.
cCombination of high/upper-middle and high/upper-middle/lower middle.
dPublic transportation, hospital at home, community centers, day care center, university, outpatient rehabilitation sports club, welfare centers, Aware Home Research Initiative (AHRI) at the Georgia Institute of Technology is a facility designed to facilitate research, while providing an authentic home environment.
eDigital therapeutics based on: therapies based on virtual technology and games, home-based exercise and rehabilitation programs, guided and personalized therapies, interventions based on robotics, emotional support and communication, medical devices and telemedicine applications.
fHealthcare provider training, Healthcare provider communication, Person-centered health records, Laboratory and Diagnostics Imaging Management, Scheduling and activity planning for healthcare providers, Person-Centered Health Records, Professional advisory roles.
gCommunication Devices, Recording Devices and Cameras, Emergency and Alarm Systems, Reminders, Virtual and Augmented Reality Devices, Storage and Playback Devices, Personal Devices.
hRecords and data management software or platforms, interactive and cognitive assistants, telephone services, websites and online platforms, exercise and educational content.
Twenty documents focused exclusively on interventions for healthcare professionals. These interventions included teleophthalmology, emergency triage, cognitive assessments and development of technologies for care and tele-rehabilitation systems. Other areas addressed include reducing emergency admissions, using wearable devices for health monitoring, supporting caregivers with digital tools, and adapting tele-neuropsychology for the COVID-19 pandemic.
Only five documents focused specifically on caregivers. These studies examined the effectiveness of a platform to enhance caregiver competence, satisfaction, and coping abilities, identified mobile apps for caregivers, and outlined best practices from successful interventions. They also analyzed psychosocial interventions using technology, examined web-based interventions, focusing on their development, delivery, and impact on caregiver health outcomes. Additionally, they explored how technology can improve caregivers’ quality of life.
Chronic diseases were the most studied condition, accounting for 51.8% (n = 218) of the total, with hypertension, diabetes, obesity, chronic obstructive pulmonary disease, chronic pain, and joint issues being the most common. Fragility-related issues, including low grip strength, falls, and balance disorders, were the focus of 27.1% (n = 114) of studies. Neurological conditions, such as Alzheimer’s and dementia were examined in 24.0% (n = 101) of the cases. Mental health including depression, anxiety, social isolation, and loneliness comprised 17.8% (n = 75). Studies on healthy ageing and quality of life made up 13.1% (n = 55) of the total. Less than 2% of the studies focused on sensory impairment and infectious disease, respectively (Table 2).
Other conditions were accounted for in 5.0% (n = 21) of the studies and were related to medication problems, acute illnesses, nutrition and dietary status, specific pathologies, medical and hospital care, health awareness and education.
Context
The studied countries classified by income and region according to the World Bank [435], are presented in Table 2. Of the total of 421 records, it was possible to classify 378 documents (89.8%), the rest did not specify countries (1.0%, n = 4) or referred to the world level (9.3%, n = 39).
When analyzing income, 80.0% (n = 337) were from high-income countries (HIC), 6.7% (n = 28) from upper-middle-income economies (UMIC), 1.0% (n = 4) from lower-middle-income (LMIC), and only 0.2% (n = 1) from low-income countries (LIC). A 1.9% (n = 8) were a combination of high/upper-middle and high/upper-middle/lower middle.
The most studied regions, accounting for 62.5%, with Europe and Central Asia (35.4%, n = 149), and North America (27.1%, n = 114), followed by East Asia and Pacific (18.5%, n = 78).
It was also studied whether the technology was applied at home, in care centers and residences for the elderly, healthcare facilities or other places. It was found that 76,0% (n = 320) declared a home context, 28.5% (n = 120) care centers and residences for the elderly, 26.4% (n = 111) healthcare facilities and 3.1% (n = 13) others (public transportation, hospital at home, community centers, university, outpatient rehabilitation sports club, welfare centers and a facility designed to research providing an authentic home environment).
Of those who studied a healthcare facility (n = 111), it was found that the level of healthcare corresponded to 64.0% (n = 71) primary, 55.0% (n = 61) secondary and 47.7% (n = 53) tertiary.
Concept
Despite the diverse methodologies and study designs in the reviewed documents, the reported results related to the use of healthcare technologies were predominantly positive (86.9%, n = 366). Additionally, 11% (n = 47) reported no differences or partially positive results, and only 1.9% (n = 8) negative results (Table 2).
When analyzing the level of technological development, 97.4% (n = 410) of the documents indicated some level. Specifically, 18.8% (n = 79) were at the conceptualization and design stage, 69.1% (n = 291) were in testing and validation, and 25.9% (n = 109) were in the implementation and scalability stage. Documents reporting multiple levels of development were mostly reviews (Table 2).
In relation to the health objective sought by the technological tool, it was found that 62.9% (n = 265) addressed monitoring/follow-up; 47.7% (n = 201) prevention; 47.5% (n = 221) treatment; 20.4% (n = 86) promotion; 19.0% (n = 80) diagnosis, and 16.6% (n = 70) rehabilitation (Table 2).
By classifying digital health interventions, services, and applications in health, of the 421 documents, 61.5% (n = 259) focused on targeted communication to persons; 45.1% (n = 190) on personal health tracking; 23.0% (n = 97) on demand communication with persons; 19.2% (n = 81) on person-to-person communication; and 9.0% (n = 38) on other categories. This last category includes digital therapeutics based on virtual technology and games, home-based exercise and rehabilitation programs, guided and personalized therapies, interventions based on robotics, emotional support and communication, and medical devices and telemedicine applications. Of those interventions aimed at healthcare providers, 56.8% (n = 239) were related to telemedicine; 47.5% (n = 200) to healthcare provider decision support; 26.8% (n = 113) to prescription and medication management; 18.5% (n = 78) to referral coordination and 3.1% (n = 13) to other classifications. The latter category considered healthcare provider training, healthcare provider communication, person-centered health records, laboratory and diagnostics imaging management, scheduling and activity planning for healthcare providers, person-centered health records, professional advisory roles (Table 2).
The type of technology related to hardware and software was analyzed. Regarding hardware, 51.3% (n = 216) referred to telephone (cell phone, smart phone, landline phone); 39.4% (n = 166) to desktop or laptop computer; similar proportions (close to 20%) were found for wearables (wrist-worn devices or step counters); Tablet and sensors and positioning system. Less than 15% was found for video game consoles (exergames, balance board, dance mat), interactive TV, robots (social robots, robotic rollators, assistive telepresence robot), and radio RX/TX with interaction. Telehealth devices (with or without health measurement) were found on 11.9% (n = 50). On the other category was found communication and recording devices, cameras, emergency and alarm systems, reminders, storage and playback devices (Table 2).
In terms of software, it was found that the most widely used was videoconference platforms with 36.6% (n = 153); followed by text/audio messaging with 26.1% (n = 110); digital health portals with 21.6% (n = 91), and less than 20% each of the following: health and fitness apps, video games, email, and digital community or groups. In the other category was found records and data management software or platforms interactive and cognitive assistants telephone services websites and online platforms, exercise and educational content (Table 2).
In relation to the health objective and the condition under study, for chronic diseases, the most prevalent objective was treatment (76.1%), for fragility was prevention (63.2%), whereas for infectious diseases, it is monitoring/follow-up (83.3%). Meanwhile, prevention and monitoring/follow-up highlight their primary objective in the case of healthy aging and quality of life (69.1% and 60.0%, respectively). The category named other is not described due to the diversity of situations. Figure 2.
FIGURE 2
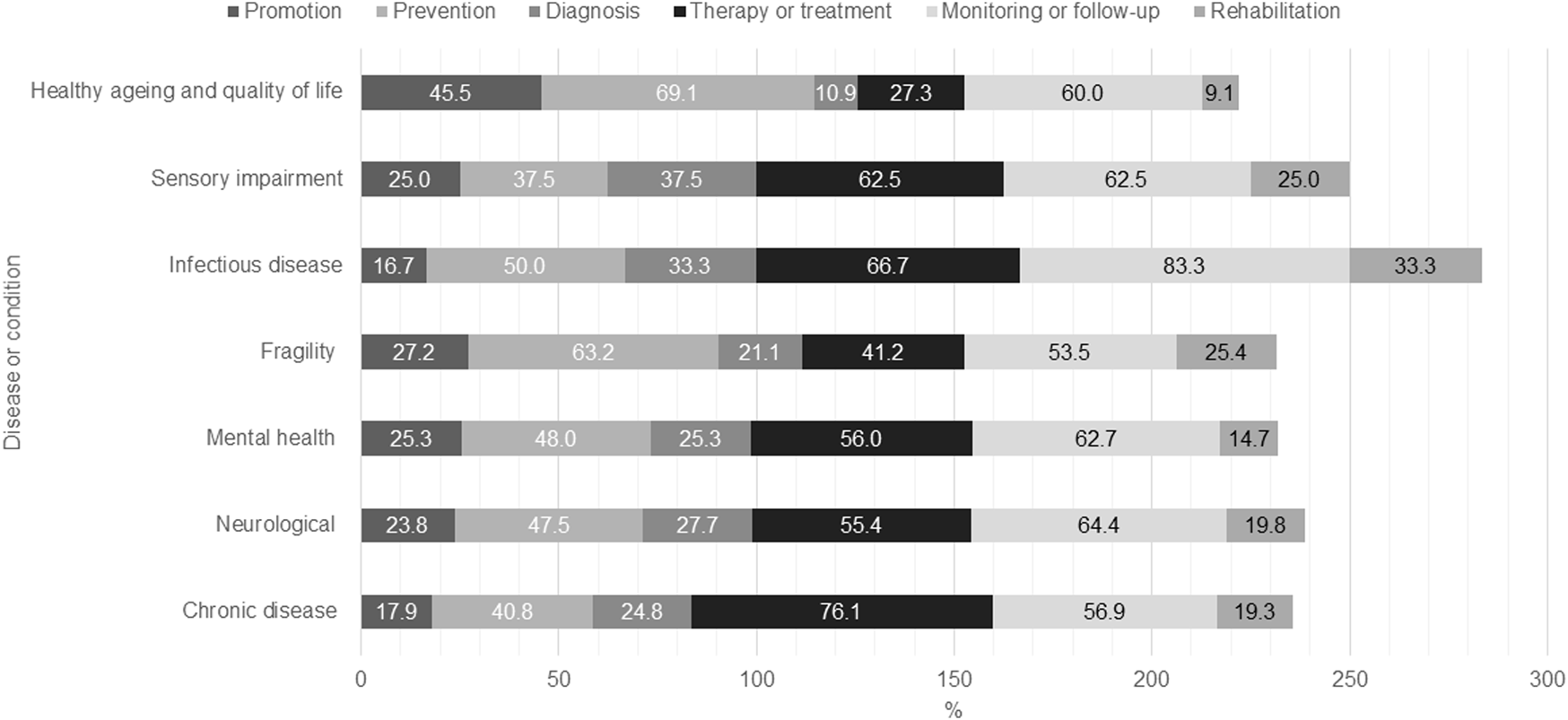
Summary of characteristics of included documents according to Population, Context, Concept (PCC) model (Worldwide, 2022).
When the year of publication and type of device studied were analyzed (Figure 3), it was found that over the years, there is a noticeable increase in the use of telephones, especially in the recent period from 2020 to 2022, suggesting a massive adoption of this technology in the analyzed studies (mostly driven by cell phone and smartphone). The use of desktop or laptop computers remains constant over the years, with significant peaks around 2011 and 2022. Activity monitors and sensors show an increasing trend from 2010 onwards, indicating a rise in the analysis of these technologies, particularly in the years 2015, 2017, and 2021. There is a sustained use of telehealth devices over the years, with a notable increase in 2022, possibly reflecting the response to the COVID-19 pandemic and the need for remote health solutions.
FIGURE 3
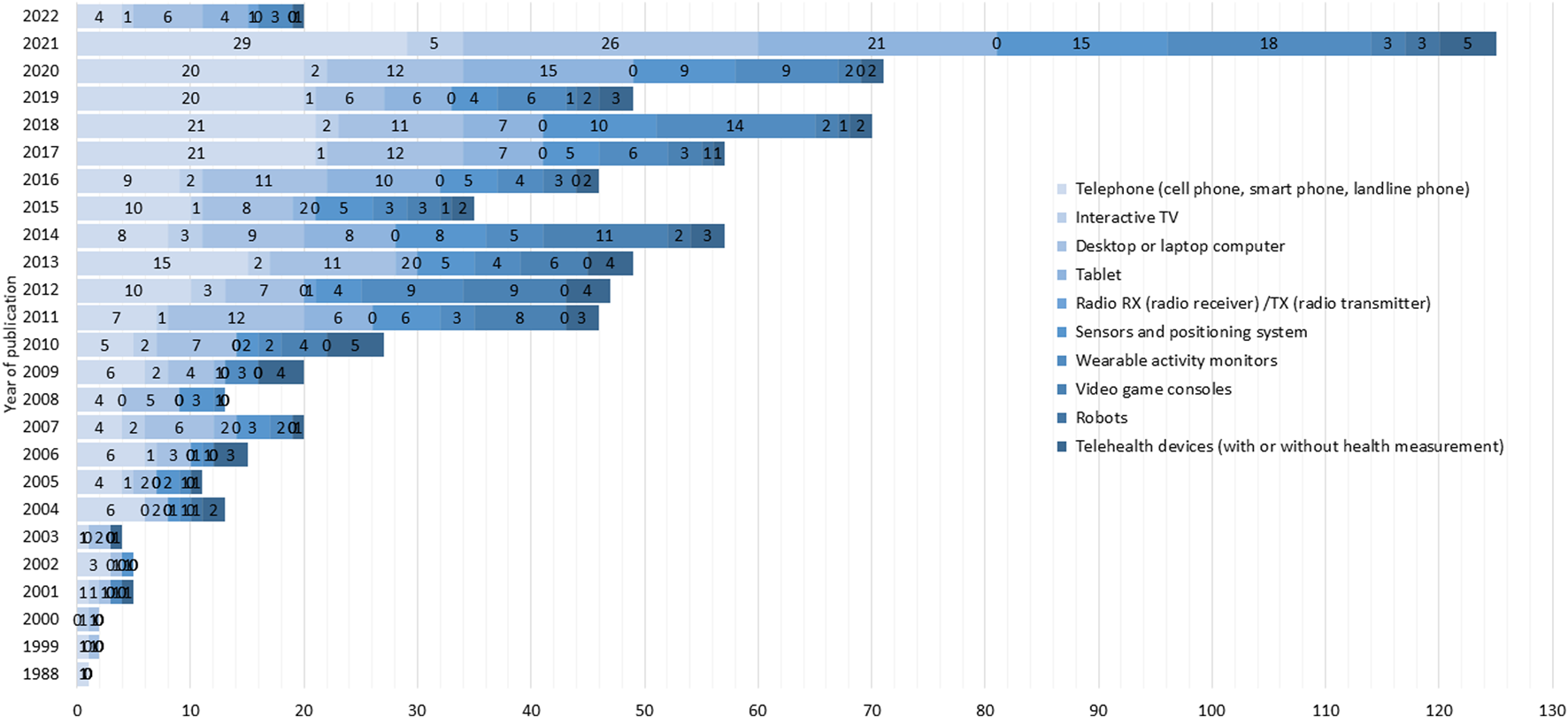
Number of documents by year of publication and type of device studied (Worldwide, 2022).
Figure 4 illustrates the utilization of various technological devices across different health objectives, including promotion, prevention, diagnosis, treatment, monitoring/follow-up, and rehabilitation. Telephones and computers are the most used devices for all health objectives analyzed. However, in the case of promotion, video game consoles (31.4%) and wearables (27.9%) also have a significant presence. For prevention and diagnosis, sensors and positioning systems (32.8% and 28.8%, respectively) and wearables (26.4% and 28.8%, respectively) are also prominent. In the case of therapy or treatment, Tablets rank third (26.0%). For monitoring/follow-up, wearable activity monitors (31.3%) and sensors and positioning systems (25.3%) are also considered important, and finally, for rehabilitation, interactive TV (22.9%) is significant. Overall, the figure highlights the diverse roles of these devices in healthcare, with some being more versatile and widely used across multiple functions.
FIGURE 4
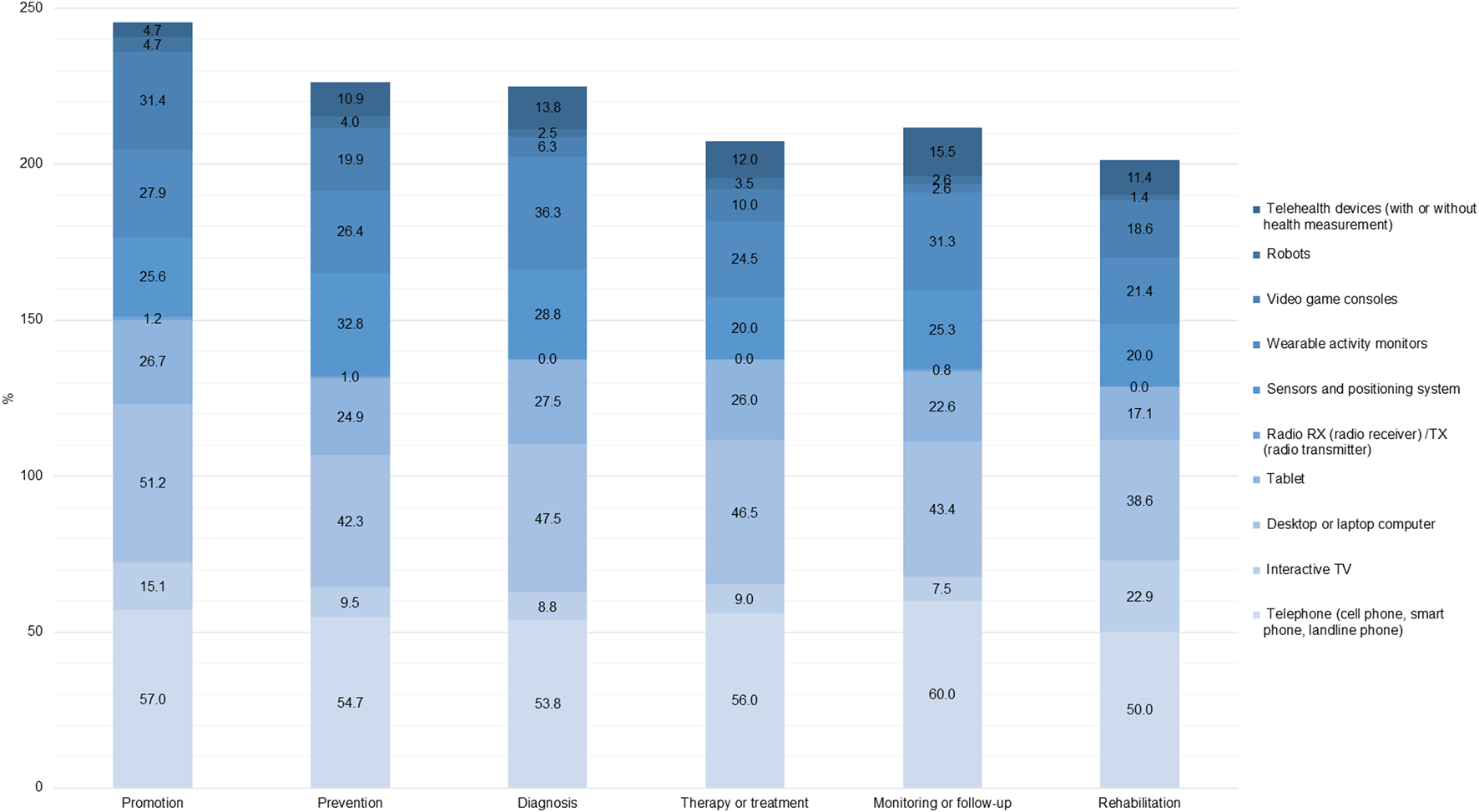
Proportion of documents by health objective and hardware (Worldwide, 2022).
The frequency and distribution of technological devices across multiple diseases, highlights the prominent role of telephones and computers. The data reveals that these devices are extensively used to address chronic diseases (62.8% and 42.2%, respectively), fragility (46.5% and 43.0%) and mental health issues (64.0% and 46.7%). Infectious diseases show same proportion for telephones, computers and Tablets (50.0%, each one). Additionally, telephones show the highest usage for sensory impairments (87.5%). Tablets, wearables and sensors also play a vital role, particularly in neurological conditions (30.7%, 20.8%, and 21.8%) and healthy aging (20.0%, 20.0%, and 25.5%).
Discussion
There has been an exponential increase in the number of publications on digital health and elderly in recent years. Interventions mainly targeted older adults and healthcare professionals, focusing on chronic conditions, frailty, and neurological diseases. Most studies originated from high-income countries, primarily in Europe and Central Asia, with home being the main application context. Technological development was mostly in the testing and validation stages, with fewer in implementation and scalability. The main objectives were monitoring/follow-up, prevention, and treatment. Interventions focused on directed communication and personal health monitoring for individuals, and telemedicine and decision support for healthcare providers. Throughout the period analyzed, telephones and computers were the most used devices, with videoconferencing and text/audio messaging being the most common software. Over the past decade, there has been an increase in the study of wearables, sensors and positioning systems, and a significant rise in telemedicine in 2022, likely due to the COVID-19 pandemic, highlighting the growing adoption of health technologies and positive trends in reported outcomes.
By 2050, 80% of older people will be living in low- and middle-income countries [1]. Despite this, this study found that most technologies designed to assist the elderly are developed and tested in high-income countries. To enhance access to health services for the elderly, it is important to ensure that these technological solutions are available and accessible where most of this population will reside.
An interesting finding were the context in which the studies were conducted, with 76% stating home as their setting, well above healthcare facilities or elderly residences. This aligns closely with older adults’ preferences to stay in their own homes for as long as possible [436, 437]. In this context, digital health, such as receiving remote care, and preparing homes as smart homes, can become a significant ally in supporting elderly to remain in their homes, helping live as independently as possible.
Most documents indicated some level of development, specifically, in testing and validation. These findings suggest a robust pipeline of technological innovations but also raise questions about their maturity and evaluation. The predominance of projects in the testing and validation phase implies many innovations are still in their early stages and may not have demonstrated efficacy in long-term, real-world environments. This focus on early stages suggests a landscape where technologies are frequently conceptualized and prototyped, but fewer are rigorously evaluated and scaled. It is essential to scrutinize whether these technologies are primarily tested with commercial intentions without thorough evaluations of their long-term impact and effectiveness. Moving forward, it is crucial to emphasize comprehensive evaluation and scalability to ensure technological advancements transition from promising prototypes to impactful solutions that withstand real-world application.
One of the key findings is the high number of interventions targeting chronic diseases focusing on treatment. This indicates a strong emphasis on managing long-term conditions through continuous treatment and monitoring, showcasing the potential of technology to support chronic disease management effectively. For neurological diseases, documents emphasize monitoring/follow-up. This suggests a critical role for technology in tracking disease progression and patient status, which is essential for conditions that require constant observation and timely intervention. Mental health conditions showed a similar trend, focusing on monitoring/follow-up. This highlights the importance of sustained surveillance in mental health to provide timely support and intervention, reflecting the need for persistent engagement and assessment in mental healthcare. When examining interventions for fragility conditions, most documents aimed at prevention. This underscores the proactive approach necessary in addressing issues related to frailty, emphasizing the role of technology in preventing falls, improving balance, and maintaining overall health among the elderly. In the same way, healthy aging and quality of life are more related to prevention, highlights the potential of technology to enhance the quality of life and health outcomes for the aging population, aiming to delay the onset of age-related issues and promote wellness. In any case, all the conditions studied show, to a greater or lesser extent, potential for the use of digital technologies for each of the health objectives. This diversity indicates the multifaceted role of technology in managing any condition, from early detection to comprehensive care and education.
Digital health interventions aimed at treatments, including virtual reality, images, videos, and app prescriptions, do not currently have a corresponding category within the existing WHO framework [14]. However, for those digital interventions with a therapeutic purpose, this classification might need to be reviewed to include a category or type of application or system related to this purpose, likely within the “Services and Application Types” section. Including such a category or type dimension would enhance our understanding of digital health applications’ scope and highlight the potential of emerging technologies to address health treatment and management challenges more effectively with innovative and patient-centered solutions. We have submitted this proposal to WHO through the respective form.
It is important to consider the increasing integration of technology in elderly daily lives, recognizing the growing familiarity and comfort of the aging population with technological tools. As today’s older adults have a greater proficiency with technology, their use of digital health interventions is expected to continue rising [438]. This shift presents opportunities to enhance health outcomes through personalized, accessible, and efficient care. However, it also underscores the need for tailored solutions that address the unique needs and preferences of older adults, ensuring that digital health tools are user-friendly and effectively support their health and wellbeing. Healthcare systems will increasingly need to consider these findings to design and implement effective digital health policies for older adults, overcoming various barriers to accessing healthcare services and digital health for this population group.
The evidence in this area is expanding quickly, not only thanks to rapid advances in technology, but also due to the global aging population and a rising interest in meeting the health and quality-of-life needs of elderly. There is very recent literature on this topic [439–441]; however, these studies primarily focus on specific conditions or isolated contexts. In contrast, this review offers a comprehensive approach, while addressing a wide range of technologies, health conditions and diverse contexts for older adults and their caregivers. This broader scope offers a more comprehensive understanding, addressing key gaps in the existing body of research and providing a crucial foundation for designing interventions and strategies that effectively respond to the complex and interconnected needs of these populations.
However, this study has limitations. Since assessing the quality of the evidence is optional in this type of reviews, low-quality studies are not identified. Detailed information on types of telephones and caregivers was also lacking due to incomplete data in the documents. Additionally, the impact of age is an aspect that warrants special consideration, as it helps to explain the growing number of studies in this area. Elderly individuals are increasingly becoming familiar with technology, which reflects an important shift in their interaction with digital health solutions. Few publications exclusively address caregivers of elderly, even though globally, many people provide care for family members with chronic illnesses, disabilities, or aging-related needs. High-income regions, despite having more developed and institutionalized care systems, also rely on family caregivers [442, 443]. A study found that over 50% of elderly (OECD countries) preferred family care over formal help, influenced by socioeconomic level and cultural values [444]. In Latin America and the Caribbean, the caregiving burden is especially significant, with family members, particularly women, shouldering most responsibilities, often involving extensive unpaid work. This demanding role often results in high levels of stress, burnout, and health issues among caregivers, underscoring the urgent need for enhanced support and resources tailored to family caregivers in these regions [445].
Finally, the high proportion of documents presenting positive results (86.9%), is consistent with the literature trend where positive results are much more represented than negative ones, indicating a potential publication bias [446]. This, among other issues related to underreporting negative results, introduces bias in analyses and misinforms researchers and, consequently, decision-makers.
Conclusion
Increasing integration of technology in older adults’ lives, along with their increasing proficiency, is driving a significant rise in digital health interventions. Despite this growth, further research in middle- and low-income countries, for caregivers and evaluating effectiveness and feasibility of these technological interventions is needed. The future of digital health for elderly population, caregivers and healthcare professionals presents challenges that must be addressed to realize its full potential. One major issue is accessibility, as these technologies evolve it will be essential ensuring that they are user-friendly and inclusive for all older adults, regardless of their technical skills. Data privacy and security also become critical concerns as more personal health information is shared through digital platforms, demanding robust protections to build and maintain trust among users. Additionally, healthcare providers will face the challenge of integrating digital health tools effectively within traditional care settings, which may require new training and adaptation to evolving workflows. Finally, supporting caregivers and family members in adopting these technologies could be complex, as they often have diverse needs and limited time. Addressing these challenges will be key to harnessing the power of digital health to improve care and quality of life for aging populations.
Statements
Author contributions
Conceptualization: AJ, MM, XM, and MH-A; Search: AJ, MM, MH-A, XM, and MT-A; Selection: AJ, AO, XM, MH-A, IM, CC-L, CA, PR, OU, TA, FS, and SE; Extraction: AO, CA, CC-L, MH-A, PR, OU, FS, and XM. Manuscript: AO, AJ, MM, MH-A, IM, CC-L, CA, TA, FS, SE, PR, MT-A, OU, and XM. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The financial support for this manuscript was provided by the Dirección de Investigación y Doctorados at Universidad del Desarrollo.
Acknowledgments
We would like to thank Jenifer Putz, librarian at the Faculty of Medicine, Clínica Alemana Universidad del Desarrollo, for her assistance in retrieving scientific articles throughout the review process. ChatGPT 4o was used as an English check in some paragraphs and to summarize others.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Correction note
A correction has been made to this article. Details can be found at: 10.3389/phrs.2026.1609579.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/phrs.2024.1607756/full#supplementary-material
Footnotes
1.^The strategy created for PubMed was modified to suit the requirements of the other databases.
References
1.
World Health Organization. Ageing and Health (2022). Available from: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (Accessed November 14, 2022).
2.
RiffinCVan NessPHIannoneLFriedT. Patient and Caregiver Perspectives on Managing Multiple Health Conditions HHS Public Access. J Am Geriatr Soc (2018) 66(10):1992–7. 10.1111/jgs.1550
3.
WeissEFMalikRSantosTCeideMCohenJVergheseJet alTelehealth for the Cognitively Impaired Older Adult and Their Caregivers: Lessons From a Coordinated Approach. Neurodegener Dis Manag (2021) 11(1):83–9. 10.2217/nmt-2020-0041
4.
PietteJDStriplinDMarinecNChenJTrivediRBAronDCet alA Mobile Health Intervention Supporting Heart Failure Patients and Their Informal Caregivers: A Randomized Comparative Effectiveness Trial. J Med Internet Res (2015) 17(6):e142. 10.2196/jmir.4550
5.
Organización Mundial de la Salud. WHO Guideline: Recommendations on Digital Interventions for Health System Strengthening (2019). Available from: https://www.who.int/publications/i/item/9789241550505 (Accessed November 14, 2022).
6.
RivoirAMoralesMJCasamayouA. Usos y Percepciones de las Tecnologías Digitales en Personas Mayores. Limitaciones y Beneficios para su Calidad de Vida. Revista Austral de Ciencias Sociales (2019) 36:295–313. 10.4206/rev.austral.cienc.soc.2019.n36-15
7.
EvansDBHsuJBoermaT. Universal Health Coverage and Universal Access. Bull World Health Organ (2013) 91(8):546–A. 10.2471/BLT.13.125450
8.
World Health Organization (WHO). The Seventy-First World Health Assembly. Digital health (2018) 4.
9.
EvangelistaLSteinhublSRTopolEJ. Digital Health Care for Older Adults. The Lancet (2019) 393(10180):1493. 10.1016/S0140-6736(19)30800-1
10.
PetersMGodfreyCMcInerneyPMunnZTriccoAKhalilH. In: AromatarisEMunnZ, editors. Chapter 11: Scoping Reviews (2020 Version). JBI Manual for Evidence Synthesis (2020). Available from: https://synthesismanual.jbi.global (Accessed June 12, 2024).
11.
TriccoACLillieEZarinWO’BrienKKColquhounHLevacDet alPRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med (2018) 169:467–73. 10.7326/M18-0850
12.
Organización Mundial de la Salud (OMS). Envejecimiento y Salud. World Health Organization (2024). Available from: https://www.who.int/es/news-room/fact-sheets/detail/ageing-and-health (Accessed February 2, 2020).
13.
PetersMDJGodfreyCMKhalilHMcInerneyPParkerDSoaresCB. Guidance for Conducting Systematic Scoping Reviews. Int J Evid Based Healthc (2015) 13:141–6. 10.1097/XEB.0000000000000050
14.
World Health Organization. Classification of Digital Interventions, Services and Applications in Health. In: A Shared Language to Describe the Uses of Digital Technology for Health. 2nd ed. (2023). Available from: https://iris.who.int/bitstream/handle/10665/373581/9789240081949-eng.pdf?sequence=1 (Accessed February 29, 2024).
15.
BhattacharyaSKumarVNarayanNS. Technology Readiness Level: An Assessment of the Usefulness of This Scale for Translational Research. Productivity (2022) 62(2):106–18. 10.32381/PROD.2021.62.02.2
16.
BurdeseETestaMRaucciPFerreriCGiovanniniGLombardoEet alUsefulness of a Telemedicine Program in Refractory Older Congestive Heart Failure Patients. Diseases (2018) 6(1):10. 10.3390/diseases6010010
17.
TomitaMRMannWCStantonKTomitaADSundarVStantonM. Use of Currently Available Smart Home Technology by Frail Elders Process and Outcomes. Top Geriatr Rehabil (2007) 23(1):24–34. 10.1097/00013614-200701000-00005
18.
Blanson HenkemansOARogersWAFiskADNeerincxMALindenbergJ,Van Der Mast CAPG. Usability of an Adaptive Computer Assistant That Improves Self-Care and Health Literacy of Older Adults. Methods Inf Med (2008) 47:82–8. 10.3414/me9105
19.
HarerimanaBForchukCO’ReganT. The Use of Technology for Mental Healthcare Delivery Among Older Adults With Depressive Symptoms: A Systematic Literature Review. Int J Ment Health Nurs (2019) 28:657–70. 10.1111/inm.12571
20.
KimJSonJKoNYoonB. Unsupervised Virtual Reality-Based Exercise Program Improves Hip Muscle Strength and Balance Control in Older Adults: A Pilot Study. Arch Phys Med Rehabil (2013) 94(5):937–43. 10.1016/j.apmr.2012.12.010
21.
BarrettD. The Role of Telemonitoring in Caring for Older People With Long-Term Conditions. Nurs Old People (2012) 24(7):21–5. 10.7748/nop2012.09.24.7.21.c9257
22.
Hee CHoGHwanGboGSoo SHinH. The Effects of Virtual Reality-Based Balance Training on Balance of the Elderly. Phys Ther Sci (2014) 26(4):615–7. 10.1589/jpts.26.615
23.
ParkECKimSGLeeCW. The Effects of Virtual Reality Game Exercise on Balance and Gait of the Elderly. Phys Ther Sci (2015) 27(4):1157–9. 10.1589/jpts.27.1157
24.
LarsenLHSchouLLundHHLangbergH, The Physical Effect of Exergames in Healthy Elderly - A Systematic Review. Games Health J (2013). 2, 205–12. 10.1089/g4h.2013.0036
25.
JungHLeeJE. The Impact of Community-Based eHealth Self-Management Intervention Among Elderly Living Alone With Hypertension. J Telemed Telecare (2017) 23(1):167–73. 10.1177/1357633X15621467
26.
NakamuraKTakanoTAkaoC. The Effectiveness of Videophones in Home Healthcare for the Elderly. Care (1999) 37:117–25. 10.1097/00005650-199902000-00002
27.
BainbridgeEBevansSKeeleyBOrielK. The Effects of the Nintendo Wii Fit on Community-Dwelling Older Adults With Perceived Balance Deficits: A Pilot Study. Phys Occup Ther Geriatr (2011) 29(2):126–35. 10.3109/02703181.2011.569053
28.
RendonAALohmanEBThorpeDJohnsonEGMedinaEBradleyB. The Effect of Virtual Reality Gaming on Dynamic Balance in Older Adults. Age Ageing (2012) 41(4):549–52. 10.1093/ageing/afs053
29.
TeixeiraEFonsecaHDiniz-SousaFVerasLBoppreGOliveiraJet alWearable Devices for Physical Activity and Healthcare Monitoring in Elderly People: A Critical Review. Geriatrics (Basel) (2021) 6:38, 10.3390/geriatrics6020038
30.
BarnettTEChumblerNRBruce VogelWBeythRJQinHKobbR. The Effectiveness of a Care Coordination Home Telehealth Program for Veterans With Diabetes Mellitus: A 2-Year Follow-Up. Am J Manag Care (2006) 12(8):467–74.
31.
FrancoJRJacobsKInzerilloCKluzikJ. The Effect of the Nintendo Wii Fit and Exercise in Improving Balance and Quality of Life in Community Dwelling Elders. Tech Health Care (2012) 20:95–115. 10.3233/THC-2011-0661
32.
WilliamsBDohertyNLBenderAMattoxHTibbsJR. The Effect of Nintendo Wii on Balance: A Pilot Study Supporting the Use of the Wii in Occupational Therapy for the Well Elderly. Occup Ther Health Care (2011) 25(2–3):131–9. 10.3109/07380577.2011.560627
33.
KimHJhooJHJangJW. The Effect of Telemedicine on Cognitive Decline in Patients With Dementia. J Telemed Telecare (2017) 23(1):149–54. 10.1177/1357633X15615049
34.
GuderianBBorresonASlettenLECableKSteckerPProbstMAet alThe Cardiovascular and Metabolic Responses to Wii Fit Video Game Playing in Middle-Aged and Older Adults. Sports Med Phys Fitness (2010) 50:436–42.
35.
DanielK. Wii-Hab for Pre-frail Older Adults. Rehabil Nurs (2012) 37(4):195–201. 10.1002/rnj.25
36.
ToulotteCTourselCOlivierN. Wii Fit® Training vs. Adapted Physical Activities: Which One Is the Most Appropriate to Improve the Balance of Independent Senior Subjects? A Randomized Controlled Study. Clin Rehabil (2012) 26(9):827–35. 10.1177/0269215511434996
37.
WasilewskiMBStinsonJNCameronJI. Web-Based Health Interventions for Family Caregivers of Elderly Individuals: A Scoping Review. Int J Med Inform (2017) 103:109–38. 10.1016/j.ijmedinf.2017.04.009
38.
HsiehWMChenCCWangSCTanSYHwangYSChenSCet alVirtual Reality System Based on Kinect for the Elderly in Fall Prevention. Tech Health Care (2014) 22(1):27–36. 10.3233/THC-130769
39.
MolinaKIRicciNADe MoraesSAPerraciniMR. Virtual Reality Using Games for Improving Physical Functioning in Older Adults: A Systematic Review. J NeuroEngineering Rehabil (2014) 11:156. 10.1186/1743-0003-11-156
40.
PietrzakECoteaCPullmanS. Using Commercial Video Games for Falls Prevention in Older Adults: The Way for the Future?J Geriatr Phys Ther (2014). 37:166–77.
41.
KruseCFohnJWilsonNPatlanENZippSMileskiM. Utilization Barriers and Medical Outcomes Commensurate With the Use of Telehealth Among Older Adults: Systematic Review. JMIR Med Inform (2020) 8(8):e20359. 10.2196/20359
42.
ChatterjeeSByunJPottathilAMooreMNDuttaKQiHet alPersuasive Sensing: A Novel in-Home Monitoring Technology to Assist Elderly Adult Diabetic Patients. Springer (2012). p. 31–42.
43.
MaustDTMavandadiSBensonAStreimJEDiFilippoSSneddenTet alTelephone-Based Care Management for Older Adults Initiated on Psychotropic Medication. Int J Geriatr Psychiatry (2013) 28(4):410–6. 10.1002/gps.3839
44.
BrignellMWoottonRGrayL. The Application of Telemedicine to Geriatric Medicine. Age and Ageing (2007) 36:369–74. 10.1093/ageing/afm045
45.
SallesNBaudonMPCaubetCDallayFChaleuilMMagneSet alTelemedicine Consultations for the Elderly With Chronic Wounds, Especially Pressure Sores. Eur Res Telemed (2013) 2(3–4):93–100. 10.1016/j.eurtel.2013.06.001
46.
ForduceyPGGlueckaufRLBergquistTFMaheuMMYutsisM. Telehealth for Persons With Severe Functional Disabilities and Their Caregivers: Facilitating Self-Care Management in the Home Setting. Psychol Serv (2012) 9(2):144–62. 10.1037/a0028112
47.
HamiltonTJohnsonLQuinnBTCoppolaJSachsDMigliaccioJet alTelehealth Intervention Programs for Seniors: An Observational Study of a Community-Embedded Health Monitoring Initiative. Telemed e-Health (2020) 26(4):438–45. 10.1089/tmj.2018.0248
48.
CzajaSJRubertMP. Telecommunications Technology as an Aid to Family Caregivers of Persons With Dementia. Psychosom Med (2002) 64:469–76. 10.1097/00006842-200205000-00011
49.
WilliamsKNPerkhounkovaYShawCAHeinMVidoniEDColemanCK. Supporting Family Caregivers With Technology for Dementia Home Care: A Randomized Controlled Trial. Innov Aging (2019) 3(3):igz037. 10.1093/geroni/igz037
50.
WebsterDCelikO. Systematic Review of Kinect Applications in Elderly Care and Stroke Rehabilitation. J NeuroEng Rehabil (2014) 11:108. 10.1186/1743-0003-11-108
51.
KimBYBLeeJ. Smart Devices for Older Adults Managing Chronic Disease: A Scoping Review, JMIR Mhealth Uhealth (2017) 5:e69, 10.2196/mhealth.7141
52.
HarbigPBaratIDamsgaardEM. Suitability of an Electronic Reminder Device for Measuring Drug Adherence in Elderly Patients With Complex Medication. J Telemed Telecare (2012) 18(6):352–6. 10.1258/jtt.2012.120120
53.
De LeoDBuono DelloMDwyerJ. Suicide Among the Elderly: The Long-Term Impact of a Telephone Support and Assessment Intervention in Northern Italy. Br J Psychiatry (2002) 181:226–9. 10.1192/bjp.181.3.226
54.
KeoghJWLPowerNWoollerLLucasPWhatmanC. Physical and Psychosocial Function in Residential Aged-Care Elders: Effect of Nintendo Wii Sports Games. J Aging Phys Act (2014) 22(2):235–44. 10.1123/japa.2012-0272
55.
RegterschotGRHFolkersmaMZhangWBaldusHStevensMZijlstraW. Sensitivity of Sensor-Based Sit-To-Stand Peak Power to the Effects of Training Leg Strength, Leg Power and Balance in Older Adults. Gait Posture (2014) 39(1):303–7. 10.1016/j.gaitpost.2013.07.122
56.
Anderson-HanleyCSnyderALNimonJPArcieroPJ. Social Facilitation in Virtual Reality-Enhanced Exercise: Competitiveness Moderates Exercise Effort of Older Adults. Clin Interv Aging (2011) 6(1):275–80. 10.2147/CIA.S25337
57.
KuwaharaNYasudaKTetsutaniNMorimotoK. Remote Assistance for People With Dementia at Home Using Reminiscence Systems and a Schedule Prompter. Int J Comput Healthc (2010) 1:126. 10.1504/ijcih.2010.037458
58.
VincentCReinharzDDeaudelinIGarceauMTalbotLR. Public Telesurveillance Service for Frail Elderly Living at Home, Outcomes and Cost Evolution: A Quasi Experimental Design With Two Follow-Ups. Health Qual Life Outcomes (2006) 4:41. 10.1186/1477-7525-4-41
59.
CampbellAJRobertsonMCLa GrowSJKerseNMSandersonGFJacobsRJet alRandomised Controlled Trial of Prevention of Falls in People Aged > or =75 With Severe Visual Impairment: The VIP Trial. Br Med J (2005) 331(7520):817–20. 10.1136/bmj.38601.447731.55
60.
WollersheimDMerkesMShieldsN. Physical and Psychosocial Effects of Wii Video Game Use Among Older Women. Aust J Emerging Tech Soc (2010) 8(2):85–98. Available from: https://www.researchgate.net/publication/232613430 (Accessed June 1, 2023).
61.
GellisZDKenaleyBMcGintyJBardelliEDavittJTen HaveT. Outcomes of a Telehealth Intervention for Homebound Older Adults With Heart or Chronic Respiratory Failure: A Randomized Controlled Trial. Gerontologist (2012) 52(4):541–52. 10.1093/geront/gnr134
62.
TetleyJHansonEClarkeA. Older People, Telematics and Care. In: WarnesTWarrenLNolanM editors. Care Services for Later Life: Transformations and Critiques. London, UK: Jessica Kinglsey (2001). p. 243–58.
63.
SunCSunLXiSZhangHWangHFengYet alMobile Phone–Based Telemedicine Practice in Older Chinese Patients With Type 2 Diabetes Mellitus: Randomized Controlled Trial. JMIR Mhealth Uhealth (2019) 7(1):e10664. 10.2196/10664
64.
JoeJDemirisG. Older Adults and Mobile Phones for Health: A Review. J Biomed Inform (2013) 46:947–54. 10.1016/j.jbi.2013.06.008
65.
SunRSosnoffJJ. Novel Sensing Technology in Fall Risk Assessment in Older Adults: A Systematic Review. BMC Geriatr (2018) 18:14. 10.1186/s12877-018-0706-6
66.
QuinnCCKhokharBWeedKBarrEGruber-BaldiniAL. Older Adult Self-Efficacy Study of Mobile Phone Diabetes Management. Diabetes Technol Ther (2015) 17(7):455–61. 10.1089/dia.2014.0341
67.
ForsetlundLBjørndalARashidianAJamtvedtGO’BrienMAWolfFet alContinuing Education Meetings and Workshops: Effects on Professional Practice and Health Care Outcomes. Cochrane Database Syst Rev (2009) 2009:CD003030. 10.1002/14651858.CD003030.pub2
68.
ChenPYWeiSHHsiehWLCheenJRChenLKKaoCL. Lower Limb Power Rehabilitation (LLPR) Using Interactive Video Game for Improvement of Balance Function in Older People. Arch Gerontol Geriatr (2012) 55(3):677–82. 10.1016/j.archger.2012.05.012
69.
KamimuraTIshiwataRInoueT. Medication Reminder Device for the Elderly Patients With Mild Cognitive Impairment. Am J Alzheimers Dis Other Demen (2012) 27(4):238–42. 10.1177/1533317512450066
70.
Center for Technology and Aging. mHealth Technologies: Applications to Benefit Older Adults. 2011.
71.
TamuraTYonemitsuSItohAOikawaDKawakamiAHigashiYet alIs an Entertainment Robot Useful in the Care of Elderly People With Severe Dementia?J Gerontol A Biol Sci Med Sci (2004) 59:83–5. 10.1093/gerona/59.1.m83
72.
DearBFZouJTitovNLorianCJohnstonLSpenceJet alInternet-Delivered Cognitive Behavioural Therapy for Depression: A Feasibility Open Trial for Older Adults. Aust New Zealand J Psychiatry (2013) 47(2):169–76. 10.1177/0004867412466154
73.
WuYHFaucounauVDe RotrouJRiguetMRigaudAS. Intervention Psychosociale Auprès d’Aidants Familiaux de Patients Atteints de la Maladie d’Alzheimer et Technologies de l’Information et de la Communication: Une Revue de la Littérature. Psychol NeuroPsychiatrie du Vieillissement (2009) 7(3):185–92.
74.
ChopikWJ. The Benefits of Social Technology Use Among Older Adults Are Mediated by Reduced Loneliness. Cyberpsychol Behav Soc Netw (2016) 19(9):551–6. 10.1089/cyber.2016.0151
75.
JorgensenMGLaessoeUHendriksenCNielsenOBFAagaardP. Efficacy of Nintendo Wii Training on Mechanical Leg Muscle Function and Postural Balance in Community-Dwelling Older Adults: A Randomized Controlled Trial. Journals Gerontol - Ser A Biol Sci Med Sci (2013) 68(7):845–52. 10.1093/gerona/gls222
76.
SiegelCDornerTE. Information Technologies for Active and Assisted Living—Influences to the Quality of Life of an Ageing Society. Int J Med Inform (2017) 100:32–45. 10.1016/j.ijmedinf.2017.01.012
77.
KayeJAMaxwellSAMattekNHayesTLDodgeHPavelMet alIntelligent Systems for Assessing Aging Changes: Home-Based, Unobtrusive, and Continuous Assessment of Aging. J Gerontol B Psychol Sci Soc Sci (2011) 66(Suppl. 1):i180–i190. 10.1093/geronb/gbq095
78.
CottenSRAndersonWAMcCulloughBM. Impact of Internet Use on Loneliness and Contact With Others Among Older Adults: Cross-Sectional Analysis. J Med Internet Res (2013) 15(2):e39. 10.2196/jmir.2306
79.
BarnasonSZimmermanLSchulzPTuC. Influence of an Early Recovery Telehealth Intervention on Physical Activity and Functioning After Coronary Artery Bypass Surgery Among Older Adults With High Disease Burden. Heart Lung J Acute Crit Care (2009) 38(6):459–68. 10.1016/j.hrtlng.2009.01.010
80.
SatoKKurokiKSaikiSNagatomiR. Improving Walking, Muscle Strength, and Balance in the Elderly with an Exergame Using Kinect: A Randomized Controlled Trial. Games Health J (2015) 4(3):161–7. 10.1089/g4h.2014.0057
81.
BarnasonSZimmermanLNieveenJSchulzPMillerCHertzogMet alInfluence of a Symptom Management Telehealth Intervention on Older Adults’ Early Recovery Outcomes After Coronary Artery Bypass Surgery. Heart Lung J Acute Crit Care (2009) 38(5):364–76. 10.1016/j.hrtlng.2009.01.005
82.
TriefPMTeresiJAEimickeJPSheaSWeinstockRS. Improvement in Diabetes Self-Efficacy and Glycaemic Control Using Telemedicine in a Sample of Older, Ethnically Diverse Individuals Who Have Diabetes: The IDEATel Project. Age Ageing (2009) 38(2):219–25. 10.1093/ageing/afn299
83.
BernocchiPVitaccaMLa RovereMTVolterraniMGalliTBarattiDet alHome-Based Telerehabilitation in Older Patients With Chronic Obstructive Pulmonary Disease and Heart Failure: A Randomised Controlled Trial. Age Ageing (2018) 47(1):82–8. 10.1093/ageing/afx146
84.
PecinaJLHansonGJVan HoutenHTakahashiPY. Impact of Telemonitoring on Older Adults Health-Related Quality of Life: The Tele-ERA Study. Qual Life Res (2013) 22(9):2315–21. 10.1007/s11136-013-0361-5
85.
MadiganESchmotzerBJStrukCJDiCarloCMKikanoGPiñaILet alHome Health Care With Telemonitoring Improves Health Status for Older Adults With Heart Failure. Home Health Care Serv Q (2013) 32(1):57–74. 10.1080/01621424.2012.755144
86.
LudwigWWolfKHDuwenkampCGusewNHellrungNMarschollekMet alHealth-Enabling Technologies for the Elderly - An Overview of Services Based on a Literature Review. Comput Methods Programs Biomed (2012) 106(2):70–8. 10.1016/j.cmpb.2011.11.001
87.
CaljouwSRVuijkPJLamothC. Exergaming: Interactive Balance Training in Healthy Community-Dwelling Older Adults (2011). Available from: https://www.researchgate.net/publication/51994865 (Accessed August 16, 2023).
88.
SallesNLafargueACressotVGlenissonLBarateauMThielEet alGlobal Geriatric Evaluation Is Feasible during Interactive Telemedicine in Nursing Homes. Eur Res Telemed (2017) 6(2):59–65. 10.1016/j.eurtel.2017.06.002
89.
GrindrodKALiMGatesA. Evaluating User Perceptions of Mobile Medication Management Applications With Older Adults: A Usability Study. JMIR Mhealth Uhealth (2014) 2(1):e11. 10.2196/mhealth.3048
90.
Van DiestMLamothCJStegengaJVerkerkeGJPostemaK. Exergaming for Balance Training of Elderly: State of the Art and Future Developments. J NeuroEngineering Rehabil (2013) 10:101. 10.1186/1743-0003-10-101
91.
RosenbergDDeppCAVahiaIVReichstadtJPalmerBWKerrJet alExergames for Subsyndromal Depression in Older Adults: A Pilot Study of a Novel Intervention. Am J Geriatr Psychiatry (2010) 18(3):221–6. 10.1097/JGP.0b013e3181c534b5
92.
BroxELuqueLFEvertsenGJHernandezJEG. Exergames for Elderly: Social Exergames to Persuade Seniors to Increase Physical Activity. In: 2011 5th International Conference on Pervasive Computing Technologies for Healthcare (PervasiveHealth) and Workshops, Dublin, Ireland, May 23–26, 2011 (IEEE) (2011). p. 546–9.
93.
UptonDUptonPJonesTJutllaKBrookerD. Evaluation of the Impact of Touch Screen Technology on People With Dementia and Their Caregivers Within Care Home Settings. 2011.
94.
MasedaAMillán-CalentiJCLorenzo-LópezLNúñez-NaveiraL. Efficacy of a Computerized Cognitive Training Application for Older Adults With and Without Memory Impairments. Aging Clin Exp Res (2013) 25(4):411–9. 10.1007/s40520-013-0070-5
95.
RodriguesEValderramasSRossetinLGomesAR. Effects of Video Game Training on the Musculoskeletal Function of Older Adults: A Systematic Review and Meta-Analysis. Top Geriatr Rehabil (2014) 30(4):238–45. 10.1097/tgr.0000000000000040
96.
HagedornDKHolmE. Effects of Traditional Physical Training and Visual Computer Feedback Training in Frail Elderly Patients. A Randomized Intervention Study. Eur J Phys Rehabil Med (2010) 46:159–68.
97.
GeraedtsHZijlstraABulstraSKStevensMZijlstraW. Effects of Remote Feedback in Home-Based Physical Activity Interventions for Older Adults: A Systematic Review. Patient Educ Couns (2013) 91:14–24. 10.1016/j.pec.2012.10.018
98.
MaillotPPerrotAHartleyA. Effects of Interactive Physical-Activity Video-Game Training on Physical and Cognitive Function in Older Adults. Psychol Aging (2012) 27(3):589–600. 10.1037/a0026268
99.
LaiCHPengCWChenYLHuangCPHsiaoYLChenSC. Effects of Interactive Video-Game Based System Exercise on the Balance of the Elderly. Gait Posture (2013) 37(4):511–5. 10.1016/j.gaitpost.2012.09.003
100.
MuellmannSForbergerSMöllersTBröringEZeebHPischkeCR. Effectiveness of eHealth Interventions for the Promotion of Physical Activity in Older Adults: A Systematic Review. Prev Med (2018) 108:93–110. 10.1016/j.ypmed.2017.12.026
101.
ChangiziMKavehMH. Effectiveness of the mHealth Technology in Improvement of Healthy Behaviors in an Elderly Population—A Systematic Review. Mhealth (2017) 3:51. 10.21037/mhealth.2017.08.06
102.
StudenskiSPereraSHileEKellerVSpadola-BogardJGarciaJ. Interactive Video Dance Games for Healthy Older Adults. Nutr Health Aging (2010) 14(10):850–2. 10.1007/s12603-010-0119-5
103.
LeeSShinS. Effectiveness of Virtual Reality Using Video Gaming Technology in Elderly Adults With Diabetes Mellitus. Diabetes Technol Ther (2013) 15(6):489–96. 10.1089/dia.2013.0050
104.
MulasIPutzuVAsoniGVialeDMameliIPauM. Clinical Assessment of Gait and Functional Mobility in Italian Healthy and Cognitively Impaired Older Persons Using Wearable Inertial Sensors. Aging Clin Exp Res (2021) 33(7):1853–64. 10.1007/s40520-020-01715-9
105.
KueiderAMParisiJMGrossALRebokGW. Computerized Cognitive Training With Older Adults: A Systematic Review. PLoS One (2012) 7(7):e40588. 10.1371/journal.pone.0040588
106.
BotsisTHartvigsenG. Current Status and Future Perspectives in Telecare for Elderly People Suffering from Chronic Diseases. J Telemed Telecare (2008) 14(4):195–203. 10.1258/jtt.2008.070905
107.
TsaiHHTsaiYF. Changes in Depressive Symptoms, Social Support, and Loneliness Over 1 Year After a Minimum 3-Month Videoconference Program for Older Nursing Home Residents. J Med Internet Res (2011) 13(4):e93. 10.2196/jmir.1678
108.
EjupiABrodieMGschwindYJSchoeneDLordSDelbaereK. Choice Stepping Reaction Time Test Using Exergame Technology for Fall Risk Assessment in Older People. Annu Int Conf IEEE Eng Med Biol Soc (2014) 2014:6957–60. 10.1109/EMBC.2014.6945228
109.
LengFYYeoDGeorgeSBarrC. Comparison of iPad Applications With Traditional Activities Using Person-Centred Care Approach: Impact on Well-Being for Persons With Dementia. Dementia (2014) 13(2):265–73. 10.1177/1471301213494514
110.
BateniH. Changes in Balance in Older Adults Based on Use of Physical Therapy vs the Wii Fit Gaming System: A Preliminary Study. Physiotherapy (United Kingdom) (2012) 98(3):211–6. 10.1016/j.physio.2011.02.004
111.
BanburyAChamberlainDNancarrowSDartJGrayLParkinsonL. Can Videoconferencing Affect Older People’s Engagement and Perception of Their Social Support in Long-Term Conditions Management: A Social Network Analysis From the Telehealth Literacy Project. Health Soc Care Community (2017) 25(3):938–50. 10.1111/hsc.12382
112.
JenkinsCAmellaEMuellerMMooreMHathawayD. An Internet-Assisted Weight Loss Intervention for Older Overweight and Obese Rural Women A Feasibility Study. Comput Inform Nurs (2016) 34:513–9. 10.1097/CIN.0000000000000275
113.
BradleyNPoppenW. Assistive Technology, Computers and Internet May Decrease Sense of Isolation for Homebound Elderly and Disabled Persons. Technol Disabil (2003) 15:19–25. 10.3233/tad-2003-15104
114.
TedescoSBartonJO’FlynnB. A Review of Activity Trackers for Senior Citizens: Research Perspectives, Commercial Landscape and the Role of the Insurance Industry. Sensors (Switzerland); 2017.17, 1277, 10.3390/s17061277
115.
KirkAMacMillanFRiceMCarmichaelA. An Exploratory Study Examining the Appropriateness and Potential Benefit of the Nintendo Wii as a Physical Activity Tool in Adults Aged ≥ 55 Years. Interact Comput (2013) 25(1):102–14. 10.1093/iwc/iws004
116.
LamothCCaljouwSRPostemaK. Active Video Gaming to Improve Balance in the Elderly. Stud Health Technol Inform (2011) 167:159–64. Available from: https://www.researchgate.net/publication/51231122 (Accessed April 11, 2023).
117.
CheekPNikpourLNowunHD. Aging Well with Smart Technology. Nurs Admin Q (2005) 29:329–38. 10.1097/00006216-200510000-00007
118.
PiauACampoERumeauPVellasBNourhasheimF. Aging Society and Gerontechnology: A Solution for an Independent Living?Nutr Health Aging (2013). 10.1007/s12603-013-0356-5
119.
VaportzisEMartinMGowAJ. A Tablet for Healthy Ageing: The Effect of a Tablet Computer Training Intervention on Cognitive Abilities in Older Adults. Am J Geriatr Psychiatry (2017) 25(8):841–51. 10.1016/j.jagp.2016.11.015
120.
Infante‐RivardCKriegerMPetitclercMBaumgartenM. A Telephone Support Service to Reduce Medical Care Use Among the Elderly. J Am Geriatr Soc (1988) 36(4):306–11. 10.1111/j.1532-5415.1988.tb02356.x
121.
LeeJHKimHJhooHLeeUKimWLeeYet alA Telemedicine System as a Care Modality for Dementia Patients in Korea. Alzheimer Dis Assoc Disord (2000) 14:94–101. 10.1097/00002093-200004000-00007
122.
BarlowJSinghDBayerSCurryR. A Systematic Review of the Benefits of Home Telecare for Frail Elderly People and Those With Long-Term Conditions. J Telemed Telecare (2007) 13:172–9. 10.1258/135763307780908058
123.
ChauJPLeeDTYuDSChowAYuWCChairSet alA Feasibility Study to Investigate the Acceptability and Potential Effectiveness of a Telecare Service for Older People With Chronic Obstructive Pulmonary Disease. Int J Med Inform (2012) 81(10):674–82. 10.1016/j.ijmedinf.2012.06.003
124.
JerantAFAzariRMartinezCNesbittTS. A Randomized Trial of Telenursing to Reduce Hospitalization for Heart Failure: Patient-Centered Outcomes and Nursing Indicators. Home Health Care Serv Q (2003) 22(1):1–20. 10.1300/J027v22n01_01
125.
SheaSWeinstockRSTeresiJAPalmasWStarrenJCiminoJJet alA Randomized Trial Comparing Telemedicine Case Management With Usual Care in Older, Ethnically Diverse, Medically Underserved Patients With Diabetes Mellitus: 5 Year Results of the IDEATel Study. J Am Med Inform Assoc (2009) 16(4):446–56. 10.1197/jamia.M3157
126.
SheaSWeinstockRSStarrenJTeresiJPalmasWFieldLet alA Randomized Trial Comparing Telemedicine Case Management With Usual Care in Older, Ethnically Diverse, Medically Underserved Patients With Diabetes Mellitus. J Am Med Inform Assoc (2006) 13(1):40–51. 10.1197/jamia.M1917
127.
AgmonMPerryCKPhelanEDemirisGNguyenHQ. A Pilot Study of Wii Fit Exergames to Improve Balance in Older Adults. J Geriatr Phys Ther (2011) 34(4):161–7. 10.1519/JPT.0b013e3182191d98
128.
SchoeneDLordSRDelbaereKSeverinoCDaviesTASmithST. A Randomized Controlled Pilot Study of Home-Based Step Training in Older People Using Videogame Technology. PLoS One (2013) 8(3):e57734. 10.1371/journal.pone.0057734
129.
SchoeneDLordSRVerhoefPSmithST. A Novel Video Game-Based Device for Measuring Stepping Performance and Fall Risk in Older People. Arch Phys Med Rehabil (2011) 92(6):947–53. 10.1016/j.apmr.2011.01.012
130.
DiaoYLouNLiangSZhangYNingYLiGet alA Novel Environment-Adaptive Timed Up and Go Test System for Fall Risk Assessment With Wearable Inertial Sensors. IEEE Sens J (2021) 21(16):18287–97. 10.1109/jsen.2021.3082982
131.
OhtaSNakamoto’HShinagawaYTanikawaT. A Health Monitoring System for Elderly People Living Alone. J Telemed Telecare (2001) 8:151–6. 10.1177/1357633X0200800305
132.
AlmNDyeRGowansGCampbellJAstellAEllisM. A Communication Support System for Older People With Dementia. Computer (2007) 40:35–41. 10.1109/mc.2007.153
133.
PichierriGMurerKDe BruinED. A Cognitive-Motor Intervention Using a Dance Video Game to Enhance Foot Placement Accuracy and Gait Under Dual Task Conditions in Older Adults: A Randomized Controlled Trial. BMC Geriatr (2012) 12:74. 10.1186/1471-2318-12-74
134.
HainesTPRussellTBrauerSGErwinSLanePUrrySet alEffectiveness of a Video-Based Exercise Programme to Reduce Falls and Improve Health-Related Quality of Life Among Older Adults Discharged From Hospital: A Pilot Randomized Controlled Trial. Clin Rehabil (2009) 23(11):973–85. 10.1177/0269215509338998
135.
World Health Organization. WHO Clinical Consortium on Healthy Ageing 2019. In: Report of Consortium meeting; 21–22 November 2019; Geneva, Switzerland (2019). Available from: http://apps.who.int/bookorders (Accessed June 12, 2024).
136.
World Health Organization. Regional Action Plan on Healthy Ageing in the Western Pacific. 2021.
137.
World Health Organization. Integrated Care for Older People (ICOPE): Guidance for Person-Centred Assessment and Pathways in Primary Care. 2019.
138.
WambuiN. Medical Identification and Sensing Technology for Assisting and E-Health Monitoring Systems for Disabled and Elderly Persons. J Biomed Sustain Healthc Appl (2022) 5:9–17. 10.53759/0088/jbsha202202002
139.
GrahamCMJonesN. Impact of IoT on Geriatric Telehealth. Working Old People (2020) 24(3):231–43. 10.1108/wwop-04-2020-0012
140.
WangCCChenJJ. Overcoming Technophobia in Poorly-Educated Elderly - the HELPS-Seniors Service Learning Program. Int J Automation Smart Tech (2015) 5(3):173–82. 10.5875/ausmt.v5i3.980
141.
EtchemendyDBañosRMBotellaCCastillaD. Programa de Revisión de Vida Apoyado en las Nuevas Tecnologías para las Personas Mayores: Una Aplicación de Tecnologías Positivas. Escr Psicol (2010) 3(2):1–7. 10.24310/espsiescpsi.v3i2.13336
142.
SpinsanteS. Home Telehealth in Older Patients With Heart Failure – Costs, Adherence, and Outcomes. Smart Homecare Technol Telehealth (2014) 93:93. 10.2147/shtt.s45318
143.
GiovanniLFrédériqueL-GAndreaSFrancescoBClaraCStewartJet alCan Technology-Based Services Support Long-Term Care Challenges in Home Care? Analysis of Evidence From Social Innovation Good Practices Across the EU: CARICT Project Summary Report. Luxembourg: Publications Office (2012). p. 108.
144.
JohnOYadufashijeC. E-health Biosensor Platform for Noninvasive Health Monitoring for the Elderly in Low Resource Setting. Int J Biomed Eng Sci (2018) 5(3/4):15–30. 10.5121/ijbes.2018.5402
145.
KnightAFouyaxisJJarradGBeskiKChoGBidargaddiN. Systems to Harness Digital Footprint to Elucidate and Facilitate Ageing in Place. In: Studies in Health Technology and Informatics. IOS Press (2018). p. 91–101. 10.3233/978-1-61499-845-7-91
146.
World Health Organization and International Telecommunication Union. Be He@lthy Be Mobile. In: A Handbook on How to Implement mDementia (2021). Available from: http://apps.who.int/bookorders (Accessed June 12, 2024).
147.
WatsonPBearparkTLingJ. The Impact of Rapid Response and Telecare Services on Elderly and Vulnerable Residents. Health Soc Care Community (2021) 29(4):897–904. 10.1111/hsc.13123
148.
PergolottiMDealAMBryantALBennettAVFarleyECovingtonKet alSenior Sway: Using a Mobile Application to Measure Fall Risk. J Geriatr Phys Ther (2019) 42(3):E101–7. 10.1519/JPT.0000000000000223
149.
SantanaRFDantasRVSoaresTDSDelphinoTMHerculesABSLeite JuniorHMT. Telecuidado para Idosos com Azheimer e seus Cuidadores: Revisão Sistemática/Telecare to Elderly People With Alzheimer and Their Caregivers: Systematic Review. Ciência, Cuidado e Saúde (2018) 17(4). 10.4025/cienccuidsaude.v17i4.41653
150.
CourtneyKLLinglerJHMeccaLPGarlockLASchulzRDickAWet alOlder Adults’ and Case Managers’ Initial Impressions of Community-Based Telehealth Kiosks. Res Gerontol Nurs (2010) 3(4):235–9. 10.3928/19404921-20100504-03
151.
KangGRKimIKKimWJLeeDY. Promotion of Adequate Exercise for Chronic Disorders’ Elderly Through Paced Music. In: Studies in Health Technology and Informatics. IOS Press (2017). p. 136–40. 10.3233/978-1-61499-830-3-136
152.
LindLCarlgrenGKarlssonD,Old-and With Severe Heart Failure. Telemonitoring by Using Digital Pen Technology in Specialized Homecare: System Description, Implementation, and Early Results. Comput Inform Nurs (2016). 10.1097/CIN.0000000000000252
153.
OgawaEFHarrisRDufourABMoreyMCBeanJ. Reliability of Virtual Physical Performance Assessments in Veterans During the COVID-19 Pandemic. Arch Rehabil Res Clin Transl (2021) 3(3):100146. 10.1016/j.arrct.2021.100146
154.
ZieglerPStierandKBahrsCAhrendMD. Mid-Term Results After Proximal Humeral Fractures Following Angular Stable Plate Fixation in Elderly Patients - Which Scores Can Be Evaluated by a Telephone-Based Assessment?J Orthop Surg Res (2020) 15(1):6. 10.1186/s13018-019-1536-8
155.
Pinero De PlazaMABeleigoliAMuddATieuMMcMillanPLawlessMet alNot Well Enough to Attend Appointments: Telehealth Versus Health Marginalisation. In: Studies in Health Technology and Informatics. Amsterdam, Netherlands: IOS Press BV (2021). p. 72–9.
156.
TousignantMBoissyPCorriveauHMoffetH. In Home Telerehabilitation for Older Adults After Discharge From an Acute Hospital or Rehabilitation Unit: A Proof-Of-Concept Study and Costs Estimation. Disabil Rehabil Assist Technol (2006) 1(4):209–16. 10.1080/17483100600776965
157.
World Health Organization. Be He@lthy Be Mobile: A Handbook on How to Implement mAgeing (2018). Available from: http://apps.who.int/bookorders.
158.
World Health Organization. Age-Friendly Environments in Europe: A Handbook of Domains for Policy Action. Copenhagen, Denmark: Health Organization Regional Office for Europe (2017). Available from: http://www.euro.who.int/pubrequest (Accessed June 12, 2024).
159.
DamantJKnappMWattersSFreddolinoPEllisMKingD. The Impact of ICT Services on Perceptions of the Quality of Life of Older People. J Assist Technol (2013) 7(1):5–21. 10.1108/17549451311313183
160.
MeleCRusso-SpenaTMarzulloMLRuggieroA. Boundary Work in Value Co-Creation Practices: The Mediating Role of Cognitive Assistants. J Serv Manag (2022) 33(2):342–62. 10.1108/josm-10-2020-0381
161.
MarraDEHamletKMBauerRMBowersD. Validity of Teleneuropsychology for Older Adults in Response to COVID-19: A Systematic and Critical Review. Clin Neuropsychologist (2020) 34:1411–52. 10.1080/13854046.2020.1769192
162.
AilyJBBartonCJMattielloSMSilvaDde ODe NoronhaM. Telerehabilitation for Knee Osteoarthritis in Brazil: A Feasibility Study. Int J Telerehabil (2020) 12(2):137–48. 10.5195/ijt.2020.6323
163.
HostengKRSimmeringJEPolgreenLACremerJFSegreAMFrancisSLet alMultilevel Mhealth Intervention Increases Physical Activity of Older Adults Living in Retirement Community. J Phys Act Health (2021) 18(7):851–7. 10.1123/jpah.2020-0592
164.
HaradaNDDhananiSElrodMHahnTKleinmanLFangM. Feasibility Study of Home Telerehabilitation for Physically Inactive Veterans. J Rehabil Res Dev (2010) 47(5):465–75. 10.1682/jrrd.2009.09.0149
165.
TousignantMMarquisNPagéCImukuzeNMétivierASt-OngeVet alIn-home Telerehabilitation for Older Persons With Chronic Obstructive Pulmonary Disease: A Pilot Study. Int J Telerehabil (2012) 13:15–24. 10.5195/ijt.2012.6083
166.
LevyCESilvermanEJiaHGeissMOmuraD. Effects of Physical Therapy Delivery via Home Video Telerehabilitation on Functional and Health-Related Quality of Life Outcomes. J Rehabil Res Dev (2015) 52(3):361–70. 10.1682/JRRD.2014.10.0239
167.
MoffetHTousignantMNadeauSMéretteCBoissyPCorriveauHet alIn-Home Telerehabilitation Compared With Faceto-Face Rehabilitation After Total Knee Arthroplasty: A Noninferiority Randomized Controlled Trial. J Bone Jt Surg - Am (2015) 97(14):1129–41. 10.2106/JBJS.N.01066
168.
FlynnAPrestonEDennisSCanningCGAllenNE. Home-Based Exercise Monitored With Telehealth Is Feasible and Acceptable Compared to Centre-Based Exercise in Parkinson’s Disease: A Randomised Pilot Study. Clin Rehabil (2021) 35(5):728–39. 10.1177/0269215520976265
169.
BesnierFGaydaMNigamAJuneauMBhererL. Cardiac Rehabilitation During Quarantine in COVID-19 Pandemic: Challenges for Center-Based Programs. Arch Phys Med Rehabil (2020) 101:1835–8. 10.1016/j.apmr.2020.06.004
170.
TurnerAPWallinMTSloanAMaloniHKaneRMartzLet alClinical Management of Multiple Sclerosis Through Home Telehealth Monitoring Results of a Pilot Project. Int J MS Care (2013) 15(1):8–14. 10.7224/1537-2073.2012-012
171.
DahlgrenKHolzmannMJCarlssonACWändellPHasselströmJRugeT. The Use of a Swedish Telephone Medical Advice Service by the Elderly–A Population-Based Study. Scand J Prim Health Care (2017) 35(1):98–104. 10.1080/02813432.2017.1288816
172.
HutchinsonMWendtNSmithST. Trial Implementation of a Telerehabilitation Exercise System in Residential Aged Care. In: Studies in Health Technology and Informatics. IOS Press (2018). p. 62–74. 10.3233/978-1-61499-845-7-62
173.
WatersonPEasonKTuttDDentM. Using HIT to Deliver Integrated Care for the Frail Elderly in the UK: Current Barriers and Future Challenges. In: Work (2012). p. 4490–3.
174.
SöderlundR. The Role of Information and Communication Technology in Home Services: Telecare Does Not Satisfy the Needs of the Elderly. Health Inform J (2004) 10(2):127–37. 10.1177/1460458204042237
175.
UnbehaunDTaugerbeckSAalKVaziriDDLehmannJTolmiePet alNotes of Memories: Fostering Social Interaction, Activity and Reminiscence Through an Interactive Music Exergame Developed for People With Dementia and Their Caregivers. Hum Comput Interact (2021) 36(5–6):439–72. 10.1080/07370024.2020.1746910
176.
LexisMEverinkIVan Der HeideLSpreeuwenbergMWillemsCDe WitteL. Activity Monitoring Technology to Support Homecare Delivery to Frail and Psychogeriatric Elderly Persons Living at Home Alone. Technol Disabil (2013) 25(3):189–97. 10.3233/tad-130377
177.
QueyrouxASaricassapianBHerzogDMüllerKHerafaIDucouxDet alAccuracy of Teledentistry for Diagnosing Dental Pathology Using Direct Examination as a Gold Standard: Results of the Tel-E-Dent Study of Older Adults Living in Nursing Homes. J Am Med Dir Assoc (2017) 18(6):528–32. 10.1016/j.jamda.2016.12.082
178.
JaanaMSherrardHParéG. A Prospective Evaluation of Telemonitoring Use by Seniors With Chronic Heart Failure: Adoption, Self-Care, and Empowerment. Health Inform J. (2019) 25(4):1800–14. 10.1177/1460458218799458
179.
SuhMKChenCAWoodbridgeJTuMKKimJINahapetianAet alA Remote Patient Monitoring System for Congestive Heart Failure. J Med Syst (2011). p. 1165–79. 10.1007/s10916-011-9733-y
180.
De LucaRTorrisiMBramantiAMaggioMGAnchesiSAndaloroAet alA Multidisciplinary Telehealth Approach for Community Dwelling Older Adults. Geriatr Nurs (Minneap) (2021) 42(3):635–42. 10.1016/j.gerinurse.2021.03.015
181.
LeeDTFLeungDYPLeeIFKLamLWLeeSWYChanMWMet alThe Impact of Virtual Wards on Frail Older Patients With Chronic Diseases at Home: A Pre and Post Study. Age Ageing (2014) 43:i4. 10.1093/ageing/afu036.15
182.
BarrettEBurkeMWhelanSSantorelliAOliveiraBLCavalloFet alEvaluation of a Companion Robot for Individuals With Dementia: Quantitative Findings of the MARIO Project in an Irish Residential Care Setting. J Gerontol Nurs (2019) 47(7):36–45. 10.3928/00989134-20190531-01
183.
GrahamSAJesteDVLeeEEWuTCTuXKimHCet alAssociations Between Heart Rate Variability Measured With a Wrist-Worn Sensor and Older Adults’ Physical Function: Observational Study. JMIR Mhealth Uhealth (2019) 7(10):e13757. 10.2196/13757
184.
GrossmanMRZakDKZelinskiEM. Mobile Apps for Caregivers of Older Adults: Quantitative Content Analysis. JMIR Mhealth Uhealth (2018) 6(7):e162. 10.2196/mhealth.9345
185.
SadasivamRSLugerTMColeyHLTaylorBBPadirTRitchieCSet alRobot-Assisted Home Hazard Assessment for Fall Prevention: A Feasibility Study. J Telemed Telecare (2014) 20(1):3–10. 10.1177/1357633X13517350
186.
HauxRHeinAKolbGKünemundHEichelbergMAppellJEet alInformation and Communication Technologies for Promoting and Sustaining Quality of Life, Health and Self-Sufficiency in Ageing Societies-Outcomes of the Lower Saxony Research Network Design of Environments for Ageing (GAL). Inform Health Soc Care (2014) 39(3–4):166–87. 10.3109/17538157.2014.931849
187.
HantonCRKwonYJAungTWhittingtonJHighRRGouldingEHet alMobile Phone-Based Measures of Activity, Step Count, and Gait Speed: Results From a Study of Older Ambulatory Adults in a Naturalistic Setting. JMIR Mhealth Uhealth (2017) 5(10):e104. 10.2196/mhealth.5090
188.
BlixenCEBramstedtKAHammelJPTilleyBC. A Pilot Study of Health Education via a Nurse-Run Telephone Self-Management Programme for Elderly People With Osteoarthritis. J Telemed Telecare (2004) 10:44–9. 10.1258/135763304322764194
189.
NiQHernandoABGde la CruzIP. The Elderly’s Independent Living in Smart Homes: A Characterization of Activities and Sensing Infrastructure Survey to Facilitate Services Development. Sensors (Switzerland) (2015) 15:11312–62. 10.3390/s150511312
190.
SuzukiRHasegawaT. Evaluation of a One-Dose Package Medication Support System for Community-Based Elderly Patients and Eldercare Facilities. Am J Health-System Pharm (2018) 75(9):e202–12. 10.2146/ajhp170176
191.
BeckerTACTeixeiraCRde SZanettiMLPaceAEAlmeidaFATorquatoMTet alEffects of Supportive Telephone Counseling in the Metabolic Control of Elderly People With Diabetes Mellitus. Rev Bras Enferm (2017) 70(4):704–10. 10.1590/0034-7167-2017-0089
192.
Van Doorn-Van AttenMNHaveman-NiesAVan BakelMMFerryMFrancoMDe GrootLCPGMet alEffects of a Multi-Component Nutritional Telemonitoring Intervention on Nutritional Status, Diet Quality, Physical Functioning and Quality of Life of Community-Dwelling Older Adults. Br J Nutr (2018) 119(10):1185–94. 10.1017/S0007114518000843
193.
MullenEC. Effect of Telephone Counseling on Physical Activity Among Older Effect of Telephone Counseling on Physical Activity Among Older Adult Cancer Survivors Adult Cancer Survivors. Available from: http://hdl.handle.net/10950/97 (Accessed March 5, 2024).
194.
ChangKCHungSHHsuehSJChaoSFHuangWLChenHSet alDevelopment of the Houston–Apollo Model for Older People Living in Remote Areas in Taiwan. Geriatr Gerontol Int (2021) 21(3):299–305. 10.1111/ggi.14130
195.
BordaAGilbertCGrayKPrabhuD. In: van den BergMELMaederAJ, editors. Consumer Wearable Information and Health Self Management by Older Adults. IOS Press (2018). 10.3233/978-1-61499-845-7-42
196.
SteilsNWoolhamJFiskMPorteusJForsythK. Carers’ Involvement in Telecare Provision by Local Councils for Older People in England: Perspectives of Council Telecare Managers and Stakeholders. Ageing Soc (2021) 41(2):456–75. 10.1017/s0144686x1900120x
197.
ZacharopoulouGZacharopoulouVDermatisZLazakidouA. Adoption of ICT by Elderly With Hip Fracture After a Fall. Stud Health Technol Inform (2018) 251:191–4.
198.
VolandesAEZupancSNPaasche-OrlowMKLakinJRChangYBurnsEAet alAssociation of an Advance Care Planning Video and Communication Intervention With Documentation of Advance Care Planning Among Older Adults: A Nonrandomized Controlled Trial. JAMA Netw Open (2022) 5(2):e220354. 10.1001/jamanetworkopen.2022.0354
199.
BendixenRM. Assessment of a Telerehabilitation and a Telehomecare Program for Veterans With Chronic Illnesses. Florida, United States: University of Florida (2006).
200.
YasiniMMarchandG. Adoption and Use of a Mobile Health Application in Older Adults for Cognitive Stimulation. In: Studies in Health Technology and Informatics. IOS Press (2016). p. 13–7. 10.3233/978-1-61499-633-0-13
201.
GoumopoulosCPapaIStavrianosA. Development and Evaluation of a Mobile Application Suite for Enhancing the Social Inclusion and Well-Being of Seniors. Informatics (2017) 4(3):15. 10.3390/informatics4030015
202.
VaziriDDAalKGschwindYJDelbaereKWeibertAAnnegarnJet alAnalysis of Effects and Usage Indicators for a ICT-Based Fall Prevention System in Community Dwelling Older Adults. Int J Hum Comput Stud (2017) 106:10–25. 10.1016/j.ijhcs.2017.05.004
203.
KleinpellRMAvitallB. Integrating Telehealth as a Strategy for Patient Management After Discharge for Cardiac Surgery Results of a Pilot Study. J Cardiovasc Nurs (2007) 22:38–42. 10.1097/00005082-200701000-00006
204.
ResnickHEIlaganPRKaylorMBMehlingDAlwanM. TEAhM-Technologies for Enhancing Access to Health Management: A Pilot Study of Community-Based Telehealth. Telemed e-Health (2012) 18(3):166–74. 10.1089/tmj.2011.0122
205.
JarvisMAChippsJPadmanabhanunniA. “This Phone Saved My Life”: Older Persons Experiences and Appraisals of an mHealth Intervention Aimed at Addressing Loneliness. J Psychol Africa (2019) 29(2):159–66. 10.1080/14330237.2019.1594650
206.
EtchemendyEBañosRMBotellaCCastillaDAlcañizMRasalPet alAn E-Health Platform for the Elderly Population: The Butler System. Comput Educ (2011) 56(1):275–9. 10.1016/j.compedu.2010.07.022
207.
ZulfiqarAAHajjamATalhaSHajjamMHajjamJErvéSet alTelemedicine and Geriatrics in France: Inventory of Experiments. Curr Gerontol Geriatr Res (2018) 2018:9042180. 10.1155/2018/9042180
208.
KangHGMahoneyDFHoenigHHirthVABonatoPHajjarIet alIn Situ Monitoring of Health in Older Adults: Technologies and Issues. J Am Geriatr Soc (2010) 58:1579–86. 10.1111/j.1532-5415.2010.02959.x
209.
ParfittJWanADarziAParfittJShafiAde CauxRet alThe Use of Wireless Telemedicine Equipment in the Senior Assessment of Surgical Patients in an Accident and Emergency Department. J Telemed Telecare (2001) 7:82. 10.1177/1357633x010070s140
210.
YoshidaKYamaokaYEguchiYSatoDIiboshiKKishimotoMet alRemote Neuropsychological Assessment of Elderly Japanese Population Using the Alzheimer’s Disease Assessment Scale: A Validation Study. J Telemed Telecare (2020) 26(7–8):482–7. 10.1177/1357633X19845278
211.
GeraedtsHAEDijkstraHZhangWIbarraFFarIKZijlstraWet alEffectiveness of an Individually Tailored Home-Based Exercise Rogramme for Pre-Frail Older Adults, Driven by a Tablet Application and Mobility Monitoring: A Pilot Study. Eur Rev Aging Phys Activity (2021) 18(1):10. 10.1186/s11556-021-00264-y
212.
MshaliHLemloumaTMoloneyMMagoniD. A Survey on Health Monitoring Systems for Health Smart Homes. Int J Ind Ergon (2018) 66:26–56. 10.1016/j.ergon.2018.02.002
213.
ChoiSDGuoLKangDXiongS. Exergame Technology and Interactive Interventions for Elderly Fall Prevention: A Systematic Literature Review. Appl Ergon (2017) 65:570–81. 10.1016/j.apergo.2016.10.013
214.
WernerCMoustrisGPTzafestasCSHauerK. User-Oriented Evaluation of a Robotic Rollator That Provides Navigation Assistance in Frail Older Adults With and Without Cognitive Impairment. Gerontology (2018) 64(3):278–90. 10.1159/000484663
215.
PietteJDStriplinDMarinecNChenJAikensJE. A Randomized Trial of Mobile Health Support for Heart Failure Patients and Their Informal Caregivers Impacts on Caregiver-Reported Outcomes. Med Care (2015) 53:692–9. 10.1097/MLR.0000000000000378
216.
SparsaADoffoel-HantzVBonnetblancJM. Assessment of Tele-Expertise Among Elderly Subjects in Retirement Homes (EHPAD). Ann Dermatol Venereol (2013) 140(3):165–9. 10.1016/j.annder.2012.11.008
217.
ShahbaziMBagherianHSattariMSaghaeiannejad-IsfahaniS. The Opportunities and Challenges of Using Mobile Health in Elderly Self-Care. J Educ Health Promot (2021) 10(1):80. 10.4103/jehp.jehp_871_20
218.
IntawongKBoonchiengWLerttrakarnnonPBoonchiengEPuritatK. A- SA SOS: A Mobile and IoT-Based Pre-Hospital Emergency Service for the Elderly and Village Health Volunteers. Int J Adv Comput Sci Appl (2021) 12(4):513–8. 10.14569/ijacsa.2021.0120465
219.
TindallLRHuebnerRAStempleJCKleinertHL. Videophone-Delivered Voice Therapy: A Comparative Analysis of Outcomes to Traditional Delivery for Adults With Parkinson’s Disease. Telemed e-Health (2008) 14(10):1070–7. 10.1089/tmj.2008.0040
220.
NancarrowSBanburyABuckleyJ. Evaluation of a National Broadband Network-Enabled Telehealth Trial for Older People With Chronic Disease. Aust Health Rev (2016) 40(6):641–8. 10.1071/AH15201
221.
GrossiGLanzarottiRNapoletanoPNocetiNOdoneF. Positive Technology for Elderly Well-Being: A Review. Pattern Recognit Lett (2020) 137:61–70. 10.1016/j.patrec.2019.03.016
222.
Reading TurchioeMGrossmanLVBaikDLeeCSMaurerMSGoyalPet alOlder Adults Can Successfully Monitor Symptoms Using an Inclusively Designed Mobile Application. J Am Geriatr Soc (2020) 68(6):1313–8. 10.1111/jgs.16403
223.
WhitehouseCRLongJAMaloneyLMDanielsKHorowitzDABowlesKH. Feasibility of Diabetes Self-Management Telehealth Education for Older Adults During Transitions in Care. Res Gerontol Nurs (2020) 13(3):138–45. 10.3928/19404921-20191210-03
224.
ZhouSOgiharaANishimuraSJinQ. Analyzing the Changes of Health Condition and Social Capital of Elderly People Using Wearable Devices. Health Inf Sci Syst (2018) 6(1):4. 10.1007/s13755-018-0044-2
225.
HsuMHChuTBYenJCChiuWTYehGCChenTJet alDevelopment and Implementation of a National Telehealth Project for Long-Term Care: A Preliminary Study. Comput Methods Programs Biomed (2010) 97(3):286–92. 10.1016/j.cmpb.2009.12.008
226.
KimHHChoNBKimJKimKMKangMChoiYet alImplementation of a Home-Based Mhealth App Intervention Program With Human Mediation for Swallowing Tongue Pressure Strengthening Exercises in Older Adults: Longitudinal Observational Study. JMIR Mhealth Uhealth (2020) 8(10):e22080. 10.2196/22080
227.
HongEJakacicANSahooABreymanEUkegbuGTabacofLet alUse of Fitbit Technology Does Not Impact Health Biometrics in a Community of Older Adults. Telemed e-Health (2021) 27(4):409–13. 10.1089/tmj.2020.0060
228.
RochaLAAlmeidaSS. Saphiraweb: An Open-Source Cloud Platform for E-Health Analysis. Instrum Sci Technol (2020) 48(6):583–600. 10.1080/10739149.2020.1761380
229.
CidASoteloRLeguisamoMRamírez-MichelenaM. Tablets for Deeply Disadvantaged Older Adults: Challenges in Long-Term Care Facilities. Int J Hum Comput Stud (2020) 144. 10.1016/j.ijhcs.2020.102504
230.
ZulfiqarAAMassimboDNDHajjamMGenyBTalhaSHajjamJet alResults of the Second Phase of the Ger-E-Tec Experiment Concerning the Telemonitoring of Elderly Patients Affected by Covid-19 Disease to Detect the Exacerbation of Geriatric Syndromes. J Pers Med (2021) 11(11):1117. 10.3390/jpm11111117
231.
ZulfiqarAAVaudelleOHajjamMGenyBTalhaSLetourneauDet alResults of the “GER-e-TEC” Experiment Involving the Use of an Automated Platform to Detect the Exacerbation of Geriatric Syndromes. J Clin Med (2020) 9(12):3836–17. 10.3390/jcm9123836
232.
TabbaraMÖzgülerOSExadaktylosAK. New Freedom Through Medical Devices Based on the Global System for Mobile Communications: A Prospective Survey of 620 Users of the Swiss Limmex Emergency Wristwatch—An Original Study From Switzerland. Emerg Med Int (2013) 2013:563731–4. 10.1155/2013/563731
233.
Van ’t KloosterJWJRVan Der HeideLAVan ’t KloosterJWVan BruinessenIBoessenAVan Der HeideLet alIntroducing Personalised Self-Management to Support Physical Activity in Elderly: A Case Study. In: International Conference E-Health (2017). Available from: https://www.researchgate.net/publication/319137123 (Accessed July 18, 2023).
234.
DorrianCMcgibbonF. Lochaber Telemedicine Clinic-A New Approach Managing Dementia in Care Homes Conference Abstract Lochaber Telemedicine Clinic-A New Approach Managing Dementia in Care Homes. International Congress on Telehealth and Telecare (2013). Available from: https://www.researchgate.net/publication/296705067 (Accessed July 18, 2023). 10.5334/ijic.1412
235.
Pearlman-AvnionSGoldschmidtYShamisN. Impacts of Urbanization and ICT Use on Loneliness Among the Elderly in Israel. Educ Urban Soc (2020) 52(6):962–83. 10.1177/0013124519891998
236.
SaccaviniCMancinS. Integration of Telehealth and Telecare Service in the Veneto Region. Int J Integr Care (2013) 13. 10.5334/ijic.1426
237.
StellatoKRadiniDPellizzariMPordenonMPlettiLHumarFet alIntegrating Care in Complex Cardiac Care: The Tech Touch. Int J Integr Care (2016) 16(6):383. 10.5334/ijic.2931
238.
GrisSSampognaroEForestieroASaccaviniCMancinS. Improving Integrated Care for Frail Elderly Patients Throught Ict – The Veneto Region Experience. Int J Integr Care (2017) 17(5):520. 10.5334/ijic.3840
239.
YeungAJohnsonDPTrinhNHWengWCCKvedarJFavaM. Feasibility and Effectiveness of Telepsychiatry Services for Chinese Immigrants in a Nursing Home. Telemed e-Health. (2009) 15(4):336–41. 10.1089/tmj.2008.0138
240.
SalernoD. Development of E-Health Services and Integrated/Coordinated Cares. Int J Integr Care (2015) 15. 10.5334/ijic.2144
241.
RobičMPavličDR. COVID-19 and Care for the Elderly in Long-Term Care Facilities: The Role Information Communication Technology. Acta Med Academica. Acad Sci Arts Bosnia Herzegovina (2021) 50:414–22. 10.5644/ama2006-124.363
242.
CaseyJ. Carers Assistive Technology Service. In: International Digital Health and Care Congress. London (2014). Available from: http://www.ijic.org/ (Accessed July 18, 2023).
243.
SloneSMarshallKGracePWallG. Avoidance of Unnecessary Hospital Admissions Through the Implementation of a Digital Health Programme. Int J Integr Care (2018) 18(s2):219. 10.5334/ijic.s2219
244.
SaracchiniRCatalinaCBordoniL. A Mobile Augmented Reality Assistive Technology for the Elderly. Comunicar (2015) 23(45):65–73. 10.3916/C45-2015-07
245.
Vázquez-De SebastiánJCiudinACastellano-TejedorC. Analysis of Effectiveness and Psychological Techniques Implemented in Mhealth Solutions for Middle-Aged and Elderly Adults With Type 2 Diabetes: A Narrative Review of the Literature. J Clin Med (2021) 10:2701. 10.3390/jcm10122701
246.
ScherrDKastnerPKollmannAHallasAAuerJKrappingerHet alEffect of Home-Based Telemonitoring Using Mobile Phone Technology on the Outcome of Heart Failure Patients After an Episode of Acute Decompensation: Randomized Controlled Trial. J Med Internet Res (2009) 11(3):e34. 10.2196/jmir.1252
247.
MagnussonLHansonEBorgM. A literature review study of Information and Communication Technology as a support for frail older people living at home and their family carers. Technology and Disability (2004) 16(4):223–235. 10.3233/TAD-2004-16404
248.
EgedeLEAciernoRKnappRGWalkerRJPayneEHChristopher FruehB. Psychotherapy for Depression in Older Veterans via Telemedicine: Effect on Quality of Life, Satisfaction, Treatment Credibility, and Service Delivery Perception. J Clin Psychiatry (2016) 77(12):1704–11. 10.4088/JCP.16m10951
249.
AntonicelliRMazzantiIAbbatecolaAMParatiG. Impact of Home Patient Telemonitoring on Use of β-Blockers in Congestive Heart Failure. Drugs Aging (2010) 27(10):801–5. 10.2165/11538210-000000000-00000
250.
TriefPMIzquierdoREimickeJPTeresiJAGolandRPalmasWet alAdherence to Diabetes Self Care for White, African-American and Hispanic American Telemedicine Participants: 5 Year Results From the IDEATel Project. Ethn Health (2013) 18(1):83–96. 10.1080/13557858.2012.700915
251.
CarreteroSCentenoCStewartJ. Telecare and Telehealth for Informal Carers: A Research in 12 Member States on Their Benefits and Policy Role for the Success. Int J Integr Care (2013) 13(7). 10.5334/ijic.1374
252.
PoonPHuiEDaiDKwokTWooJ. Cognitive Intervention for Community-Dwelling Older Persons With Memory Problems: Telemedicine Versus Face-To-Face Treatment. Int J Geriatr Psychiatry (2005) 20(3):285–6. 10.1002/gps.1282
253.
WestSPLaguaCTriefPMIzquierdoRWeinstockRS. Goal Setting Using Telemedicine in Rural Underserved Older Adults With Diabetes: Experiences From the Informatics for Diabetes Education and Telemedicine Project. Available from: www.liebertpub.com (Accessed July 19, 2023).
254.
ZaccarelliCBenatiGBoschiFBarbanFAnnicchiaricoRLymperopoulouO. Computer-Based Cognitive Training for Dementia. Results From a Randomized Controlled Trial on MCI, Mild AD and Healthy Ageing. In: Journal of Alzheimer’s Disease. IOS Press (2016). p. S56. 10.3233/JAD-169001
255.
Comín-ColetJEnjuanesCVerdú-RotellarJMLinasARuiz-RodriguezPGonzález-RobledoGet alImpact on Clinical Events and Healthcare Costs of Adding Telemedicine to Multidisciplinary Disease Management Programmes for Heart Failure: Results of a Randomized Controlled Trial. J Telemed Telecare (2016) 22(5):282–95. 10.1177/1357633X15600583
256.
JenkinsRMcSweeneyM. Assessing Elderly Patients With Congestive Heart Failure via in-Home Interactive Telecommunication. J Gerontol Nurs (2001) 27:21–7. 10.3928/0098-9134-20010101-09
257.
GathercoleRBradleyRHarperEDaviesLPankLLamNet alAssistive Technology and Telecare to Maintain Independent Living at Home for People With Dementia: The ATTILA RCT. Health Technol Assess (Rockv) (2021) 25(19):1–156. 10.3310/hta25190
258.
PedoneCChiurcoDScarlataSIncalziRA. Efficacy of Multiparametric Telemonitoring on Respiratory Outcomes in Elderly People With COPD: A Randomized Controlled Trial. BMC Health Serv Res (2013) 13:82. 10.1186/1472-6963-13-82
259.
AntonicelliRTestarmataPSpazzafumoLGagliardiCBiloGValentiniMet alImpact of Telemonitoring at Home on the Management of Elderly Patients With Congestive Heart Failure. J Telemed Telecare (2008) 14(6):300–5. 10.1258/jtt.2008.071213
260.
SabatierRCoutanceGBelinABiannicCLoiseletPPradereGet alThree Months Educational Remote Telemonitoring in Elderly Patients With Heart Failure Reduces Hospitalizations for Acute Heart Failure at One Year: A Randomized Trial. P666. In: European Journal of Heart Failure. Wiley (2013).
261.
MavandadiSBensonADiFilippoSStreimJEOslinD. A Telephone-Based Program to Provide Symptom Monitoring Alone vs Symptom Monitoring Plus Care Management for Late-Life Depression and Anxiety a Randomized Clinical Trial. JAMA Psychiatry (2015) 72(12):1211–8. 10.1001/jamapsychiatry.2015.2157
262.
ZeghariRGuerchoucheRTran DucMBremondFLemoineMPBultingaireVet alPilot Study to Assess the Feasibility of a Mobile Unit for Remote Cognitive Screening of Isolated Elderly in Rural Areas. Int J Environ Res Public Health (2021) 18(11):6108. 10.3390/ijerph18116108
263.
SharmaYThompsonCHKaambwaBShahiRHakendorfPMillerM. Investigation of the Benefits of Early Malnutrition Screening With Telehealth Follow up in Elderly Acute Medical Admissions. QJM: Int J Med (2017) 110(10):639–47. 10.1093/qjmed/hcx095
264.
TriefPMTeresiJAIzquierdoRMorinPCGolandRFieldLet alPsychosocial Outcomes of Telemedicine Case Management for Elderly Patients With Diabetes: The Randomized IDEATel Trial. Diabetes Care (2007) 30:1266–8. 10.2337/dc06-2476
265.
MandalANgNMokVLantzMSinaiMIsraelBet al“Put It on Mi Tab”: Assessing the Cost of Geriatric “Regulars” in the Psychiatric Emergency Department. In: AAGP Annual Meeting (2019).
266.
NoelHCVogelDCErdosJJCornwallDLevinF. Home Telehealth Reduces Healthcare Costs. Telemed J E Health (2004) 10:170–83. 10.1089/tmj.2004.10.170
267.
HiraniSPBeynonMCartwrightMRixonLDollHHendersonCet alThe Effect of Telecare on the Quality of Life and Psychological Well-Being of Elderly Recipients of Social Care over a 12-Month Period: The Whole Systems Demonstrator Cluster Randomised Trial. Age Ageing (2014) 43(3):334–41. 10.1093/ageing/aft185
268.
GellisZDKenaleyBLHaveTT. Integrated Telehealth Care for Chronic Illness and Depression in Geriatric Home Care Patients: The Integrated Telehealth Education and Activation of Mood (I-TEAM) Study. J Am Geriatr Soc (2014) 62(5):889–95. 10.1111/jgs.12776
269.
SorknaesADBechMMadsenHTitlestadILHounsgaardLHansen-NordMet alThe Effect of Real-Time Teleconsultations Between Hospital-Based Nurses and Patients With Severe COPD Discharged After an Exacerbation. J Telemed Telecare (2013) 19(8):466–74. 10.1177/1357633X13512067
270.
LinFCChienHYChenSHKaoYCChengPWTeWC. Voice Therapy for Benign Voice Disorders in the Elderly: A Randomized Controlled Trial Comparing Telepractice and Conventional Face-To-Face Therapy. J Speech, Lang Hearing Res (2020) 63(7):2132–40. 10.1044/2020_JSLHR-19-00364
271.
CasselS. A Comparison of Traditional Face-To-Face and Tele-Dysphagia Instructional Methods in Geriatric TBI and CVA Populations. Arch Phys Med Rehabil (2016) 97(10):e16–7. 10.1016/j.apmr.2016.08.046
272.
TitovNDearBFAliSZouJBLorianCNJohnstonLet alClinical and Cost-Effectiveness of Therapist-Guided Internet-Delivered Cognitive Behavior Therapy for Older Adults With Symptoms of Depression: A Randomized Controlled Trial. Behav Ther (2015) 46:193–205. 10.1016/j.beth.2014.09.008
273.
PedoneCRossiFFCecereACostanzoLAntonelli IncalziR. Efficacy of a Physician-Led Multiparametric Telemonitoring System in Very Old Adults With Heart Failure. J Am Geriatr Soc (2015) 63(6):1175–80. 10.1111/jgs.13432
274.
ChoiNGHegelMTNathan MartiCLynn MarinucciMSirrianniLBruceML. Telehealth Problem-Solving Therapy for Depressed Low-Income Homebound Older Adults. Am J Geriatr Psychiatry (2012) 1:1. 10.1097/jgp.0b013e318266b356
275.
LinKHChenCHChenYYHuangWTLaiJSYuSMet alBidirectional and Multi-User Telerehabilitation System: Clinical Effect on Balance, Functional Activity, and Satisfaction in Patients With Chronic Stroke Living in Long-Term Care Facilities. Sensors (Switzerland) (2014) 14(7):12451–66. 10.3390/s140712451
276.
BakerKLaValleyMPBrownCFelsonDTLedinghamAKeysorJJ. Efficacy of Computer-Based Telephone Counseling on Long-Term Adherence to Strength Training in Elderly Patients With Knee Osteoarthritis: A Randomized Trial. Arthritis Care Res (Hoboken) (2020) 72(7):982–90. 10.1002/acr.23921
277.
SparrowDGottliebDJDemollesDFieldingRA. Increases in Muscle Strength and Balance Using a Resistance Training Program Administered via a Telecommunications System in Older Adults. Journals Gerontol - Ser A Biol Sci Med Sci (2011) 66 A(11):1251–7. 10.1093/gerona/glr138
278.
JakobsenASLaursenLCRydahl-HansenSØstergaardBGerdsTAEmmeCet alHome-Based Telehealth Hospitalization for Exacerbation of Chronic Obstructive Pulmonary Disease: Findings From “The Virtual Hospital Trial”. Telemed e-Health (2015) 21(5):364–73. 10.1089/tmj.2014.0098
279.
OlivariZGiacomelliSGubianLMancinSVisentinEDi FrancescoVet alThe Effectiveness of Remote Monitoring of Elderly Patients After Hospitalisation for Heart Failure: The Renewing Health European Project. Int J Cardiol (2018) 257:137–42. 10.1016/j.ijcard.2017.10.099
280.
TieuCChaudhryRSchroederDRBockFAHansonGJTungEE. Utilization of Patient Electronic Messaging to Promote Advance Care Planning in the Primary Care Setting. Am J Hosp Palliat Med (2017) 34(7):665–70. 10.1177/1049909116650237
281.
ValdiviesoBGarcía-SempereASanfélix-GimenoGFaubelRLibreroJSorianoEet alThe Effect of Telehealth, Telephone Support or Usual Care on Quality of Life, Mortality and Healthcare Utilization in Elderly High-Risk Patients With Multiple Chronic Conditions. A Prospective Study. Med Clin (Barc) (2018) 151(8):308–14. 10.1016/j.medcli.2018.03.013
282.
BarnasonSZimmermanLNieveenJHertzogM. Impact of a Telehealth Intervention to Augment Home Health Care on Functional and Recovery Outcomes of Elderly Patients Undergoing Coronary Artery Bypass Grafting. Heart Lung J Acute Crit Care (2006) 35(4):225–33. 10.1016/j.hrtlng.2005.10.003
283.
PandeyAChoudhryN. An M-Health Application of Daily Text Messages to Address Forgetfulness as Contributor to Non-Adherence to Medications Post-Myocardial Infarction. In: Welcome to the Future: Technological Changes to Cardiovascular Health and Health Care (2015).
284.
GuoYLipGYH. Improving Outcomes With Integrated Care of Patients With Atrial Fibrillation and Multimorbidity Using Mobile Health Technology: A Report From the mAFA II Trial. Available from: https://academic.oup.com/eurheartj/article/42/Supplement_1/ehab724.3114/6391995 (Accessed July 5, 2023).
285.
ZimmermanLBarnasonSNieveenJSchmadererM. Symptom Management Intervention in Elderly Coronary Artery Bypass Graft Patients.
286.
ShanyTHessionMPryceDGalangRRobertsMLovellNet alHome Telecare Study for Patients With Chronic Lung Disease in the Sydney West Area Health Service. In: Studies in Health Technology and Informatics. IOS Press (2010). p. 139–48. 10.3233/978-1-60750-659-1-139
287.
FottrellEAhmedNMorrisonJKuddusAShahaSKKingCet alCommunity Groups or Mobile Phone Messaging to Prevent and Control Type 2 Diabetes and Intermediate Hyperglycaemia in Bangladesh (DMagic): A Cluster-Randomised Controlled Trial. Lancet Diabetes Endocrinol (2019) 7(3):200–12. 10.1016/S2213-8587(19)30001-4
288.
De KluiverEPVan Der VeldeAEMeindersmaEPPrinsLFWilhelmMIliouMCet alA European Randomised Controlled Trial for M-Health Guided Cardiac Rehabilitation in the Elderly; Results of the EU-CaRE RCT Study. In: ESC Congress 2019 Together with World Congress of Cardiology (2019). Available from: https://academic.oup.com/eurheartj/article/40/Supplement_1/ehz748.0674/5597461 (Accessed July 5, 2023).
289.
YuFMathiasonMAJohnsonKGauglerJEKlassenD. Memory Matters in Dementia: Efficacy of a Mobile Reminiscing Therapy App. Alzheimer’s Demen Translational Res Clin Interventions (2019) 5:644–51. 10.1016/j.trci.2019.09.002
290.
GschwindYJEichbergSEjupiAde RosarioHKrollMMarstonHRet alICT-Based System to Predict and Prevent Falls (iStoppFalls): Results From an International Multicenter Randomized Controlled Trial. Eur Rev Aging Phys Activity (2015) 12(1):10. 10.1186/s11556-015-0155-6
291.
Núñez-NaveiraLAlonso-BúaBDe LabraCGregersenRMaibomKMojsEet alUnderstAID, an ICT Platform to Help Informal Caregivers of People With Dementia: A Pilot Randomized Controlled Study. Biomed Res Int (2016) 2016:5726465. 10.1155/2016/5726465
292.
BrathHMorakJKästenbauerTModre-OsprianRStrohner-KästenbauerHSchwarzMet alMobile Health (mHealth) Based Medication Adherence Measurement - A Pilot Trial Using Electronic Blisters in Diabetes Patients. Br J Clin Pharmacol (2013) 76(S1):47–55. 10.1111/bcp.12184
293.
ChanMHMKeungDTFLuiSYTCheungRTH. A Validation Study of a Smartphone Application for Functional Mobility Assessment of the Elderly. Hong Kong Physiother J (2016) 35:1–4. 10.1016/j.hkpj.2015.11.001
294.
WadeMDesaiASpettellCMSnyderADMcGowan-StackewiczVKummerPJet alTelemonitoring With Case Management for Seniors With Heart Failure. Am J Manag Care (2011) 17(3):e71–e79.
295.
ShapiraSYeshua-KatzDCohn-SchwartzEAharonson-DanielLSaridOClarfieldAM. A Pilot Randomized Controlled Trial of a Group Intervention via Zoom to Relieve Loneliness and Depressive Symptoms Among Older Persons During the COVID-19 Outbreak. Internet Interv (2021) 24. 10.1016/j.invent.2021.100368
296.
ChanJYCChanTKWongMPFCheungRSMYiuKKLTsoiKKF. Effects of Virtual Reality on Moods in Community Older Adults. A Multicenter Randomized Controlled Trial. Int J Geriatr Psychiatry (2020) 35(8):926–33. 10.1002/gps.5314
297.
Pérez-RodríguezRGuevara-GuevaraTMoreno-SánchezPAVillalba-MoraEValdés-AragonésMOviedo-BrionesMet alMonitoring and Intervention Technologies to Manage Diabetic Older Persons: The CAPACITY Case—A Pilot Study. Front Endocrinol (Lausanne) (2020) 13:11. 10.3389/fendo.2020.00300
298.
GuoYChenYLaneDALiuLWangYLipGYH. Mobile Health Technology for Atrial Fibrillation Management Integrating Decision Support, Education, and Patient Involvement: mAF App Trial. Am J Med (2017) 130(12):1388–96. 10.1016/j.amjmed.2017.07.003
299.
LiXLiTChenJXieYAnXLvYet alA Wechat-Based Self-Management Intervention for Community Middle-Aged and Elderly Adults With Hypertension in Guangzhou, China: A Cluster-Randomized Controlled Trial. Int J Environ Res Public Health (2019) 16(21):4058. 10.3390/ijerph16214058
300.
FinkelsteinSMSpeedieSMZhouXPotthoffSRatnerER. Perception, Satisfaction and Utilization of the VALUE Home Telehealth Service. J Telemed Telecare (2011) 17(6):288–92. 10.1258/jtt.2011.100712
301.
GuoYLaneDAChenYLipGYHmAF-App II Trial investigators. Regular Bleeding Risk Assessment Associated With Reduction in Bleeding Outcomes: The mAFA-II Randomized Trial. Am J Med (2020) 133(10):1195–202.e2. 10.1016/j.amjmed.2020.03.019
302.
HermesSLurzMBöhmMKrcmarH. Evaluating the Usability and Usefulness of a Mobile Application for Training Visual Mnemonic Techniques in Participants With Subjective Cognitive Decline: An Exploratory Pilot Study. In: Procedia Computer Science. Elsevier B.V. (2019). p. 439–44.
303.
MiraJJNavarroIBotellaFBorrásFNuño-SolinísROrozcoDet alA Spanish Pillbox App for Elderly Patients Taking Multiple Medications: Randomized Controlled Trial. J Med Internet Res (2014) 16(4):e99. 10.2196/jmir.3269
304.
MertensABrandlCMiron-ShatzTSchlickCNeumannTKribbenAet alA Mobile Application Improves Therapy-Adherence Rates in Elderly Patients Undergoing Rehabilitation A Crossover Design Study Comparing Documentation via iPad With Paper-Based Control. Medicine (United States) (2016) 95(36):e4446. 10.1097/MD.0000000000004446
305.
RobertPManeraVDerreumauxAMontesinoMFYLeoneEFabreRet alEfficacy of a Web App for Cognitive Training (MEMO) Regarding Cognitive and Behavioral Performance in People With Neurocognitive Disorders: Randomized Controlled Trial. J Med Internet Res (2020) 22(3):e17167. 10.2196/17167
306.
KiJYJoSRChoKSParkJEChoJWJangJH. Effect of Oral Health Education Using a Mobile App (Ohema) on the Oral Health and Swallowing-Related Quality of Life in Community-Based Integrated Care of the Elderly: A Randomized Clinical Trial. Int J Environ Res Public Health (2021) 18(21):11679. 10.3390/ijerph182111679
307.
SnoekJAPrescottEIVan Der VeldeAEEijsvogelsTMHMikkelsenNPrinsLFet alEffectiveness of Home-Based Mobile Guided Cardiac Rehabilitation as Alternative Strategy for Nonparticipation in Clinic-Based Cardiac Rehabilitation Among Elderly Patients in Europe: A Randomized Clinical Trial. JAMA Cardiol (2021) 6(4):463–8. 10.1001/jamacardio.2020.5218
308.
YuJJeonHSongCHanW. Speech Perception Enhancement in Elderly Hearing Aid Users Using an Auditory Training Program for Mobile Devices. Geriatr Gerontol Int (2017) 17(1):61–8. 10.1111/ggi.12678
309.
TchallaAELachalFCardinaudNSaulnierIRialleVPreuxPMet alPreventing and Managing Indoor Falls With Home-Based Technologies in Mild and Moderate Alzheimer’s Disease Patients: Pilot Study in a Community Dwelling. Dement Geriatr Cogn Disord (2013) 36(3–4):251–61. 10.1159/000351863
310.
BerkmanPHeinikJRosenthalMBurkeM. Supportive Telephone Outreach as an Interventional Strategy for Elderly Patients in a Period of Crisis. Soc Work Health Care (1999) 28(4):63–76. 10.1300/J010v28n04_05
311.
TchallaAELachalFCardinaudNSaulnierIBhallaDRoquejoffreAet alEfficacy of Simple Home-Based Technologies Combined With a Monitoring Assistive Center in Decreasing Falls in a Frail Elderly Population (Results of the Esoppe Study). Arch Gerontol Geriatr (2012) 55(3):683–9. 10.1016/j.archger.2012.05.011
312.
UpatisingBHansonGJKimYLChaSSYihYTakahashiPY. Effects of Home Telemonitoring on Transitions Between Frailty States and Death for Older Adults: A Randomized Controlled Trial. Int J Gen Med (2013) 6:145–51. 10.2147/IJGM.S40576
313.
Read PaulLSalmonCSinnarajahASpiceR. Web-Based Videoconferencing for Rural Palliative Care Consultation With Elderly Patients at Home. Support Care Cancer (2019) 27(9):3321–30. 10.1007/s00520-018-4580-8
314.
ChangRLowHMcDonaldAParkGSongX. Web-Based Software Applications for Frailty Assessment in Older Adults: A Scoping Review of Current Status With Insights Into Future Development. BMC Geriatr (2021) 21(1):723. 10.1186/s12877-021-02660-6
315.
KimHHLeeSHChoNBYouHChoiTKimJ. User-Dependent Usability and Feasibility of a Swallowing Training Mhealth App for Older Adults: Mixed Methods Pilot Study. JMIR Mhealth Uhealth (2020) 8(7):e19585. 10.2196/19585
316.
ChanWMWooJHuiEHjelmNM. The Role of Telenursing in the Provision of Geriatric Outreach Services to Residential Homes in Hong Kong. J Telemed Telecare (2001) 7:38–46. 10.1258/1357633011936129
317.
RichardSLavandierKZiouecheYPelletierSVezainADucrocqX. Use of Telemedicine to Manage Severe Ischaemic Strokes in a Rural Area With an Elderly Population. Neurol Sci (2014) 35(5):683–5. 10.1007/s10072-013-1577-4
318.
GüttlerJGeorgoulasCLinnerTBockT. Towards a Future Robotic Home Environment: A Survey. Gerontology (2015) 61:268–80. 10.1159/000363698
319.
OhligsMStocklassaSRossaintRCzaplikMFollmannA. Employment of Telemedicine in Nursing Homes: Clinical Requirement Analysis, System Development and First Test Results. Clin Interv Aging (2020) 15:1427–37. 10.2147/CIA.S260098
320.
De LucaRBramantiADe ColaMCTrifilettiATomaselloPTorrisiMet alTele-Health-Care in the Elderly Living in Nursing Home: The First Sicilian Multimodal Approach. Aging Clin Exp Res (2016) 28(4):753–9. 10.1007/s40520-015-0463-8
321.
MatsumotoYKizakiHIkedaYNakamuraSKinaSNagaiTet alTelepharmacy in Mountainous Depopulated Areas of Japan: An Exploratory Interview Study of Patients’ Perspectives. Drug Discov Ther (2021) 15(6):337–40. 10.5582/ddt.2021.01102
322.
PerssonHLLythJLindL. The Health Diary Telemonitoring and Hospital-Based Home Care Improve Quality of Life Among Elderly Multimorbid Copd and Chronic Heart Failure Subjects. Int J COPD (2020) 15:527–41. 10.2147/COPD.S236192
323.
Goodman-CasanovaJMDura-PerezEGuzman-ParraJCuesta-VargasAMayoral-CleriesF. Telehealth Home Support During COVID-19 Confinement for Community-Dwelling Older Adults With Mild Cognitive Impairment or Mild Dementia: Survey Study. J Med Internet Res (2020) 22:e19434. 10.2196/19434
324.
HaoJFCuiHMHanJMBaiJXSongXCaoN. Tele-ICU: The Way Forward in Geriatric Care? In: Aging Clinical and Experimental Research. Springer International Publishing (2014). 26:575–82.
325.
ChooCCKuekJHLBurtonAAD. Smartphone Applications for Mindfulness Interventions With Suicidality in Asian Older Adults: A Literature Review. Int J Environ Res Public Health MDPI AG (2018) 15:2810. 10.3390/ijerph15122810
326.
SadekIMohktariM. Nonintrusive Remote Monitoring of Sleep in Home-Based Situation. J Med Syst (2018) 42(4):64. 10.1007/s10916-018-0917-6
327.
AanesenMLotheringtonATOlsenF. Smarter Elder Care? A Cost-Effectiveness Analysis of Implementing Technology in Elder Care. Health Inform J (2011) 17(3):161–72. 10.1177/1460458211409716
328.
BarnesNSeniorSWTomRResearcherMResearcherJNReevesA. Liverpool Telecare Pilot: Case Studies Mark Buckland Senior Researcher.
329.
BartelsSJDiMiliaPRFortunaKLNaslundJA. Integrated Care for Older Adults With Serious Mental Illness and Medical Comorbidity: Evidence-Based Models and Future Research Directions. Psychiatr Clin North America (2018) 41:153–64. 10.1016/j.psc.2017.10.012
330.
LiFHarmerPVoitJChouLS. Implementing an Online Virtual Falls Prevention Intervention During a Public Health Pandemic for Older Adults With Mild Cognitive Impairment: A Feasibility Trial. Clin Interv Aging (2021) 16:973–83. 10.2147/CIA.S306431
331.
de BatlleJMassipMVargiuENadalNFuentesABravoMOet alImplementing Mobile Health-Enabled Integrated Care for Complex Chronic Patients: Intervention Effectiveness and Cost-Effectiveness Study. JMIR Mhealth Uhealth (2021) 9(1):e22135. 10.2196/22135
332.
MatzOVillaLLecceCOlaciregui DagueKHaegerABollheimerLCet alImplementation of a Telemedicine Geriatric Co-Evaluation in the Emergency Department: A Prospective Pilot Study. Swiss Med Wkly (2021) 151:w20500. 10.4414/smw.2021.20500
333.
NoguésXSánchez-MartinezFCastellsXDíez-PérezASabatéRAPetitIet alHospital-at-Home Expands Hospital Capacity During COVID-19 Pandemic. J Am Med Dir Assoc (2021) 22(5):939–42. 10.1016/j.jamda.2021.01.077
334.
RubegniPNamiNCeveniniGPoggialiSHofmann-WellenhofRMassoneCet alGeriatric Teledermatology: Store-And-Forward vs. Face-To-Face Examination. J Eur Acad Dermatol Venereol (2011) 25(11):1334–9. 10.1111/j.1468-3083.2011.03986.x
335.
KikuchiATaniguchiTNakamotoKSeraFOhtaniTYamadaTet alFeasibility of Home-Based Cardiac Rehabilitation Using an Integrated Telerehabilitation Platform in Elderly Patients With Heart Failure: A Pilot Study. J Cardiol (2021) 78(1):66–71. 10.1016/j.jjcc.2021.01.010
336.
HoffmannWvan den BergNThyrianJRFissT. Frequency and Determinants of Potential Drug-Drug Interactions in an Elderly Population Receiving Regular Home Visits by GPs - Results of the Home Medication Review in the AGnES-Studies. Pharmacoepidemiol Drug Saf (2011) 20(12):1311–8. 10.1002/pds.2224
337.
JelcicNAgostiniMMeneghelloFBussèCPariseSGalanoAet alFeasibility and Efficacy of Cognitive Telerehabilitation in Early Alzheimer’s Disease: A Pilot Study. Clin Interv Aging (2014) 9:1605–11. 10.2147/CIA.S68145
338.
SkjæretNNawazAMoratTSchoeneDHelbostadJLVereijkenB. Exercise and Rehabilitation Delivered Through Exergames in Older Adults: An Integrative Review of Technologies, Safety and Efficacy. Int J Med Inform (2016) 85:1–16. 10.1016/j.ijmedinf.2015.10.008
339.
ChoiHKimJ. Effectiveness of Telemedicine: Videoconferencing for Low-Income Elderly With Hypertension. Telemed e-Health (2014) 20(12):1156–64. 10.1089/tmj.2014.0031
340.
ScherrenbergMZeymerUSchneiderSVan der VeldeAEWilhelmMVan’t HofAWJet alEU-CaRE Study: Could Exercise-Based Cardiac Telerehabilitation Also Be Cost-Effective in Elderly?Int J Cardiol (2021) 340:1–6. 10.1016/j.ijcard.2021.08.024
341.
PerssonHLLythJWiréhnABLindL. Elderly Patients With COPD Require More Health Care Than Elderly Heart Failure Patients Do in a Hospital-Based Home Care Setting. Int J COPD (2019) 14:1569–81. 10.2147/COPD.S207621
342.
KoceskaNKoceskiSZobelPBTrajkovikVGarciaN. A Telemedicine Robot System for Assisted and Independent Living. Sensors (Switzerland) (2019) 19(4):834. 10.3390/s19040834
343.
García‐villamilGNeira‐álvarezMHuertas‐hoyasERamón‐jiménezARodríguez‐sánchezC. A Pilot Study to Validate a Wearable Inertial Sensor for Gait Assessment in Older Adults With Falls. Sensors (2021) 21(13):4334. 10.3390/s21134334
344.
TegelerCBeyerAKHoppmannFLudwigVKesslerE-M. Current State of Research on Psychotherapy for Home-Living Vulnerable Older Adults With Depression. Z Gerontologie Geriatrie (2020) 53:721–7. 10.1007/s00391-020-01805-3
345.
KraftMVan Den BergNKraftKSchmekelSGärtnerSKrügerJet alDevelopment of a Telemedical Monitoring Concept for the Care of Malnourished Geriatric Home-Dwelling Patients: A Pilot Study. Maturitas (2012) 72(2):126–31. 10.1016/j.maturitas.2012.02.011
346.
AbbasMSommeDLe Bouquin JeannèsR. D-SORM: A Digital Solution for Remote Monitoring Based on the Attitude of Wearable Devices. Comput Methods Programs Biomed (2021) 208. 10.1016/j.cmpb.2021.106247
347.
LiCNeugroschlJZhuCWAloysiASchimmingCACaiDet alDesign Considerations for Mobile Health Applications Targeting Older Adults. J Alzheimer’s Dis (2021) 79(1):1–8. 10.3233/JAD-200485
348.
Dang ÃwzSMaFNeddNFlorez ÃwHÃwEARoos ÃwzBA. Care Coordination and Telemedicine Improves Glycaemic Control in Ethnically Diverse Veterans With Diabetes. J Telemed Telecare (2007) 13:263–7. 10.1258/135763307781458958
349.
GamitoPOliveiraJMoraisDCoelhoCSantosNAlvesCet alCognitive Stimulation of Elderly Individuals With Instrumental Virtual Reality-Based Activities of Daily Life: Pre-Post Treatment Study. Cyberpsychol Behav Soc Netw (2019) 22(1):69–75. 10.1089/cyber.2017.0679
350.
BrunettiNDDe GennaroLPellegrinoPLDellegrottaglieGAntonelliGDi BiaseM. Atrial Fibrillation With Symptoms Other Than Palpitations: Incremental Diagnostic Sensitivity With At-Home Tele-Cardiology Assessment for Emergency Medical Service. Eur J Prev Cardiol (2012) 19(3):306–13. 10.1177/1741826711406060
351.
GöranssonCWengströmYHälleberg-NymanMLangius-EklöfAZiegertKBlombergK. An App for Supporting Older People Receiving Home Care - Usage, Aspects of Health and Health Literacy: A Quasi-Experimental Study. BMC Med Inform Decis Mak (2020) 20(1):226. 10.1186/s12911-020-01246-3
352.
SugiharaTFujinamiTPhaalRIkawaY. A Technology Roadmap of Assistive Technologies for Dementia Care in Japan. Dementia (2015) 14(1):80–103. 10.1177/1471301213493798
353.
WongYKHuiEWooJ. A Community-Based Exercise Programme for Older With Knee Pain Using Telemedicine. J Telemed Telecare (2005) 11:310–5. 10.1258/1357633054893346
354.
MoriichiKFujiyaMRoTOtaTNishimiyaHKodamaMet alA Novel Telerehabilitation With an Educational Program for Caregivers Using Telelecture Is Feasible for Fall Prevention in Elderly People: A Case Series. Medicine (United States) (2022) 101(6):E27451. 10.1097/MD.0000000000027451
355.
FasilisTPatrikelisPSiatouniAAlexoudiAVeretziotiAZachouLet alA Pilot Study and Brief Overview of Rehabilitation via Virtual Environment in Patients Suffering From Dementia. Psychiatriki (2018) 29(1):42–51. 10.22365/jpsych.2018.291.42
356.
FallahMYasiniM. A Medication Reminder Mobile App: Does It Work for Different Age Ranges. Stud Health Technol Inform (2017) 235:68–72.
357.
AudiauSSchmollLBlancF. Déplacements et Hospitalisations Évités Grâce aux Téléconsultations pour les Patients Hébergés en Ehpad. Geriatr Psychol Neuropsychiatr Vieil (2021) 19(4):447–58. 10.1684/pnv.2021.0990
358.
AndrèsETalhaSBenyahiaAKellerOHajjamMMoukademAet alExpérimentation d’une Plateforme de Détection Automatisée des Situations à Risque de Décompensation Cardiaque (Plateforme E-Care) dans une Unité de Médecine Interne. Revue de Medecine Interne (2016) 37(9):587–93. 10.1016/j.revmed.2016.01.004
359.
BrondiRBannoFBendinelliSCastelliCMancinaAMarinoniMet alDrugs Don’t Work in Patients Who Don’t Take Them: Dr. Drin, the New ICT Paradigm for Chronic Therapies. Stud Health Technol Inform (2013) 191:100–4.
360.
SchofieldRSKlineSESchmalfussCMCarverHMArandaJMPaulyDFet alEarly Outcomes of a Care Coordination-Enhanced Telehome Care Program for Elderly Veterans With Chronic Heart Failure. Telemed J E Health (2005) 11:20–7. 10.1089/tmj.2005.11.20
361.
CorcoranHHuiEWooJ. The Acceptability of Telemedicine for Podiatric Intervention in a Residential Home for the Elderly.
362.
VestalLSmith-OlindeLHicksGHuttonTHartJJr. Efficacy of Language Assessment in Alzheimer’s Disease: Comparing In-Person Examination and Telemedicine. Clin Interv Aging (2006) 1(4):467–71. 10.2147/ciia.2006.1.4.467
363.
DukeC. The Frail Elderly Community– Based Case Management Project. Geriatr Nurs (Minneap) (2005) 26(2):122–7. 10.1016/j.gerinurse.2005.03.003
364.
Moon ChaeYHeon LeeJHee HoSJa KimHHong JunKUk WonJ. Patient Satisfaction With Telemedicine in Home Health Services for the Elderly. Int J Med Inform (2001) 61:167–73. 10.1016/s1386-5056(01)00139-3
365.
HuiEWooJHjelmMZhangYTTsuiHT. Clinical Section Telemedicine: A Pilot Study in Nursing Home Residents (2001). Available from: https://www.karger.com/journals/ger (Accessed July 5, 2023).
366.
DemirisGShigakiCLSchoppLH. An Evaluation Framework for a Rural Home-Based Telerehabilitation Network. J Med Syst (2005) 29:595–603. 10.1007/s10916-005-6127-z
367.
SchweickertPARutledgeCMCattell-GordonDCDivMWSolenskiNJJensenMEet alTelehealth Stroke Education for Rural Elderly Virginians.
368.
ChumblerNRMannWCWuSSchmidAKobbR. Veterans Affairs Health Services Research and Development/Rehabilitation Research and Development, Rehabilitation Outcomes Research Center (RORC), North Florida/South Georgia Veterans Health System, 6 Tech Care Coordination Program, North Florida/South Georgia Veterans Health System. Telemedicine Journal e-Health (2004) 10.
369.
CitoniBFigliuzziIPrestaVVolpeMTocciG. Home Blood Pressure and Telemedicine: A Modern Approach for Managing Hypertension During and After COVID-19 Pandemic. Vol. 29, High Blood Pressure and Cardiovascular Prevention. Adis (2022). 10.1007/s40292-021-00492-4
370.
RehmICMusićSCarlssonAScanlanFSilverMBharSS. Integrating Web-Based Applications Into Aged Care: Two Case Studies and Discussion. J Clin Psychol Med Settings (2016) 23(3):285–97. 10.1007/s10880-016-9457-8
371.
FatygaEDziȩgielewska-GȩsiakSWierzgońAStołtnyDMuc-WierzgońM (2020).The Coronavirus Disease 2019 Pandemic: Telemedicine in Elderly Patients With Type 2 DiabetesPolish Arch Intern Med Medycyna Praktyczna130. 452–4. 10.20452/pamw.15346
372.
PorathAIronyABorobickASNasserSMalachiAFundNet alMaccabi Proactive Telecare Center for Chronic Conditions - The Care of Frail Elderly Patients. Isr J Health Pol Res (2017) 6(1):68. 10.1186/s13584-017-0192-x
373.
BatsisJAPletcherSNStahlJE. Telemedicine and Primary Care Obesity Management in Rural Areas - Innovative Approach for Older Adults? Vol. BMC Geriatr (2017) 17:6. 10.1186/s12877-016-0396-x
374.
CardozoLSteinbergJ. Telemedicine for Recently Discharged Older Patients. Telemed e-Health (2010) 16:49–55. 10.1089/tmj.2009.0058
375.
LeeJKimJJeongSChoiHJinMKimS. A Health Recreation Program for U-Healthcare Clients: Effects on Mental Health. Telemed e-Health (2014) 20(10):930–5. 10.1089/tmj.2013.0323
376.
LattanzioFAbbatecolaAMBevilacquaRChiattiCCorsonelloARossiLet alAdvanced Technology Care Innovation for Older People in Italy: Necessity and Opportunity to Promote Health and Wellbeing. J Am Med Dir Assoc (2014) 15(7):457–66. 10.1016/j.jamda.2014.04.003
377.
Melander-WikmanAFältholmYGardG. Safety vs. Privacy: Elderly Persons’ Experiences of a Mobile Safety Alarm. Health Soc Care Community (2008) 16(4):337–46. 10.1111/j.1365-2524.2007.00743.x
378.
KonstantinidisEIBillisASMouzakidisCAZilidouVIAntoniouPEBamidisPD. Design, Implementation, and Wide Pilot Deployment of FitForAll: An Easy to Use Exergaming Platform Improving Physical Fitness and Life Quality of Senior Citizens. IEEE J Biomed Health Inform (2016) 20(1):189–200. 10.1109/JBHI.2014.2378814
379.
DangSDimmickSKelkarG, Evaluating the Evidence Base for the Use of Home Telehealth Remote Monitoring in Elderly With Heart Failure. Telemed J e-health15 (2009). p. 783–96. 10.1089/tmj.2009.0028
380.
ChenYHLinYHHungCSHuangCCYeihDFChuangPYet alClinical Outcome and Cost-Effectiveness of a Synchronous Telehealth Service for Seniors and Nonseniors With Cardiovascular Diseases: Quasi-Experimental Study. J Med Internet Res (2013) 15(4):e87. 10.2196/jmir.2091
381.
MarescaGDe ColaMCCaliriSDe LucaRManuliAScarcellaIet alMoving Towards Novel Multidisciplinary Approaches for Improving Elderly Quality of Life: The Emerging Role of Telemedicine in Sicily. J Telemed Telecare (2019) 25(5):318–24. 10.1177/1357633X17753057
382.
CarolanKGrabowskiDCMehrotraAHatfieldLA. Use of Telemedicine for Emergency Triage in an Independent Senior Living Community: Mixed Methods Study. J Med Internet Res (2020) 22(12):e23014. 10.2196/23014
383.
StutzelMCFilippoMPSztajnbergADa CostaRMEMBritesADSDa MottaLBet alMulti-Part Quality Evaluation of a Customized Mobile Application for Monitoring Elderly Patients With Functional Loss and Helping Caregivers. BMC Med Inform Decis Mak (2019) 19(1):140. 10.1186/s12911-019-0839-3
384.
WillardSCremersGManYPVan RossumESpreeuwenbergMDe WitteL. Development and Testing of an Online Community Care Platform for Frail Older Adults in the Netherlands: A User-Centred Design. BMC Geriatr (2018) 18(1):87. 10.1186/s12877-018-0774-7
385.
TorpSHansonEHaugeSUlsteinIMagnussonL. A Pilot Study of How Information and Communication Technology May Contribute to Health Promotion Among Elderly Spousal Carers in Norway. Health Soc Care Community (2008) 16(1):75–85. 10.1111/j.1365-2524.2007.00725.x
386.
MarinelloRBrunettiELuppiCBiancaDTibaldiVIsaiaGet alTelemedicine-Assisted Care of an Older Patient With COVID-19 and Dementia: Bridging the Gap Between Hospital and Home. Aging Clin Exp Res (2021) 33(6):1753–6. 10.1007/s40520-021-01875-2
387.
ShahMNGillespieSMWoodNWassermanEBNelsonDLDozierAet alHigh-intensity Telemedicine-Enhanced Acute Care for Older Adults: An Innovative Healthcare Delivery Model. J Am Geriatr Soc (2013) 61(11):2000–7. 10.1111/jgs.12523
388.
GillespieSMShahMNWassermanEBWoodNEWangHNoyesKet alReducing Emergency Department Utilization through Engagement in Telemedicine by Senior Living Communities. Engagement Telemed by Senior Living Communities. Telemed e-Health (2016) 22(6):489–96. 10.1089/tmj.2015.0152
389.
GasparAGMLapãoLV. A Digital Health Service for Elderly People With Balance Disorders and Risk of Falling: A Design Science Approach. Int J Environ Res Public Health (2022) 19(3):1855. 10.3390/ijerph19031855
390.
HaimiMGesser-EdelsburgA. Application and Implementation of Telehealth Services Designed for the Elderly Population During the COVID-19 Pandemic: A Systematic Review. Health Inform J (2022) 28(1):14604582221075561. 10.1177/14604582221075561
391.
ShahMNWassermanEBWangHGillespieSMNoyesKWoodNEet alHigh-Intensity Telemedicine Decreases Emergency Department Use by Senior Living Community Residents. Telemed e-Health (2016) 22(3):251–8. 10.1089/tmj.2015.0103
392.
SavolainenLHansonEMagnussonLGustavssonT. An Internet-Based Videoconferencing System for Supporting Frail Elderly People and Their Carers. J Telemed Telecare (2008) 14(2):79–82. 10.1258/jtt.2007.070601
393.
NgaruiyaCOtiSVan De VijverSKyobutungiCFreeC. Target Women: Equity in Access to mHealth Technology in a Non-Communicable Disease Care Intervention in Kenya. PLoS One (2019) 14(9):e0220834. 10.1371/journal.pone.0220834
394.
GillespieSMWassermanEBWoodNEWangHDozierANelsonDet alHigh-Intensity Telemedicine Reduces Emergency Department Use by Older Adults With Dementia in Senior Living Communities. J Am Med Dir Assoc (2019) 20(8):942–6. 10.1016/j.jamda.2019.03.024
395.
SheeranTRabinowitzTLottermanJReillyCFBrownSDonehowerPet alFeasibility and Impact of Telemonitor-Based Depression Care Management for Geriatric Homecare Patients. Telemed e-Health. (2011) 17(8):620–6. 10.1089/tmj.2011.0011
396.
Ramos-RosRMateosRLojoDConnDKPattersonT. Telepsychogeriatrics: A New Horizon in the Care of Mental Health Problems in the Elderly. Int Psychogeriatrics (2012) 24:1708–24. 10.1017/S1041610212000981
397.
MarschollekMMixSWolfKHEffertzBHauxRSteinhagen-ThiessenE. ICT-Based Health Information Services for Elderly People: Past Experiences, Current Trends, and Future Strategies. Med Inform Internet Med (2007) 32(4):251–61. 10.1080/14639230701692736
398.
De ColaMCDe LucaRBramantiABertèFBramantiPCalabròRS. Tele-Health Services for the Elderly: A Novel Southern Italy Family Needs-Oriented Model. J Telemed Telecare (2016) 22(6):356–62. 10.1177/1357633X15604290
399.
AdamiIFoukarakisMNtoaSPartarakisNStefanakisNKoutrasGet alMonitoring Health Parameters of Elders to Support Independent Living and Improve Their Quality of Life. Sensors (Switzerland) (2021) 21(2):517–36. 10.3390/s21020517
400.
ZulfiqarAAHajjamAAndrèsE. Focus on the Different Projects of Telemedicine Centered on the Elderly in France. Curr Aging Sci (2019) 11(4):202–15. 10.2174/1874609812666190304115426
401.
MulassoABrustioPRRainoldiAZiaGFelettiLN’DjaAet alA Comparison Between an ICT Tool and a Traditional Physical Measure for Frailty Evaluation in Older Adults. BMC Geriatr (2019) 19(1):88. 10.1186/s12877-019-1089-z
402.
SmithACGrayLC. Telemedicine Across the Ages. Med J Aust (2009) 190(1):15–9. 10.5694/j.1326-5377.2009.tb02255.x
403.
ScalviniSBernocchiPZanelliECominiLVitaccaM,Maugeri Centre for Telehealth and Telecare MCTT. Maugeri Centre for Telehealth and Telecare: A Real-Life Integrated Experience in Chronic Patients. J Telemed Telecare (2018) 24(7):500–7. 10.1177/1357633X17710827
404.
GentryMTLapidMIRummansTA. Geriatric Telepsychiatry: Systematic Review and Policy Considerations. Am J Geriatr Psychiatry (2019) 27(2):109–27. 10.1016/j.jagp.2018.10.009
405.
Elie-LefebvreCSchusterJPLimosinF. Télépsychiatrie: Quelle Place dans les Soins des Sujets Âgés. Geriatr Psychol Neuropsychiatr Vieil (2016) 14(3):325–31. 10.1684/pnv.2016.0625
406.
KarunanithiM. Monitoring Technology for the Elderly Patient. Expert Rev Med Devices (2007) 4:267–77. 10.1586/17434440.4.2.267
407.
LythJLindLPerssonHLWiréhnAB. Can a Telemonitoring System Lead to Decreased Hospitalization in Elderly Patients?J Telemed Telecare (2021) 27(1):46–53. 10.1177/1357633X19858178
408.
TseMMYChoiKCYLeungRSW. E-Health for Older People: The Use of Technology in Health Promotion. Cyberpsychology Behav (2008) 11(4):475–9. 10.1089/cpb.2007.0151
409.
BaxterKEKocharSWilliamsCBlackmanCHimmelvoJ. Development of a Palliative Telehealth Pilot to Meet the Needs of the Nursing Home Population. J Hosp Palliat Nurs (2021) 23(5):478–83. 10.1097/NJH.0000000000000784
410.
KhosraviPGhapanchiAH. Investigating the Effectiveness of Technologies Applied to Assist Seniors: A Systematic Literature Review. Int J Med Inform (2015) 85(1):17–26. 10.1016/j.ijmedinf.2015.05.014
411.
Van DenBNSchumannMKraftKHoffmannW. Telemedicine and Telecare for Older Patients - A Systematic Review. Maturitas (2012) 73:94–114. 10.1016/j.maturitas.2012.06.010
412.
KimHJungYIKimGSChoiHParkYH. Effectiveness of a Technology-Enhanced Integrated Care Model for Frail Older People: A Stepped-Wedge Cluster Randomized Trial in Nursing Homes. Gerontologist (2021) 61(3):460–9. 10.1093/geront/gnaa090
413.
WassSVimarlundV. The Role of ICT in Home Care. In: Studies in Health Technology and Informatics. IOS Press BV (2017). p. 153–8. 10.3233/978-1-61499-794-8-153
414.
MarcelinoILazaRDominguesPGómez-MeireSFdez-RiverolaFPereiraA. Active and Assisted Living Ecosystem for the Elderly. Sensors (Switzerland) (2018) 18(4):1246. 10.3390/s18041246
415.
LinnNGoetzingerCRegnauxJPSchmitzSDessenneCFagherazziGet alDigital Health Interventions Among People Living With Frailty: A Scoping Review. J Am Med Directors Assoc (2021) 22:1802–12.e21. 10.1016/j.jamda.2021.04.012
416.
Calvillo‐arbizuJNaranjo‐hernándezDBarbarov‐rostánGTalaminos‐barrosoARoa‐romeroLMReina‐tosinaJ. A Sensor‐based Mhealth Platform for Remote Monitoring and Intervention of Frailty Patients at Home. Int J Environ Res Public Health (2021) 18(21):11730. 10.3390/ijerph182111730
417.
BonVGhemameMFantouPPhilliponnetAMouriauxF. Feedback on Ophthalmologic Telemedicine in a Nursing Home. J Fr Ophtalmol (2020) 43(9):e293–7. 10.1016/j.jfo.2020.09.002
418.
JaanaMParéG. Comparison of Mobile Health Technology Use for Self-Tracking Between Older Adults and the General Adult Population in Canada: Cross-Sectional Survey. JMIR Mhealth Uhealth (2020) 8(11):e24718. 10.2196/24718
419.
LeeSYuS. Effectiveness of Information and Communication Technology (Ict) Interventions in Elderly’s Sleep Disturbances: A Systematic Review and Meta-Analysis. Sensors (2021) 21:6003. 10.3390/s21186003
420.
GlomsåsHSKnutsenIRFossumMHalvorsenK. They Just Came With the Medication Dispenser-a Qualitative Study of Elderly Service Users’ Involvement and Welfare Technology in Public Home Care Services. BMC Health Serv Res (2021) 21(1):245. 10.1186/s12913-021-06243-4
421.
KruseCSMileskiMMorenoJ. Mobile Health Solutions for the Aging Population: A Systematic Narrative Analysis. J Telemed Telecare (2017) 23(4):439–51. 10.1177/1357633X16649790
422.
LapãoLVPeyroteoMMaiaMSeixasJGregórioJMira da SilvaMet alImplementation of Digital Monitoring Services During the COVID-19 Pandemic for Patients With Chronic Diseases: Design Science Approach. J Med Internet Res (2021) 23(8):e24181. 10.2196/24181
423.
LangCRoesslerMSchmittJBergmannAHolthoff-DettoV. Health-Related Quality of Life in Elderly, Multimorbid Individuals With and Without Depression And/or Mild Cognitive Impairment Using a Telemonitoring Application. Qual Life Res (2021) 30(10):2829–41. 10.1007/s11136-021-02848-8
424.
JoosenPPietteDBuekersJTaelmanJBerckmansDDe BoeverP. A Smartphone-Based Solution to Monitor Daily Physical Activity in a Care Home. J Telemed Telecare (2019) 25(10):611–22. 10.1177/1357633X18790170
425.
AndrèsEZulfiqarAATalhaSHajjamMHajjamJErvéSet alTélémédecine et Insuffisance Cardiaque du Sujet âgé, 16. Geriatrie et Psychologie Neuropsychiatrie du Vieillissement (2018). p. 341–8. NLM (Medline). 10.1089/dia.2009.0102
426.
LiuLStrouliaENikolaidisIMiguel-CruzARios RinconA. Smart Homes and Home Health Monitoring Technologies for Older Adults: A Systematic Review. Int J Med Inform (2016) 91:44–59. 10.1016/j.ijmedinf.2016.04.007
427.
MajumderSAghayiENoferestiMMemarzadeh-TehranHMondalTPangZet alSmart Homes for Elderly Healthcare—Recent Advances and Research Challenges. Sensors (Switzerland) (2017) 17:2496. 10.3390/s17112496
428.
AlsaqerM. Aging and Technology: Understanding the Issues and Creating a Base for Technology Designers. J Med Eng Technol (2021) 45(4):258–83. 10.1080/03091902.2021.1891313
429.
ChelongarKAjamiS. Using Active Information and Communication Technology for Elderly Homecare Services: A Scoping Review. Home Health Care Serv Q (2021) 40:93–104. 10.1080/01621424.2020.1826381
430.
GokalpHDe FolterJVermaVFursseJJonesRClarkeM. Integrated Telehealth and Telecare for Monitoring Frail Elderly With Chronic Disease. Telemed J E Health (2018) 24:940–57. 10.1089/tmj.2017.0322
431.
SekhonHSekhonKLaunayCAfililoMInnocenteNVahiaIet alTelemedicine and the Rural Dementia Population: A Systematic Review. Maturitas (2021) 143:105–14. 10.1016/j.maturitas.2020.09.001
432.
BrooksSEBurrussSKMukherjeeK. Suicide in the Elderly: A Multidisciplinary Approach to Prevention. Clin Geriatr Med (2019) 35:133–45. 10.1016/j.cger.2018.08.012
433.
ChenYRRSchulzPJ. The Effect of Information Communication Technology Interventions on Reducing Social Isolation in the Elderly: A Systematic Review. J Med Internet Res (2016) 18(1):e18. 10.2196/jmir.4596
434.
WHO Global Observatory for eHealth. Global Diffusion of eHealth: Making Universal Health Coverage Achievable. Rep third Glob Surv eHealth (2016).
435.
World Bank. Data Blog. New World Bank Country Classifications by Income Level: 2022-2023 (2022). Available from: https://blogs.worldbank.org/en/opendata/new-world-bank-country-classifications-income-level-2022-2023 (Accessed May 9, 2024).
436.
National Institutes of Health. Aging in Place: Growing Older at Home. Natl Inst Aging (2023). Available from: https://www.nia.nih.gov/health/aging-place/aging-place-growing-older-home (Accessed July 4, 2024).
437.
RatnayakeMLukasSBrathwaiteSNeaveJHenryH. Aging in Place: Are We Prepared?Dela J Public Health (2022) 8(3):28–31. 10.32481/djph.2022.08.007
438.
MaceRAMattosMKVranceanuAM. Older Adults Can Use Technology: Why Healthcare Professionals Must Overcome Ageism in Digital Health. Transl Behav Med (2022) 12(12):1102–5. 10.1093/tbm/ibac070
439.
de Siqueira SilvaÍde AraújoAJLopesRHSilvaCRDVXavierPBde FigueirêdoRCet alDigital Home Care Interventions and Quality of Primary Care for Older Adults: A Scoping Review. BMC Geriatr (2024) 24(1):507–19. 10.1186/s12877-024-05120-z
440.
TsaiYIPBehJGandertonCPranataA. Digital Interventions for Healthy Ageing and Cognitive Health in Older Adults: A Systematic Review of Mixed Method Studies and Meta-Analysis. BMC Geriatr (2024) 24(1):217. 10.1186/s12877-023-04617-3
441.
AlruwailiMMShabanMElsayed RamadanOM. Digital Health Interventions for Promoting Healthy Aging: A Systematic Review of Adoption Patterns, Efficacy, and User Experience. Sustainability (Switzerland) (2023) 15(23):16503. 10.3390/su152316503
442.
LeeSHChonYKimYY. Comparative Analysis of Long-Term Care in OECD Countries: Focusing on Long-Term Care Financing Type. Healthcare (2023) 11(2):206. 10.3390/healthcare11020206
443.
Mounier-JackSMayhewSHMaysN. Integrated Care: Learning Between High-Income, and Low- and Middle-Income Country Health Systems. Health Policy Plan (2017) 32(Suppl. 4):iv6–iv12. 10.1093/heapol/czx039
444.
FangFYangX. Socioeconomic Status, Cultural Values, and Elderly Care: An Examination of Elderly Care Preference in OECD Countries. Aging Health Res (2023) 3(3):100153. 10.1016/j.ahr.2023.100153
445.
HuenchuanS. Envejecimiento, Personas Mayores y Agenda 2030 para el Desarrollo Sostenible. Perspectiva regional y de Derechos Humanos. Desarrollo Social. Santiago: Naciones Unidas (2018). Available from: www.cepal.org/es/suscripciones (Accessed July 8, 2024).
446.
MlinarićAHorvatMVšS. Dealing With the Positive Publication Bias: Why You Should Really Publish Your Negative Results. Biochem Med (Zagreb) (2017) 27(3):30201. 10.11613/BM.2017.030201
Appendix: Search Strategy
Database: PubMed (The strategy created for PubMed was modified to suit the requirements of the other databases.)
Date: 06 April 2022.
Key words: elderly OR frail OR senior OR frail elderly.
AND
digital health OR e-Health OR telemedicine OR telehealth OR digital therapeutics OR virtual medicine OR information and communication technology OR ICT OR silver economy OR mhealth OR mobile application.
Filters: humans and languages (English, French, Portuguese, Spanish)
Strategy:
(“elderly”[Title/Abstract] OR “frail”[Title/Abstract] OR “senior”[Title/Abstract] OR “frail elderly”[Title/Abstract]) AND (“digital health”[Title/Abstract] OR “e-Health”[Title/Abstract] OR “telemedicine”[Title/Abstract] OR “telehealth”[Title/Abstract] OR “digital therapeutics”[Title/Abstract] OR “virtual medicine”[Title/Abstract] OR “ICT”[Title/Abstract] OR “Information and Communication Technology” OR “silver economy”[Title/Abstract] OR “mhealth”[Title/Abstract] OR “mobile application”[Title/Abstract])
Summary
Keywords
digital health, elderly, caregiver, reviews, telemedicine
Citation
Hirmas-Adauy M, Castillo-Laborde C, Awad C, Jasmen A, Mattoli M, Molina X, Olea A, Matute I, Soto F, Rubilar P, Urrejola O, Alfaro T, Abusleme Lama MT and Esnouf S (2024) Navigating Through Innovation in Elderly’s Health: A Scoping Review of Digital Health Interventions. Public Health Rev 45:1607756. doi: 10.3389/phrs.2024.1607756
Received
12 July 2024
Accepted
26 November 2024
Published
19 December 2024
Corrected
17 February 2026
Volume
45 - 2024
Edited by
Milena Maule, University of Turin, Italy
Reviewed by
Maria Vittoria Bulgheroni, Ab.Acus, Italy
Maria Bujnowska-Fedak, Wroclaw Medical University, Poland
Updates
Copyright
© 2024 Hirmas-Adauy, Castillo-Laborde, Awad, Jasmen, Mattoli, Molina, Olea, Matute, Soto, Rubilar, Urrejola, Alfaro, Abusleme Lama and Esnouf.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms. PHR is edited by the Swiss School of Public Health (SSPH+) in a partnership with the Association of Schools of Public Health of the European Region (ASPHER)+
*Correspondence: Macarena Hirmas-Adauy, mhirmas@udd.cl
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.