Abstract
Objectives: The aim was to systematically review and synthesise international evidence on changes in health risk behaviours by immigrants’ duration of residence.
Methods: We searched literature databases for peer-reviewed quantitative studies published from 2000 to 2019, examining alcohol, drug and tobacco use; physical inactivity; and dietary habits by duration of residence.
Results: Narrative synthesis indicated that immigrants tend to adopt health risk behaviours with longer residence in North America, with larger variation in effect sizes and directionality in other contexts. Random-effects meta-analyses examining the pooled effect across all receiving countries and immigrant groups showed lower odds of smoking (OR 0.54, 0.46–0.63, I2 = 68.7%) and alcohol use (OR 0.61, 0.47–0.75, I2 = 93.5%) and higher odds of physical inactivity (OR 1.71, 1.40–2.02, I2 = 99.1%) among immigrants than natives, but did not provide support for a universal trend by duration of residence.
Conclusion: Findings suggest that duration of residence could serve as an effective instrument to monitor immigrants’ health changes. However, differences in receiving country contexts and immigrant populations’ composition seem to be important to predict the level and direction of behavioural change.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/, PROSPERO CRD42018108881.
Introduction
Health risk behaviours, including alcohol, drug and tobacco use, physical inactivity and poor dietary habits are responsible for a myriad of adverse outcomes [1, 2]. Due to the uneven distribution of these behaviours across social groups, they also contribute to the maintenance of health inequalities [3–5]. The adoption of health risk behaviours has commonly been hypothesised to explain why immigrants frequently experience health deterioration with increasing time in their receiving country, often to converge with native risks [6].
Although the literature on immigrants’ health risk behaviours by duration of residence is extensive, there is a general lack of synthesised evidence. To date, the only systematic reviews that have examined changes in immigrants’ health risk behaviours in the receiving context—albeit for specific health risk behaviours, immigrant populations and receiving country contexts [7–16]—have exclusively focused on the role of acculturation (the process by which immigrants assimilate and gradually adopt norms, values and characteristics of the majority population in the receiving country). Besides applying an unequivocal theoretical approximation to interpreting findings (a cultural lens), this approach has favoured the use of specific instruments (acculturation measures) and reduced the use of others within the same domain (including for duration of residence). Furthermore, this practice has limited the synthesis of evidence beyond the acculturation framework, which in turn limits the capacity to propose and discuss alternative models, such as the role of social inequalities in health behaviours. Thus, despite the availability of an extensive literature on changes in immigrants’ health risk behaviours by duration of residence, to our knowledge, there have been no previous systematic evaluations.
This systematic review aimed to comprehensively synthesise international evidence on changes in health risk behaviours, including alcohol, drug and tobacco use, physical activity and diet, by immigrants’ duration of residence, with immigrant and native reference populations. Through meta-analysis, we additionally aimed to investigate whether universal patterns of health behavioural changes exist across heterogeneous immigrant populations and country contexts.
Methods
Search Strategy and Selection Criteria
This systematic review and meta-analysis was conducted in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [17]. PubMed/MEDLINE, Web of Science, and ProQuest databases were systematically searched for peer-reviewed English-language articles published online between January 1st, 2000 and December 31st, 2019. Search strings were developed over multiple iterations (Supplementary Table S1).
Studies were included if they examined international immigrants aged 18–64 years at the time of assessment (including individuals who migrated as children), by duration of residence (with a reference group in the receiving country), with a health risk behaviour outcome, including alcohol, drug (i.e., illicit substances) and tobacco (i.e., cigarettes, smokeless tobacco products) use; physical inactivity; and poor dietary habits. We did not distinguish by countries or regions of origin and destination; reasons for migration; or native or immigrant reference groups. Studies on internal migrants; temporary migrants; circular and return migrants; and minority groups indistinguishable by their foreign-birth status were excluded, as were studies focusing on transitional life periods, i.e., adolescence or retirement. Only studies utilising quantitative or mixed methods with observational data were considered. Qualitative studies and grey literature were excluded.
Using the Covidence systematic review online management tool, two authors independently screened and selected papers by title and abstract. Full-length articles were then reviewed by four authors in review pairs.
The study protocol was registered in PROSPERO (no. CRD42018108881), then peer-reviewed and published with open access, detailing the search strategy and selection process [18].
Data Analysis
Relevant data from the selected studies was extracted in review pairs using a piloted and standardised data extraction form. Extracted data included sample characteristics (e.g., sample size, age range, sex proportion, socioeconomic information) and details about exposure and outcome measures, analytical approaches, effect measures and controls. Each study was independently and systematically assessed for quality by two authors, using modified versions of the Newcastle-Ottawa Scale for cross-sectional studies (based on original case-control version) and cohort studies [19], and checked by a third author for completeness and accuracy.
We conducted a narrative synthesis to explore and summarise patterns of health risk behaviours by duration of residence. In the narrative synthesis, particular attention was given to studies with native reference groups to explore patterns of convergence and divergence with behaviours of native-born populations. We examined findings for different health risk behaviours separately and, given sufficient data from the included studies, by sex, immigrant region of origin and study (i.e., receiving) region. The narrative synthesis followed the Synthesis Without Meta-analysis [20] and PRISMA guidelines.
Thereafter, random-effects meta-analyses [21] were performed using the metan command in Stata version 13 [22]. Results were presented in Forest plots to visualise changes in health risk behaviours by immigrants’ duration of residence, relative to native-born populations. Summary estimates were used to broadly compare health risk behaviours between immigrants and natives, and I2 statistics to indicate the proportion of variance attributable to study heterogeneity (i.e., due to differences in duration of residence measures) [23]. By treating the native-born populations as a homogeneous reference group, these analyses permitted us to evaluate whether there was a universal pattern of health behavioural changes by duration of residence comparable to other empirical generalisations, such as the healthy immigrant paradox [24]. Summary estimates are presented as Odds Ratios (ORs) with 95% Confidence Intervals (CI) and plotted as log ORs to facilitate visualisation. Unadjusted Risk Ratios were transformed into ORs when enough information was provided in the studies. Separate analyses were conducted for unadjusted and adjusted estimates. When several model specifications were available, we extracted information from minimally-adjusted models, i.e., adjusting for sex, age and socioeconomic information, to avoid over-adjustment.
Subgroup meta-analyses were conducted by country or region of birth, receiving country and sex, when data allowed. Subgroup analyses by type of alcohol use (i.e., regular vs. binge drinking) and physical inactivity (i.e., leisure- vs. non-leisure-time) were not possible due to insufficient data for statistical pooling. Finally, we conducted subgroup analyses by different categorisations of duration of residence to assess the sensitivity of the results. In reporting meta-analysis results, Meta-analysis of Observational Studies in Epidemiology (MOOSE) Group recommendations were followed [25].
Any conflicts in the review, extraction or quality rating processes were resolved through discussion with other review team members. Study authors were contacted if clarification was needed.
Results
The database searches yielded 10,409 records (Figure 1), of which 4,019 were removed as duplicates, 440 by publication type and 151 by language. Non-relevant studies were excluded by title (n = 2,621), abstract (n = 2,199) and full text (n = 856), with a final count of 123 included studies (Supplementary Table S2) [26–148].
FIGURE 1
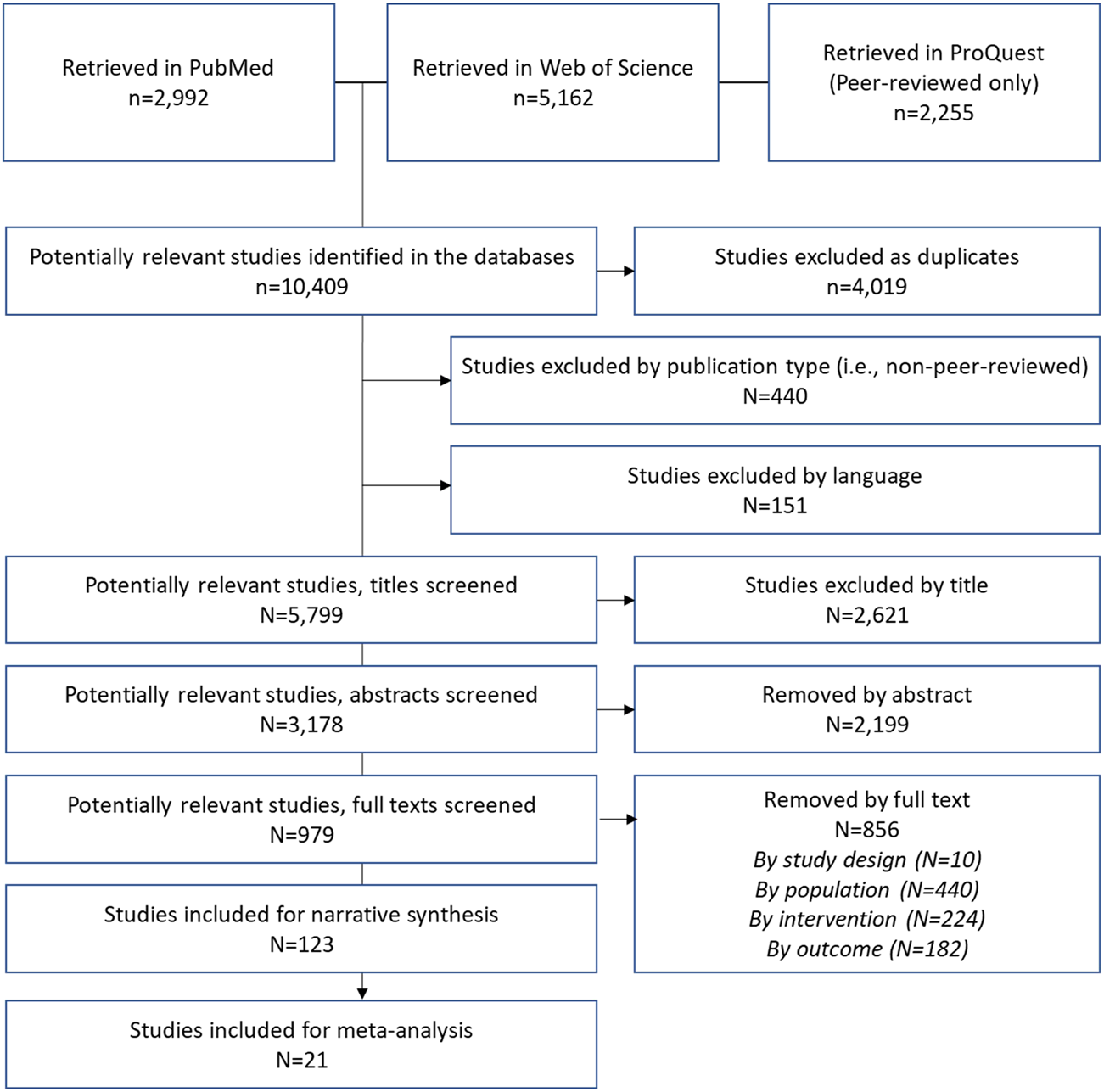
Selection process (Sweden, 2022).
Studies examined tobacco (n = 58), alcohol (n = 31) and drug use (n = 10); substance use diagnoses or dependence (n = 11); physical inactivity (n = 49); and diet (n = 17). Most studies were cross-sectional (n = 117), with a few longitudinal studies (n = 6), based on large-scale or study-specific surveys and interviews from 1988 to 2015. More than half of the studies (56%) were rated 75% or better (Supplementary Tables S3, S4). Included studies were from North America, including the USA (n = 81) and Canada (n = 12); Europe, including Finland (n = 1), France (n = 2), Germany (n = 7), Ireland (n = 1), the Netherlands (n = 6), Norway (n = 1), Spain (n = 4), Sweden (n = 1) and the UK (n = 7); as well as Australia (n = 6) and Israel (n = 1). Immigrant origins were commonly unspecified. Specified regions of origin can be broadly summarised as Asian (n = 41), African/Afro-Caribbean (n = 19), Latino/Hispanic (n = 31), European (n = 5) and Middle Eastern (n = 8). Some studies presented sex-stratified (n = 35) or sex-specific findings for men (n = 13) and women (n = 12). See Supplementary Table S5 for index of study characteristics.
Findings from the narrative synthesis of the 123 included studies are described below, with detailed tables provided as Supplementary Tables S6–S20.
Tobacco Use
With one exception [117], all included tobacco-related studies referred to smoking. In North America, most studies revealed increased risks of smoking with longer residence among general immigrant populations [67, 89, 96, 102, 109, 128, 146], as well as Latino/Hispanic [71, 119] and African/Afro-Caribbean [44, 127] immigrants specifically. Findings among Asian immigrants ranged from increasing [100, 103, 117] to decreasing [34, 72, 78, 115] risks, or no trend at all [50, 90, 133]. Asian immigrant men in particular had decreased risks of smoking with longer residence [31, 65, 70, 81, 106, 123], while findings for Latino/Hispanic men were less conclusive [39, 106, 123, 124]. Increased risks of smoking with longer residence appeared for immigrant women of unspecified origin [32, 52, 89, 100, 102, 144], and of African [74], Asian [31, 53, 106, 117, 123, 145] and Latino/Hispanic origin [106, 123].
For immigrants residing in Europe, increased risks of smoking were apparent with longer residence, regardless of country of origin or destination [40, 45, 82, 131]. Findings were mixed among men, with African men showing increased risks [85, 125], Eastern European men no change or decreased risks [125] and Middle Eastern men varied risks of smoking by longer residence [120–122, 125]. Immigrant women largely had increased risks of smoking with longer residence [75, 85, 121, 122, 125]. Studies from Australia were generally inconclusive with regards to directionality of risks [43, 76, 80, 137].
Among North American studies with native-born references, risks generally converged to native levels [32, 44, 102, 119, 123, 128], with some evidence of divergence [34, 39, 60, 123] or unclear patterns relative to natives [39, 93, 109, 114]. European evidence on convergence was more inconclusive, varying by country of origin and destination [64, 85, 131].
Meta-analyses showed lower odds of smoking among immigrants compared to natives regardless of model specification (unadjusted OR 0.54, 95% CI 0.46–0.63, I2 = 68.7%; adjusted OR 0.44, 95% CI 0.39–0.50, I2 = 97.0%; Figure 2), but with no clear patterns of change by duration of residence.
FIGURE 2
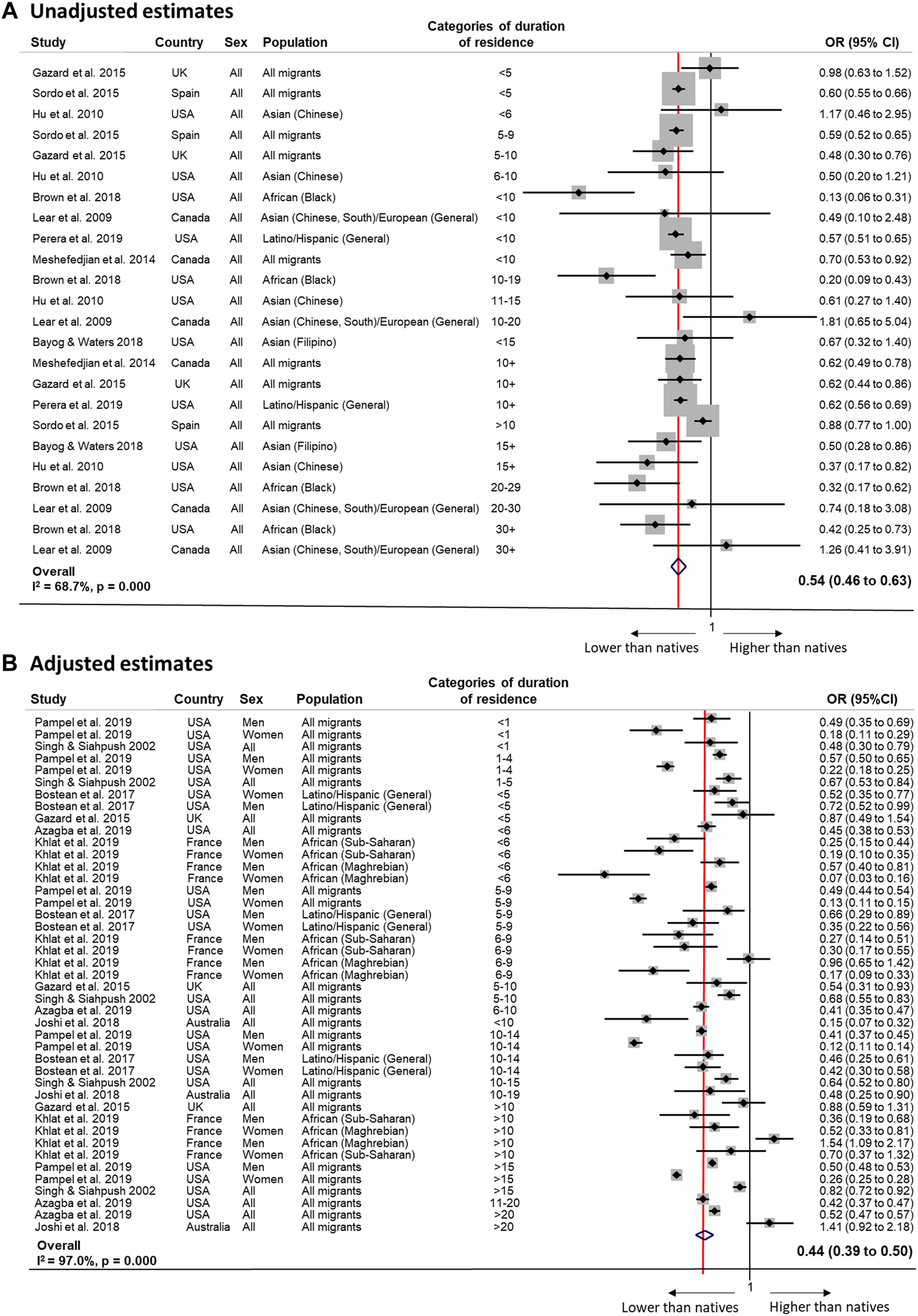
Random-effects meta-analysis of unadjusted (Panel (A)) and adjusted (Panel (B)) estimates of the association between tobacco use and duration of residence among migrants compared to the native population (Sweden, 2022). Panel (A): <5 years 0.73 (0.38 to 1.07), I2 = 62.6%, p 0.102 (2 estimates); ≥5 years 0.52 (0.43 to 0.62); I2 = 81.7%, p 0.000 (21 estimates); <10 years 0.54 (0.43 to 0.66); I2 = 83.4%, p 0.000 (10 estimates); ≥10 years 0.54 (0.42 to 0.67); I2 = 77.6%, p 0.000 (14 estimates); <15 years 0.57 (0.48 to 0.66); I2 = 83.8%, p 0.000 (18 estimates); ≥15 years 0.40 (0.27 to 0.53); I2 = 0%, p 0.829 (6 estimates). By host country: USA <5 years N/a; ≥5 years 0.42 (0.29 to 0.56); I2 = 85.5%, p 0.000 (11 estimates); <10 years 0.43 (0.01 to 0.85), I2 = 94.8%, p 0.000 (3 estimates); ≥10 years 0.44 (0.28 to 0.60); I2 = 76.0%, p 0.000 (8 estimates); <15 years 0.45 (0.27 to 0.63); I2 = 89.3%, p 0.000 (8 estimates); ≥15 years 0.40 (0.27 to 0.53); I2 = 0.0%, p 0.802 (4 estimates). Panel (B): <5 years 0.49 (0.34 to 0.65), I2 = 93.7%, p 0.000 (9 estimates); ≥5 years 0.46 (0.39 to 0.54); I2 = 98.2%, p 0.000 (26 estimates); <10 years 0.38 (0.30 to 0.47); I2 = 95.1%, p 0.000 (23 estimates); ≥10 years 0.52 (0.42 to 0.62); I2 = 98.5%, p 0.000 (17 estimates); <15 years 0.42 (0.36 to 0.49); I2 = 95.9%, p 0.000 (37 estimates); ≥15 years 0.54 (0.39 to 0.69); I2 = 98.8%, p 0.000 (6 estimates). By gender: Men <5 years 0.57 (0.49 to 0.66), I2 = 17.2%, p 0.299 (3 estimates); ≥5 years 0.48 (0.41 to 0.55); I2 = 81.1%, p 0.000 (9 estimates); <10 years 0.51 (0.41 to 0.60); I2 = 74.4%, p 0.000 (9 estimates); ≥10 years 0.48 (0.38 to 0.58); I2 = 86.6%, p 0.000 (5 estimates); <15 years N/a (1 estimates); ≥15 years 0.50 (0.42 to 0.58); I2 = 79.3%, p 0.000 (13 estimates). Women <5 years 0.26 (0.15 to 0.37), I2 = 76.7%, p 0.014 (3 estimates); ≥5 years 0.25 (0.18 to 0.33); I2 = 96.4%, p 0.000 (9 estimates); <10 years 0.20 (0.15 to 0.26); I2 = 82.4%, p 0.000 (9 estimates); ≥10 years 0.30 (0.19 to 0.42); I2 = 97.9%, p 0.000 (5 estimates); <15 years 0.21 (0.17 to 0.26); I2 = 85.9%, p 0.000 (13 estimates; ≥15 years N/a (1 estimates). By origin: “All migrants” <5 years 0.47 (0.27 to 0.63), I2 = 94.5%, p 0.000 (7 estimates); ≥5 years 0.46 (0.37 to 0.56); I2 = 99.0%, p 0.000 (14 estimates); <10 years 0.39 (0.28 to 0.51); I2 = 97.3%, p 0.000 (11 estimates); ≥10 years 0.50 (0.39 to 0.62); I2 = 99.0%, p 0.000 (11 estimates); <15 years 0.43 (0.34 to 0.51); I2 = 97.6%, p 0.000 (19 estimates); ≥15 years 0.54 (0.39 to 0.69); I2 = 98.8%, p 0.000 (6 estimates). By host country: USA <5 years 0.47 (0.31 to 0.63), I2 = 94.3%, p 0.000 (8 estimates); ≥5 years 0.43 (0.34 to 0.529); I2 = 98.9%, p 0.000 (15 estimates); <10 years 0·44 (0.33 to 0.55); I2 = 96.9%, p 0.000 (13 estimates); ≥10 years 0.45 (0.34 to 0.57); I2 = 99.1%, p 0.000 (10 estimates); <15 years 0.44 (0.36 to 0.52); I2 = 97.5%, p 0.000 (20 estimates); ≥15 years 0.50 (0.35 to 0.65); I2 = 99·9%, p 0.000 (5 estimates).
Alcohol Use
Immigrants showed increased risks of mild-to-moderate alcohol use with longer residence in North America [77, 102, 109], but unclear trends in heavy alcohol use [28, 35, 48]. Latino/Hispanic immigrants generally decreased their regular alcohol use with longer residence [38, 46], while Asian immigrants’ direction of risks varied widely [101, 115, 116, 129, 133]. There was evidence of increased risks of regular [102, 147] and heavy drinking with longer residence [100, 102] for immigrant men. Studies on immigrant women indicated increased risks with longer duration for regular [47, 61, 69, 102, 145] and heavy drinking [100, 102], especially among Latina/Hispanic women [47, 61]. There was little to no consensus on the direction of alcohol use patterns by residence in European countries. General, African, Latino/Hispanic, Eastern European and Middle Eastern immigrants showed both increased [26, 64, 125, 131] and decreased alcohol use [30, 45, 125, 131], depending on the receiving country.
In North America, immigrants consistently converged towards native levels of alcohol use [47, 77, 101, 102, 109], with limited evidence of diverging trends [38]. European studies with native reference groups failed to show consistent patterns of convergence/divergence [64, 131].
Pooled meta-analysis estimates showed lower odds of alcohol use among immigrants compared to natives (unadjusted OR 0.61, 95% CI 0.47–0.75, I2 = 93.5%; adjusted OR 0.73, 95% CI 0.57–0.88, I2 = 74.9%; Figure 3). Changes by duration of residence were observed in analyses of “All immigrants”, using 10 years as a cut-off (<10 years: OR 0.64, 95% CI 0.53 to 0.76, I2 = 0.0%, p = 0.489 (4 estimates); >10 years: OR 1.00, 95% CI 0.73 to 1.26, I2 = 53.6%, p = 0.116 (3 estimates)), suggesting convergence to native levels.
FIGURE 3
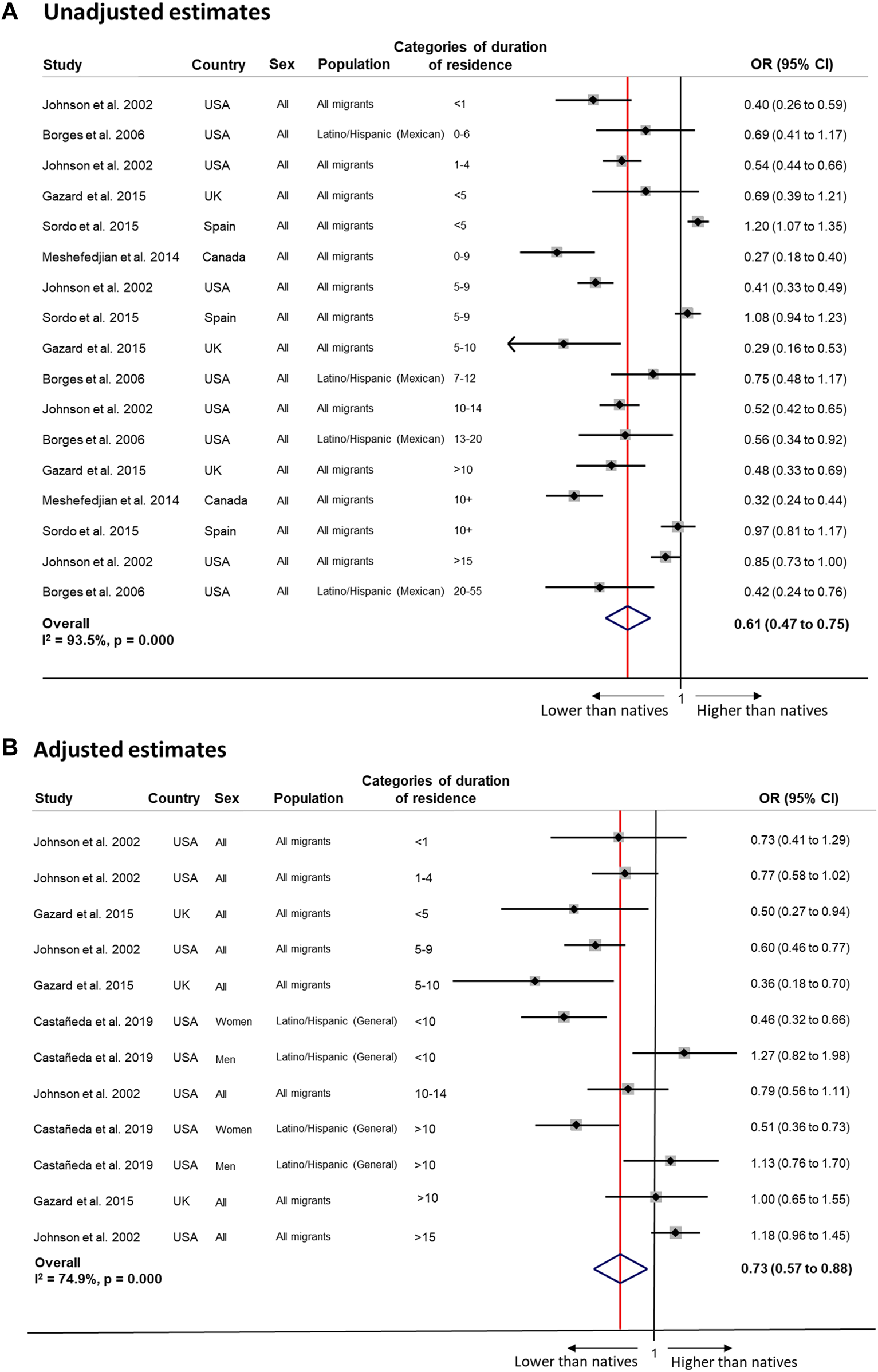
Random-effects meta-analysis of unadjusted (Panel (A)) and adjusted (Panel (B)) estimates of the association between alcohol and duration of residence among migrants compared to the native population (Sweden, 2022). Panel (A): <5 years 0.71 (0.31 to 1.11), I2 = 95.9%, p 0.000 (4 estimates); ≥5 years 0.60 (0.44 to 0.77); I2 = 92.4%, p 0.000 (11 estimates); <10 years 0.65 (0.41 to 0.90); I2 = 96.0%, p 0.000 (8 estimates); ≥10 years 0.59 (0.40 to 0.78); I2 = 90.3%, p 0.000 (7 estimates); <15 years 0.60 (0.45 to 0.76); I2 = 93.8%, p 0.000 (15 estimates); ≥15 years 0.65 (0.23 to 1.07); I2 = 87.9%, p 0.000 (2 estimates). By host country: USA <5 years 0.48 (0.35 to 0.61), I2 = 48.8%, p 0.162 (2 estimates); ≥5 years 0.58 (0.41 to 0.75), I2 = 85.0%, p 0.000 (6 estimates); <10 years 0.46 (0.37 to 0.56); I2 = 46.7%, p 0.131 (4 estimates); ≥10 years 0.60 (0.39 to 0.81); I2 = 81.8%, p 0.001 (4 estimates); <15 years 0.49 (0.42 to 0.57); I2 = 38.7%, p 0.134 (7 estimates); ≥15 years 0.65 (0.23 to 1.07); I2 = 87.9%, p 0.000 (2 estimates). Panel (B): <5 years 0.70 (0.53 to 0.86), I2 = 00.0%, p 0.412 (3 estimates); ≥5 years 0.75 (0.56 to 0.95); I2 = 80.9%, p 0.000 (9 estimates); <10 years 0.64 (0.48 to 0.79); I2 = 53.3%, p 0.058 (6 estimates); ≥10 years 0.90 (0.60 to 1.20); I2 = 81.3%, p 0.000 (5 estimates). By origin: “All migrants” <10 years: 0.64 (0.53 to 0.76); I2 = 0.0%, p 0.489 (4 estimates); ≥10 years 1.00 (0.73 to 1.26); I2 = 53.6%, p 0.116 (3 estimates). By host country: USA <5 years N/a; ≥5 years 0.79 (0.57 to 1.01); I2 = 82.7%, p 0.000 (7 estimates); <10 years 0.67 (0.49 to 0.85); I2 = 61.1%, p 0.036 (5 estimates); ≥10 years 0.88 (0.53 to 1.24); I2 = 85.4%, p 0.000 (4 estimates).
Drug Use
Increased risks of drug use with longer residence in North America [46, 77, 88, 97] and Europe [125, 131] were generally observed. All studies examining recent or lifetime cannabis use found increased risks with longer residence [88, 125, 131]. Studies on other drugs had mixed findings [46, 97, 131]. All [77, 88, 131] but one study [64] with a native reference suggested a convergence of immigrant drug use to native patterns, in some cases even surpassing native risks [131]. Findings were insufficient for meta-analysis.
Substance Use Diagnoses and Dependence
All studies examining substance use diagnoses or dependence, including drug-related, alcohol-related or unspecified diagnoses, came from North America [29, 37, 38, 41, 42, 91, 92, 118, 126, 132]. Most studies found increased risks of substance use diagnosis with longer residence, for immigrants of all origins [41, 118, 126], and specifically for Asian [41, 132], African/Afro-Caribbean [91, 92] and Latino/Hispanic immigrants [29, 38], with only a few studies finding no change [37] or unclear trends in diagnosis [38, 132]. Most studies with a native reference indicated convergence to native risks of substance use diagnosis [29, 38, 41, 42, 92, 126, 132]. Findings were insufficient for meta-analysis.
Physical Inactivity
Physical inactivity was divided into general/unspecified, leisure-time (e.g., exercise) and non-leisure-time (e.g., work-, travel-, household-related) physical inactivity. Studies examining indicators of physical activity were reverse interpreted.
North American evidence on changes in general physical inactivity by duration of residence varied from increased [98, 110, 113, 119, 127, 133–135, 142] to decreased [34, 51, 53, 54, 59, 62, 78, 115, 148] risks. Two European studies suggested either no change or increased inactivity with time [87, 108]. Studies from Australia, predominantly examining Asian or non-English-speaking immigrants, showed no consensus in the direction of behavioural changes [43, 76, 79, 137].
Meanwhile, immigrants largely decreased their risk of being inactive during leisure time with longer residence in North America, in both joint and sex-stratified analyses, as well as across multiple origins [27, 33, 44, 49, 54, 55, 59, 60, 63, 83, 89, 99, 110, 138, 144, 146, 148], excepting a few Canadian studies suggesting increased inactivity [93, 104, 109, 138]. European [56, 57, 108] and Australian [94] were limited and inconclusive. Non-leisure-time physical inactivity appeared to increase with longer residence in North America [27, 33, 59], especially among Latino/Hispanic and non-English-speaking immigrants [62, 68, 110, 148], with some conflicting evidence [54, 62, 148].
Altogether, most North American studies with native-born references suggested a convergence of physical inactivity patterns [34, 59, 60, 83, 109, 110, 113, 119, 138, 148], with only a few suggesting divergence [59, 84, 93, 138, 148]. Studies from outside North America showed mixed results regarding the direction of changes relative to natives.
Meta-analyses showed higher odds of any physical inactivity among immigrants compared to natives with unadjusted (OR 1.71, 95% CI 1.40–2.02, I2 = 99.1%) or adjusted estimates (OR 1.84, 95% CI 1.55–2.13, I2 = 97.6%), but no patterns by duration of residence (Figure 4).
FIGURE 4
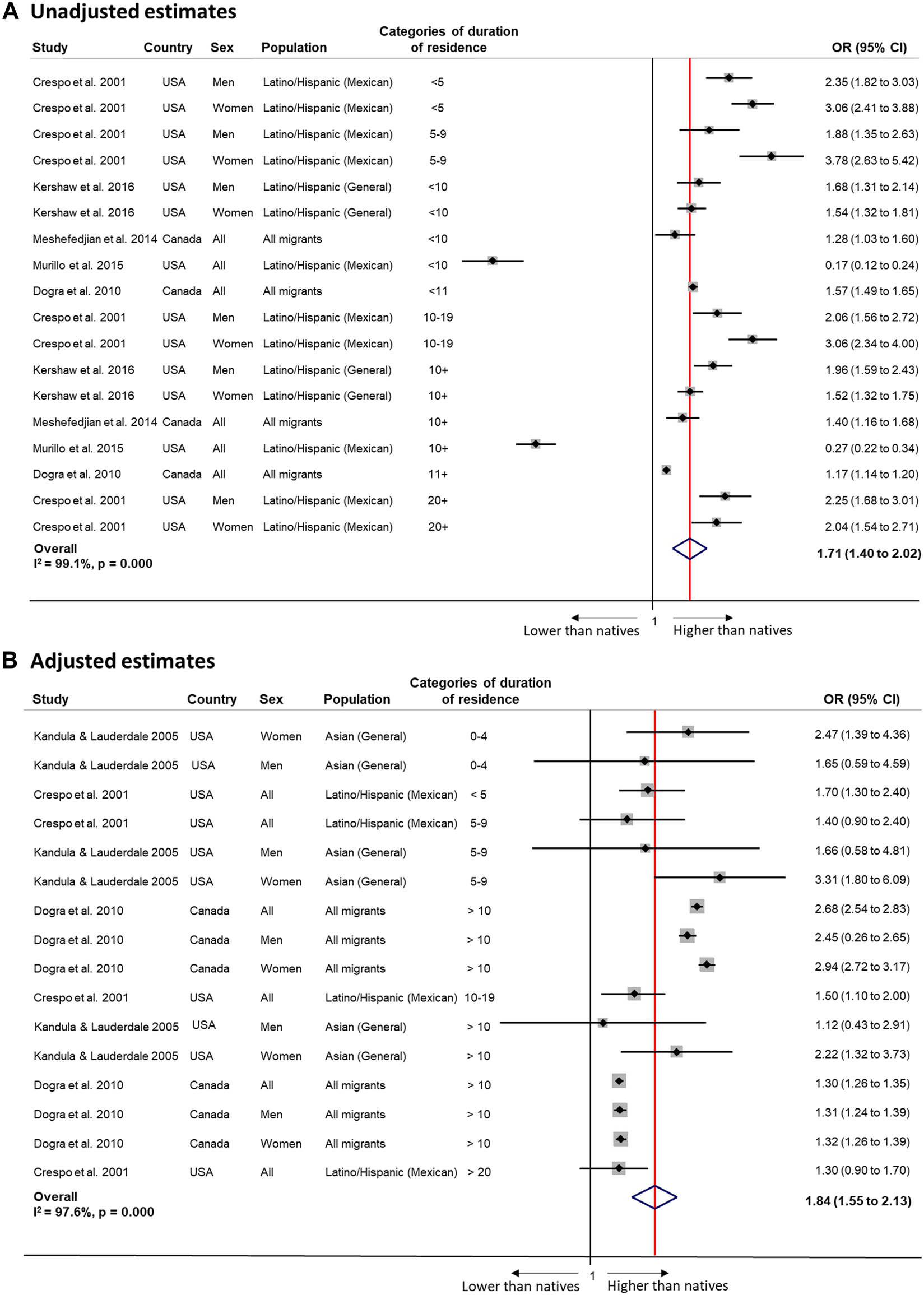
Random-effects meta-analysis of unadjusted (Panel (A)) and adjusted (Panel (B)) estimates of the association between physical activity and duration of residence among migrants compared to the native population (Sweden, 2022). Panel (A): <5 years 2.67 (1.98 to 3.37), I2 = 53.2%, p 0.144 (2 estimates); ≥5 years 1.79 (1.38 to 2.20); I2 = 98.8%, p 0.000 (11 estimates); <10 years 1.88 (1.10 to 2.65); I2 = 98.0%, p 0.000 (8 estimates); ≥10 years 1.68 (1.23 to 2.10); I2 = 99.0%, p 0.000 (9 estimates); <15 years 1.66 (1.33 to 1.99); I2 = 99.2%, p 0.000 (16 estimates); ≥15 years 2.13 (1.69 to 2.57); I2 = 00.0%, p 0.645 (2 estimates). Panel (B): <5 years 1.78 (1.29 to 2.28), I2 = 0.0%, p 0.629 (3 estimates); ≥5 years 1.83 (1.52 to 2.15); I2 = 98.1%, p 0.000 (13 estimates); <10 years 1.72 (1.32 to 2.12); I2 = 0.0%, p 0.578 (6 estimates); ≥10 years 1.31 (1 28 to 1 34); I2 = 0.0%, p 0.916 (5 estimates).
Dietary Habits
Narrative synthesis of dietary changes by duration of residence were subdivided into summative measures of daily energy intake [33, 44, 66, 93–95, 105, 133, 139, 140] and various healthy eating indices [44, 58, 73, 84, 105, 111, 119, 130, 141]. North American studies found greater energy intake among various immigrant groups by longer residence [33, 44, 93], with some studies suggesting no change [139, 140] or even decreased [133] intake among Asian immigrants. European [66, 105], Australian [94] and Israeli [95] findings suggested increased levels of energy intake with longer residence. Regarding healthy eating indices, most North American studies found greater scores, i.e., less unhealthy diets, by longer residence for immigrants of African/Afro-Caribbean [44, 73] and Latino/Hispanic origin [84, 105, 119, 141]. Evidence from Europe was mixed [58, 105, 111]. Studies with native references found converging risks in Canada [93], but diverging risks among Latino/Hispanic immigrants in the US, relative to US-born Latino/Hispanics [84, 119]. Findings were insufficient for meta-analysis.
Discussion
This systematic evaluation of the international literature demonstrates evidence of general changes in health risk behaviours by immigrants’ duration of residence, while also highlighting important heterogeneity in these patterns.
Narrative synthesis of the literature revealed that among general immigrant populations, especially women, increased risks of smoking were seen with longer residence in both North America and Europe. Similarly, North American studies demonstrated increased risks of (mild-to-moderate) alcohol and drug use with longer residence. Studies suggested increased levels of energy intake and less unhealthy dietary patterns, with decreased leisure-time but increased non-leisure-time inactivity risks with longer residence in North America. There were no consistent patterns in European studies for alcohol use, physical inactivity or diet scores. Although the narrative synthesis indicated that smoking, alcohol and drug use, and physical inactivity risks tended to converge to native-born reference levels in North America, studies of convergence or divergence in other contexts (mainly Europe) were fewer and less conclusive. The results of our narrative synthesis call for consideration of duration of residence as an instrument to monitor immigrants’ health behaviours over time in the receiving country.
Overall, the meta-analyses showed lower odds of smoking and alcohol use, but higher odds of physical inactivity among immigrants compared to natives, offering evidence of systematic differences in health risk behaviours between immigrants and natives. Yet, despite some signs of convergence, i.e., for alcohol use in North America, the meta-analyses did not provide robust support for a universal trend in health behaviours by duration of residence, nor for the convergence of risk behaviours to native levels (i.e., “regression to the mean”). The lack of such a universal pattern illustrates the role of different factors in immigrants’ adoption of health risk behaviours, contingent on the heterogeneity existing between specific migrant groups and within the reference native population. This observation deviates to a large extent from other universal trends (e.g., the healthy immigrant paradox) [24] which have been corroborated by meta-analyses despite large heterogeneity between groups.
Given that this is the first systematic review to consider immigrants’ changes in health behaviours by duration of residence, the reason for the lack of a universal trend across country contexts remains unknown. Previous studies considering health behavioural changes by acculturation (rather than duration of residence) attribute this heterogeneity to differences in the prevalence of health risk behaviours in the country of origin and destination, in combination with differences in origin and destination country norms and values (i.e., the operant model of acculturation) [149, 150]. The complexity of our review—which considers international evidence for many immigrant populations, receiving country contexts and health risk behaviours across a long time-span—does not permit a close evaluation of any specific model of change. However, we believe that our study offers a solid basis to build further studies in this direction.
Several important theoretical limitations with implications for public health interventions were identified in this review. Most studies assessing changes by duration of residence (alone or in combination with acculturation indices) motivate or interpret their results as a process of cultural assimilation (i.e., acculturation). The hegemonic use of cultural arguments to motivate the study of duration of residence effects lacks empirical support and is not sufficiently justified from a theoretical point of view. Most importantly, this practice could limit consideration of alternative, time-dependent mechanisms and potential targets for public health intervention. Cumulative experiences of (increasing) social inequalities in the receiving country could alternatively explain changes in health risk behaviours. For instance, lack of material resources could limit possibilities to make healthy choices, including buying healthy food or participating in physical activity, while unhealthy habits could further stem from the psychosocial stress of economic instability as well as racism or discrimination [151–153]. Thus, the social determinants of health [154] may be more relevant for the interpretation of these results than acculturation, with social policies as important instruments of change. Within this framework, our lack of evidence for a universal pattern of change in health risk behaviours could reflect heterogeneity stemming from various upstream social factors in the receiving country. In fact, recent systematic evidence has highlighted the often uncaptured adverse health effects of restrictive entry and integration policies for immigrants worldwide [155].
Our efforts to synthesise the literature also revealed several methodological limitations. Importantly, most of the captured studies used cross-sectional data, limiting the evaluation and interpretation of actual behavioural changes over time. Although studies include multiple controls (e.g., education, employment, income, marital status, language and acculturation), authors may unwittingly control for potential mediators (i.e., explanations for differences) in their effort to rule out compositional differences between groups with different lengths of residence. This practice is common and even less justified in longitudinal studies. For this reason, we ran meta-analyses using available unadjusted estimates (or when data allowed for calculation) to be able to evaluate possible statistical bias. However, models using unadjusted estimates led to similar conclusions, so it is unlikely that the lack of concrete findings regarding health-behavioural patterning is due to over-adjustment.
Certain reference groups, i.e., established immigrants, may also have enlarged compositional differences, making it difficult to test convergence to the norm. Furthermore, these populations may represent a selectively healthy group, given the increasing propensity of return migration with poorer health (i.e., so-called salmon bias) [156]. Thus, we focused on native reference populations in the meta-analyses. In some studies, second-generation immigrants were also equated as natives, and although not immigrants themselves, the second generation may continue to experience stable or growing health inequalities. Including them as a reference population could lead to over- or under-estimation of first-generation changes.
The lack of justification for different duration of residence categories is also a limitation. Studies typically did not specify whether this selection was data-driven, dependent on receiving-country-specific migration trajectories or corresponding to international conventions. Researchers should develop a standardised operationalisation of duration of residence categories with public health relevance to facilitate international comparisons, e.g., by five-, ten- or fifteen-year intervals.
Data limitations, such as small sample size, might have constrained the possibility of evaluating variations by country of birth when assessing changes in immigrants’ health risk behaviours, as well as the possibility of offering gender-specific comparisons. This was especially the case for the meta-analysed studies, which represented a subset of the published studies on the topic, thus limiting the generalisability of the meta-analysis findings beyond that of the narrative synthesis results. Overall, further studies are needed to fill this gap as well as to contribute evidence from other areas of the world, beyond North America and Europe.
Given that research is more likely to exclude insignificant duration of residence effects in favour of general associations between migration status and health risk behaviours, any publication bias would likely have led to an overestimation of duration of residence effects, which we do not observe. Yet, given that only studies with duration of residence measures were included, our results of overall health behavioural differences between immigrants and natives, irrespective of duration of residence, should be interpreted with caution. On the other hand, these results could be more representative of immigrant populations than results from single studies which do not consider duration of residence, as the latter may overrepresent newly-arrived or long-term immigrants.
To our knowledge, this is the first study to comprehensively synthesise 20 years of international evidence on changes in health risk behaviours by immigrants’ duration of residence. We found evidence for changing patterns by immigrants’ duration of residence, yet the existence of a clear, universal trend in behavioural changes was called into question by the meta-analyses. This nuance highlights the importance of considering alternative theoretical frameworks regarding the role of receiving country contexts, including structural factors as well as entry and integration policies, as potential explanations of this variation. Finally, this evaluation identified several methodological challenges to address in future research, including the need for longitudinal studies, comparative duration of residence categorisations, deliberate adjustment methods and thorough consideration of reference populations.
Conclusion
Duration of residence could serve as an effective public health instrument for monitoring, predicting and preventing developments in immigrants’ health risk behaviours, conditional on immigrants’ background characteristics and contextual factors. In combination with other relevant information, such as age at migration and country of origin, this instrument could help to tailor and evaluate targeted public health interventions by considering when (with regards to time after migration) to act for specific immigrant populations in specific contexts. Duration of residence data can be easily collected through questionnaires and administrative registers. Furthermore, it is increasingly acknowledged that the adoption of health risk behaviours is largely influenced by socioeconomic conditions at the individual, community and societal levels, factors which cannot be captured by traditional acculturation measures but can be operationalised within the duration of residence framework. Thus, by studying patterns of health risk behaviours by immigrants’ duration of residence in different receiving contexts, researchers can evaluate the role of societal conditions in shaping immigrant health over time.
Statements
Author contributions
SJ and HH conceived the idea for the study. SJ, HH, N-KG, and LB planned and designed the study. HH developed the search strategy and carried out the database searches. N-KG and LB performed the screening and selection of papers by title and abstract. Full-length articles were reviewed by SJ, HH, N-KG, and LB. SJ, HH, N-KG, and LB did the data extraction, synthesis and quality assessments. SJ carried out the meta-analysis. SJ, HH, and LB drafted the manuscript with substantive contributions from MR. All authors contributed to the interpretation of findings and critical revision of the manuscript. All authors approved the final version submitted for publication.
Funding
This study was funded by the Swedish Council for Health, Working Life and Welfare (FORTE, Grant #2016–07128 and #2021-00271) and Swedish Research Council (VR, grant #2018–01825). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2022.1604437/full#supplementary-material
References
1.
Lim SS Vos T Flaxman AD Danaei G Shibuya K Adair-Rohani H et al A Comparative Risk Assessment of Burden of Disease and Injury Attributable to 67 Risk Factors and Risk Factor Clusters in 21 Regions, 1990–2010: A Systematic Analysis for the Global Burden of Disease Study 2010. Lancet (2012) 380:2224–60. 10.1016/S0140-6736(12)61766-8
2.
Ezzati M Riboli E . Behavioral and Dietary Risk Factors for Noncommunicable Diseases. N Engl J Med (2013) 369(954–64):954–64. 10.1056/NEJMra1203528
3.
Mackenbach J . The Persistence of Health Inequalities in Modern Welfare States: The Explanation of a Paradox. Soc Sci Med (2017) 75(4):761–9. 10.1016/j.socscimed.2012.02.031
4.
Goldberg M Zins M Kivimäki M Marmot M Sabia S Singh-Manoux A . Health behaviours, socioeconomic status, and mortality: Further analyses of the British whitehall II and the French GAZEL prospective cohorts. Plos Med (2011) 8(2):e1000419. 10.1371/journal.pmed.1000419
5.
Pampel FC Krueger PM Denney JT . Socioeconomic disparities in health behaviors. Annu Rev Sociol (2010) 36:349–70. 10.1146/annurev.soc.012809.102529
6.
Antecol H Bedard K . Unhealthy assimilation: Why do immigrants converge to American health status level?Demography (2006) 43(2):337–60. 10.1353/dem.2006.0011
7.
Gotay CC Reid MS Dawson MY Wang S . Acculturation and smoking in North Americans of Chinese ancestry: A systematic review. Can J Public Health (2015) 106(5):e333–40. 10.17269/cjph.106.4762
8.
Choi S Rankin S Stewart A Oka R . Effects of acculturation on smoking behavior in asian Americans: A meta-analysis. J Cardiovasc Nurs (2008) 23(1):67–73. 10.1097/01.JCN.0000305057.96247.f2
9.
Lui PP Zamboanga BL . Acculturation and alcohol use among asian Americans: A meta-analytic review. Psychol Addict Behav (2018) 32(2):173–86. 10.1037/adb0000340
10.
Kondo KK Rossi JS Schwartz SJ Zamboanga BL Scalf CD . Acculturation and cigarette smoking in hispanic women: A meta-analysis. J Ethn Subst Abuse (2016) 15(1):46–72. 10.1080/15332640.2014.1002878
11.
Lui PP Zamboanga BL . A critical review and meta-analysis of the associations between acculturation and alcohol use outcomes among Hispanic Americans. Alcohol Clin Exp Res (2018) 42(10):1841–62. 10.1111/acer.13845
12.
Yi JY Chen Y Hussong AM Daughters SB . Acculturation and substance use among Hispanic-Latino and Asian adolescents. Curr Psychiatry Rev (2016) 12(2):139–49. 10.2174/1573400512666160216234716
13.
Zemore SE . Acculturation and alcohol among Latino adults in the United States: A comprehensive review. Alcohol Clin Exp Res (2007) 31(12):1968–90. 10.1111/j.1530-0277.2007.00532.x
14.
Reiss K Lehnhardt J Razum O . Factors associated with smoking in immigrants from non-Western to Western countries - What role does acculturation play? A systematic review. Tob Induc Dis (2015) 16(13):11. 10.1186/s12971-015-0036-9
15.
Gerber M Barker D Pühse U . Acculturation and physical activity among immigrants: A systematic review. J Public Health (2012) 20(3):313–41. 10.1007/s10389-011-0443-1
16.
Sanou D O'Reilly E Ngnie-Teta I Batal M Mondain N Andrew C et al Acculturation and nutritional health of immigrants in Canada: A scoping review. J Immigr Minor Health (2014) 16(1):24–34. 10.1007/s10903-013-9823-7
17.
Moher D Liberati A Tetzlaff J Altman D PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLOS Med (2009) 6(7):e1000097. 10.1371/journal.pmed.1000097
18.
Berg L Gustafsson N-K Honkaniemi H Juárez S . Health risk behaviours among migrants by duration of residence: Protocol for a systematic review and meta-analysis. BMJ open (2020) 27(1010):e038388. 10.1136/bmjopen-2020-038388
19.
Wells G Shea B O'Connell D Peterson J Welch V Losos M et al The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa, Canada: Ottawa Hospital Research Institute (2009).
20.
Campbell M McKenzie J Sowden A Katikireddi S Brennan S Bllis S et al Synthesis without meta-analysis (SWiM) in systematic reviews: Reporting guideline. BMJ (2020) 16(368):l6890. 10.1136/bmj.l6890
21.
Borenstein M Hedges L Higgins J Rothstein H . A basic introduction to fixedeffect and randomeffects models for metaanalysis. Res Synth Methods (2010) 1(2):97–111. 10.1002/jrsm.12
22.
StataCorp. Stata. 13 ed.College Station: Texas: StataCorp (2013).
23.
Higgins JP Thompson SG Deeks JJ Altman DG . Measuring inconsistency in meta-analyses. BMJ (2003) 6(7474):557–60. 10.1136/bmj.327.7414.557
24.
Aldridge R Nellums L Bartlett S Barr A Patel P Burns R et al Global patterns of mortality in international migrants: A systematic review and meta-analysis. Lancet (2018) 15(39210164):2553–66. 10.1016/S0140-6736(18)32781-8
25.
Stroup D Berlin J Morton S Olkin I Williamson D Rennie D et al Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-Analysis of observational studies in Epidemiology (MOOSE) group. JAMA (2000) 283(15):2008–12. 10.1001/jama.283.15.2008
26.
Addo J Cook S Galbete C Agyemang C Klipstein-Grobusch K Nicolaou M et al Differences in alcohol consumption and drinking patterns in Ghanaians in Europe and Africa: The RODAM Study. PLOS One (2018) 13(11):e0206286. 10.1371/journal.pone.0206286
27.
Afable A Yeh M-C Trivedi T Andrews E Wylie-Rosett J . Duration of US residence and obesity risk in NYC Chinese immigrants. J Immigr Minor Health (2016) 18(3):624–35. 10.1007/s10903-015-0216-y
28.
Agic B Mann RE Tuck A Ialomiteanu A Bondy S Simich L et al Alcohol use among immigrants in Ontario, Canada. Drug Alcohol Rev (2016) 35(2):196–205. 10.1111/dar.12250
29.
Alegría M Mulvaney-Day N Torres M Polo A Cao Z Canino G et al Prevalence of psychiatric disorders across Latino subgroups in the United States. Am J Public Health (2007) 97(1):68–75. 10.2105/AJPH.2006.087205
30.
Amundsen EJ . Low level of alcohol drinking among two generations of non-western immigrants in oslo: A multi-ethnic comparison. BMC Public Health (2012) 12(1):535. 10.1186/1471-2458-12-535
31.
An N Cochran SD Mays VM McCarthy WJ . Influence of American acculturation on cigarette smoking behaviors among Asian American subpopulations in California. Nicotine Tob Res (2008) 10(4):579–87. 10.1080/14622200801979126
32.
Azagba S Shan L Latham K . Assessing trends and healthy migrant paradox in cigarette smoking among US immigrant adults. Prev Med (2019) 129:105830. 10.1016/j.ypmed.2019.105830
33.
Basu S Insler MA . The body mass index assimilation of US immigrants: Do diet and exercise contribute?East Econ J (2018) 44(3):337–63. 10.1057/s41302-017-0097-y
34.
Bayog ML Waters CM . Nativity, chronic health conditions, and health behaviors in Filipino Americans. J Transcult Nurs (2018) 29(3):249–57. 10.1177/1043659617703164
35.
Bharmal N Kaplan RM Shapiro MF Mangione CM Kagawa-Singer M Wong MD et al The association of duration of residence in the United States with cardiovascular disease risk factors among South Asian immigrants. J Immigr Minor Health (2015) 17(3):781–90. 10.1007/s10903-013-9973-7
36.
Bingham BA Duong MT Ricks M Mabundo LS Baker RL Jr Utumatwishima JN et al The association between stress measured by allostatic load score and physiologic dysregulation in african immigrants: The africans in America study. Front Public Health (2016) 4:265. 10.3389/fpubh.2016.00265
37.
Blanco C Morcillo C Alegría M Dedios MC Fernández-Navarro P Regincos R et al Acculturation and drug use disorders among Hispanics in the US. J Psychiatr Res (2013) 47(2):226–32. 10.1016/j.jpsychires.2012.09.019
38.
Borges G Medina-Mora ME Lown A Ye Y Robertson MJ Cherpitel C et al Alcohol use disorders in national samples of Mexicans and Mexican-Americans: The Mexican national addiction survey and the US national alcohol survey. Hisp J Behav Sci (2006) 28(3):425–49. 10.1177/0739986306291502
39.
Bostean G Ro A Fleischer NL . Smoking trends among US Latinos, 1998–2013: The impact of immigrant arrival cohort. Int J Environ Res Public Health (2017) 14(3):255. 10.3390/ijerph14030255
40.
Brathwaite R Addo J Kunst AE Agyemang C Owusu-Dabo E de-Graft Aikins A et al Smoking prevalence differs by location of residence among Ghanaians in Africa and Europe: The RODAM study. PLOS One (2017) 12(5):e0177291. 10.1371/journal.pone.0177291
41.
Breslau J Chang DF . Psychiatric disorders among foreign-born and US-born Asian-Americans in a US national survey. Soc Psychiatry Psychiatr Epidemiol (2006) 41(12):943–50. 10.1007/s00127-006-0119-2
42.
Breslau J Aguilar-Gaxiola S Borges G Kendler KS Su M Kessler RC et al Risk for psychiatric disorder among immigrants and their US-born descendants: Evidence from the National Comorbidity Survey-Replication. J Nerv Ment Dis (2007) 195(3):189–95. 10.1097/01.nmd.0000243779.35541.c6
43.
Brock K Lockwood E Cant B Bermingham M Tran-Dinh H . An investigation of health behavior change in Vietnamese-born individuals living in Sydney, Australia. Ethn Dis (2001) 11(3):385–90.
44.
Brown AG Houser RF Mattei J Rehm CD Mozaffarian D Lichtenstein AH et al Diet quality among US-born and foreign-born non-hispanic blacks: NHANES 2003–2012 data. Am J Clin Nutr (2018) 107(5):695–706. 10.1093/ajcn/nqy021
45.
Canfield M Worrell M Gilvarry C . Determinants of substance use amongst Brazilians residing in the UK: The role of acculturation. Drug Alcohol Rev (2017) 36(6):751–60. 10.1111/dar.12530
46.
Cano MÁ Sánchez M Trepka MJ Dillon FR Sheehan DM Rojas P et al Immigration stress and alcohol use severity among recently immigrated Hispanic adults: Examining moderating effects of gender, immigration status, and social support. J Clin Psychol (2017) 73(3):294–307. 10.1002/jclp.22330
47.
Castañeda SF Garcia ML Lopez-Gurrola M Stoutenberg M Emory K Daviglus ML et al Alcohol use, acculturation and socioeconomic status among Hispanic/Latino men and women: The Hispanic Community Health Study/Study of Latinos. PLOS One (2019) 14(4):e0214906. 10.1371/journal.pone.0214906
48.
Chartier KG Thomas NS Kendler KS . Interrelationship between family history of alcoholism and generational status in the prediction of alcohol dependence in US Hispanics. Psychol Med (2017) 47(1):137–47. 10.1017/S0033291716002105
49.
Choi J Wilbur J Miller A Szalacha L McAuley E . Correlates of leisure-time physical activity in Korean immigrant women. West J Nurs Res (2008) 30(5):620–38. 10.1177/0193945907310645
50.
Chou C-F Johnson PJ Blewett LA . Immigration and selected indicators of health status and healthcare utilization among the Chinese. J Immigr Minor Health (2010) 12(4):470–9. 10.1007/s10903-009-9240-0
51.
Commodore-Mensah Y Ukonu N Cooper LA Agyemang C Himmelfarb CD . The association between acculturation and cardiovascular disease risk in Ghanaian and Nigerian-born african immigrants in the United States: The afro-cardiac study. J Immigr Minor Health (2018) 20(5):1137–46. 10.1007/s10903-017-0644-y
52.
Constantine ML Adejoro OO D’Silva J Rockwood TH Schillo BA . Evaluation of use of stage of tobacco epidemic to predict post-immigration smoking behaviors. Nicotine Tob Res (2013) 15(11):1910–7. 10.1093/ntr/ntt077
53.
Coronado GD Woodall ED Do H Li L Yasui Y Taylor VM et al Heart disease prevention practices among immigrant Vietnamese women. J Womens Health (2008) 17(8):1293–300. 10.1089/jwh.2007.0751
54.
Creighton MJ Goldman N Pebley AR Chung CY . Durational and generational differences in Mexican immigrant obesity: Is acculturation the explanation?Soc Sci Med (2012) 75(2):300–10. 10.1016/j.socscimed.2012.03.013
55.
Crespo CJ Smit E Carter-Pokras O Andersen R . Acculturation and leisure-time physical inactivity in Mexican American adults: Results from NHANES III, 1988–1994. Am J Public Health (2001) 91(8):1254–7. 10.2105/ajph.91.8.1254
56.
Dawson AJ Sundquist J Johansson S-E . The influence of ethnicity and length of time since immigration on physical activity. Ethn Health (2005) 10(4):293–309. 10.1080/13557850500159965
57.
De Munter JS Agyemang C Van Valkengoed IG Bhopal R Zaninotto P Nazroo J et al Cross national study of leisure-time physical activity in Dutch and English populations with ethnic group comparisons. Eur J Public Health (2013) 23(3):440–6. 10.1093/eurpub/cks088
58.
Delisle HF Vioque J Gil A . Dietary patterns and quality in West-African immigrants in Madrid. Nutr J (2009) 8(1):3. 10.1186/1475-2891-8-3
59.
Dogra S Meisner BA Ardern CI . Variation in mode of physical activity by ethnicity and time since immigration: A cross-sectional analysis. Int J Behav Nutr Phys Act (2010) 7(1):75. 10.1186/1479-5868-7-75
60.
Echeverría SE Pentakota SR Abraído-Lanza AF Janevic T Gundersen DA Ramirez SM et al Clashing paradigms: An empirical examination of cultural proxies and socioeconomic condition shaping Latino health. Ann Epidemiol (2013) 23(10):608–13. 10.1016/j.annepidem.2013.07.023
61.
Ertl MM Dillon FR Martin JL Babino R De La Rosa M . Alcohol use exacerbates acculturative stress among recently immigrated, young adult Latinas. J Immigr Minor Health (2018) 20(3):594–602. 10.1007/s10903-017-0586-4
62.
Evenson KR Sarmiento OL Ayala GX . Acculturation and physical activity among North Carolina Latina immigrants. Soc Sci Med (2004) 59(12):2509–22. 10.1016/j.socscimed.2004.04.011
63.
Gaskins RB Baskin ML Person SD . Language, duration of United States residency, and leisure time physical activity among women from the Third National Health and Nutrition Examination Survey (NHANES III). J Womens Health (2012) 21(11):1170–9. 10.1089/jwh.2012.3477
64.
Gazard B Frissa S Nellums L Hotopf M Hatch SL . Challenges in researching migration status, health and health service use: An intersectional analysis of a south london community. Ethn Health (2015) 20(6):564–93. 10.1080/13557858.2014.961410
65.
Glenn BA Surani Z Chawla N Bastani R . Tobacco use among south asians: Results of a community–University collaborative study. Ethn Health (2009) 14(2):131–45. 10.1080/13557850802307817
66.
Goff LM Timbers L Style H Knight A . Dietary intake in Black British adults; an observational assessment of nutritional composition and the role of traditional foods in UK Caribbean and West African diets. Public Health Nutr (2015) 18(12):2191–201. 10.1017/S1368980014002584
67.
Gorman BK Lariscy JT Kaushik C . Gender, acculturation, and smoking behavior among US Asian and Latino immigrants. Soc Sci Med (2014) 106:110–8. 10.1016/j.socscimed.2014.02.002
68.
Ham SA Yore MM Kruger J Moeti R Heath GW . Physical activity patterns among latinos in the United States: Putting the pieces together. Prev Chronic Dis (2007) 4(4):A92.
69.
Hardie TL Polek C Garcia V González L Welsh M . Drinks per day in women of Mexican origin: Does birth place matter?J Addict Nurs (2013) 24(3):173–9. 10.1097/JAN.0b013e3182a4cc0a
70.
Hislop TG Tu S-P Teh C Li L Low A Taylor VM et al Knowledge and behaviour regarding heart disease prevention in Chinese Canadian immigrants. Can J Public Health (2008) 99(3):232–5. 10.1007/bf03405480
71.
Holmes LM Marcelli EA . Neighborhood social cohesion and smoking among legal and unauthorized Brazilian migrants in metropolitan Boston. J Urban Health (2014) 91(6):1175–88. 10.1007/s11524-014-9912-5
72.
Hu SS Pallonen UE Meshack AF . The impact of immigration status on tobacco use among Chinese-American adults in Texas. J Immigr Minor Health (2010) 12(2):206–14. 10.1007/s10903-007-9097-z
73.
Huffman FG Vaccaro JA Zarini GG Dixon Z . Comparison of two indices of diet quality with acculturation factors and demographics in Haitian Americans. Ecol Food Nutr (2014) 53(1):42–57. 10.1080/03670244.2013.774674
74.
Hyman I Fenta H Noh S . Gender and the smoking behaviour of Ethiopian immigrants in Toronto. Chronic Dis Can (2008) 28(4):121–7. 10.24095/hpcdp.28.4.02
75.
Jayaweera H Quigley MA . Health status, health behaviour and healthcare use among migrants in the UK: Evidence from mothers in the millennium cohort study. Soc Sci Med (2010) 71(5):1002–10. 10.1016/j.socscimed.2010.05.039
76.
Jin K Gullick J Neubeck L Koo F Ding D . Acculturation is associated with higher prevalence of cardiovascular disease risk-factors among Chinese immigrants in Australia: Evidence from a large population-based cohort. Eur J Prev Cardiol (2017) 24(18):2000–8. 10.1177/2047487317736828
77.
Johnson TP VanGeest JB Cho YI . Migration and substance use: Evidence from the US national health interview survey. Subst Use Misuse (2002) 37(8-10):941–72. 10.1081/ja-120004160
78.
Jonnalagadda SS Diwan S . Health behaviors, chronic disease prevalence and self-rated health of older Asian Indian immigrants in the US. J Immigr Health (2005) 7(2):75–83. 10.1007/s10903-005-2640-x
79.
Joshi S Jatrana S Paradies Y . Are immigrants more physically active than native-born Australians and does it changes over time? Evidence from a nationally representative longitudinal survey. J Phys Act Health (2017) 14(2):145–54. 10.1123/jpah.2016-0002
80.
Joshi S Jatrana S Paradies Y . Tobacco smoking between immigrants and non‐immigrants in Australia: A longitudinal investigation of the effect of nativity, duration of residence and age at arrival. Health Promot J Austr (2018) 29(3):282–92. 10.1002/hpja.19
81.
Juonl HS Kimz M Hanz H Ryu JP Han W . Acculturation and cigarette smoking among Korean American men.Yonsei Med J (2003) 44(5):875–82. 10.3349/ymj.2003.44.5.875
82.
Kabir Z Clarke V Keogan S Currie LM Zatonski W Clancy L et al Smoking characteristics of polish immigrants in dublin. BMC Public Health (2008) 8(1):428. 10.1186/1471-2458-8-428
83.
Kandula NR Lauderdale DS . Leisure time, non-leisure time, and occupational physical activity in Asian Americans. Ann Epidemiol (2005) 15(4):257–65. 10.1016/j.annepidem.2004.06.006
84.
Kershaw KN Giacinto RE Gonzalez F Isasi CR Salgado H Stamler J et al Relationships of nativity and length of residence in the US with favorable cardiovascular health among hispanics/latinos: The hispanic community health study/study of latinos (HCHS/SOL). Prev Med (2016) 89:84–9. 10.1016/j.ypmed.2016.05.013
85.
Khlat M Legleye S Bricard D . Migration-related changes in smoking among non-Western immigrants in France. Eur J Public Health (2019) 29(3):453–7. 10.1093/eurpub/cky230
86.
Kim SS Lee HO Kiang P Kalman D Ziedonis DM . Factors associated with alcohol problems among asian American college students: Gender, ethnicity, smoking and depressed mood. J Subst Use (2014) 19(1-2):12–7. 10.3109/14659891.2012.709912
87.
Koca C Lapa TY . Analysis of physical activity and acculturation among Turkish migrants in Germany and England. Percept Mot Skills (2014) 119(3):698–716. 10.2466/06.PMS.119c29z7
88.
Kolar K Erickson P Hathaway A Osborne G . Differentiating the drug normalization framework: A quantitative assessment of cannabis use patterns, accessibility, and acceptability attitudes among University undergraduates. Subst Use Misuse (2018) 53(14):2339–49. 10.1080/10826084.2018.1474226
89.
Koya DL Egede LE . Association between length of residence and cardiovascular disease risk factors among an ethnically diverse group of United States immigrants. J Gen Intern Med (2007) 22(6):841–6. 10.1007/s11606-007-0163-y
90.
Kuerban A . Healthy migrant effect on smoking behavior among Asian immigrants in the United States. J Immigr Minor Health (2016) 18(1):94–101. 10.1007/s10903-014-0155-z
91.
Lacey KK Sears KP Govia IO Forsythe-Brown I Matusko N Jackson JS et al Substance use, mental disorders and physical health of Caribbeans at-home compared to those residing in the United States. Int J Environ Res Public Health (2015) 12(1):710–34. 10.3390/ijerph120100710
92.
Lacey KK Mouzon DM Govia IO Matusko N Forsythe-Brown I Abelson JM et al Substance abuse among Blacks across the diaspora. Subst Use Misuse (2016) 51(9):1147–58. 10.3109/10826084.2016.1160124
93.
Lear SA Humphries KH Hage-Moussa S Chockalingam A Mancini GJ . Immigration presents a potential increased risk for atherosclerosis. Atherosclerosis (2009) 205(2):584–9. 10.1016/j.atherosclerosis.2008.12.037
94.
Lee W-P Lingard J Bermingham M . Change in diet and body mass index in Taiwanese women with length of residence in Australia. Asia Pac J Clin Nutr (2007) 16(1):56–65.
95.
Leshem M Dessie-Navon H . Acculturation of immigrant diet, basic taste responses and sodium appetite. J Nutr Sci (2018) 7:e21. 10.1017/jns.2018.12
96.
Leung LA . Healthy and unhealthy assimilation: Country of origin and smoking behavior among immigrants. Health Econ (2014) 23(12):1411–29. 10.1002/hec.2992
97.
Levy V Page-Shafer K Evans J Ruiz J Morrow S Reardon J et al HIV-related risk behavior among Hispanic immigrant men in a population-based household survey in low-income neighborhoods of northern California. Sex Transm Dis (2005) 32(8):487–90. 10.1097/01.olq.0000161185.06387.94
98.
Li J Hummer RA . The relationship between duration of US residence, educational attainment, and adult health among Asian immigrants. Popul Res Pol Rev (2015) 34(1):49–76. 10.1007/s11113-014-9344-7
99.
Li K Wen M . Racial and ethnic disparities in leisure-time physical activity in California: Patterns and mechanisms. Race Soc Probl (2013) 5(3):147–56. 10.1007/s12552-013-9087-9
100.
Li K Wen M . Substance use, age at migration, and length of residence among adult immigrants in the United States. J Immigr Minor Health (2015) 17(1):156–64. 10.1007/s10903-013-9887-4
101.
Lo CC Cheng TC Howell RJ . The role of immigration status in heavy drinking among Asian Americans. Subst Use Misuse (2014) 49(8):932–40. 10.3109/10826084.2013.852578
102.
Lopez-Gonzalez L Aravena VC Hummer RA . Immigrant acculturation, gender and health behavior: A research note. Social Forces (2005) 84(1):581–93. 10.1353/sof.2005.0112
103.
Maffini CS Vaughan EL Wong YJ . Life transitions and smoking among Asian Americans. Asian Am J Psychol (2015) 6(1):81–7. 10.1037/a0037203
104.
Mahmood B Bhatti JA Leon A Gotay C . Leisure time physical activity levels in immigrants by ethnicity and time since immigration to Canada: Findings from the 2011–2012 Canadian Community Health Survey. J Immigr Minor Health (2019) 21(4):801–10. 10.1007/s10903-018-0789-3
105.
Marín-Guerrero A Rodríguez-Artalejo F Guallar-Castillón P López-García E Gutiérrez-Fisac JL . Association of the duration of residence with obesity-related eating habits and dietary patterns among Latin-American immigrants in Spain. Br J Nutr (2015) 113(2):343–9. 10.1017/S0007114514003614
106.
Maxwell AE Bernaards CA McCarthy WJ . Smoking prevalence and correlates among Chinese-and Filipino-American adults: Findings from the 2001 California health interview survey. Prev Med (2005) 41(2):693–9. 10.1016/j.ypmed.2005.01.014
107.
Maxwell AE Garcia GM Berman BA . Understanding tobacco use among Filipino American men. Nicotine Tob Res (2007) 9(7):769–76. 10.1080/14622200701397890
108.
Méjean C Traissac P Eymard-Duvernay S Delpeuch F Maire B . Influence of acculturation among Tunisian migrants in France and their past/present exposure to the home country on diet and physical activity. Public Health Nutr (2009) 12(6):832–41. 10.1017/S1368980008003285
109.
Meshefedjian GA Leaune V M-È S Drouin M . Disparities in lifestyle habits and health related factors of montreal immigrants: Is immigration an important exposure variable in public health?J Immigr Minor Health (2014) 16(5):790–7. 10.1007/s10903-013-9839-z
110.
Murillo R Albrecht SS Daviglus ML Kershaw KN . The role of physical activity and sedentary behaviors in explaining the association between acculturation and obesity among Mexican-American adults. Am J Health Promot (2015) 30(1):50–7. 10.4278/ajhp.140128-QUAN-49
111.
Nicolaou M Van Dam RM Stronks K . Acculturation and education level in relation to quality of the diet: A study of Surinamese south asian and afro‐caribbean residents of The Netherlands. J Hum Nutr Diet (2006) 19(5):383–93. 10.1111/j.1365-277X.2006.00720.x
112.
Osei-Kwasi HA Boateng D Danquah I Holdsworth M Mejean C Terragni L et al Acculturation and food intake among Ghanaian migrants in Europe: Findings from the RODAM study. J Nutr Educ Behav (2020) 52(2):114–25. 10.1016/j.jneb.2019.09.004
113.
Osypuk TL Roux AVD Hadley C Kandula NR . Are immigrant enclaves healthy places to live? The multi-ethnic study of atherosclerosis. Soc Sci Med (2009) 69(1):110–20. 10.1016/j.socscimed.2009.04.010
114.
Pampel F Khlat M Bricard D Legleye S . Smoking among immigrant groups in the United States: Prevalence, education gradients, and male-to-female ratios. Nicotine Tob Res (2020) 22(4):532–8. 10.1093/ntr/ntz022
115.
Parikh NS Fahs MC Shelley D Yerneni R . Health behaviors of older Chinese adults living in New York City. J Community Health (2009) 34(1):6–15. 10.1007/s10900-008-9125-5
116.
Park S-Y Anastas J Shibusawa T Nguyen D . The impact of acculturation and acculturative stress on alcohol use across Asian immigrant subgroups. Subst Use Misuse (2014) 49(8):922–31. 10.3109/10826084.2013.855232
117.
Patel M Mistry R Maxwell AE Divan HA McCarthy WJ . Contextual factors related to conventional and traditional tobacco use among California Asian Indian immigrants. J Community Health (2018) 43(2):280–90. 10.1007/s10900-017-0419-3
118.
Patterson B Kyu HH Georgiades K . Age at immigration to Canada and the occurrence of mood, anxiety, and substance use disorders. Can J Psychiatry (2013) 58(4):210–7. 10.1177/070674371305800406
119.
Perera MJ Chirinos DA Brintz CE Schneiderman N Daviglus M Talavera GA et al Body mass of US hispanics/latinos from the hispanic community health study/study of latinos (HCHS/SOL): How do diet quality and sedentary time relate? Hisp Health Care Int (2020) 18(2):55–63. 10.1177/1540415319874809
120.
Reeske A Spallek J Razum O . Changes in smoking prevalence among first-and second-generation Turkish migrants in Germany–an analysis of the 2005 Microcensus. Int J Equity Health (2009) 8(1):26. 10.1186/1475-9276-8-26
121.
Reiss K Sauzet O Breckenkamp J Spallek J Razum O . How immigrants adapt their smoking behaviour: Comparative analysis among Turkish immigrants in Germany and The Netherlands. BMC Public Health (2014) 14(1):844. 10.1186/1471-2458-14-844
122.
Reiss K Schunck R Razum O . Effect of length of stay on smoking among Turkish and eastern European immigrants in Germany—Interpretation in the light of the smoking epidemic model and the acculturation theory. Int J Environ Res Public Health (2015) 12(12):15925–36. 10.3390/ijerph121215030
123.
Riosmena F Wong R Palloni A . Migration selection, protection, and acculturation in health: A binational perspective on older adults. Demography (2013) 50(3):1039–64. 10.1007/s13524-012-0178-9
124.
Riosmena F Kuhn R Jochem WC . Explaining the immigrant health advantage: Self-selection and protection in health-related factors among five major national-origin immigrant groups in the United States. Demography (2017) 54(1):175–200. 10.1007/s13524-016-0542-2
125.
Salama E Niemelä S Suvisaari J Laatikainen T Koponen P Castaneda AE et al The prevalence of substance use among Russian, Somali and Kurdish migrants in Finland: A population-based study. BMC Public Health (2018) 18(1):651. 10.1186/s12889-018-5564-9
126.
Salas-Wright CP Vaughn MG Goings TTC Córdova D Schwartz SJ . Substance use disorders among immigrants in the United States: A research update. Addict Behav (2018) 76:169–73. 10.1016/j.addbeh.2017.08.014
127.
Sewali B Harcourt N Everson-Rose SA Leduc RE Osman S Allen ML et al Prevalence of cardiovascular risk factors across six African Immigrant Groups in Minnesota. BMC Public Health (2015) 15(1):411. 10.1186/s12889-015-1740-3
128.
Singh GK Siahpush M . Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: An analysis of two national data bases. Hum Biol (2002) 74:83–109. 10.1353/hub.2002.0011
129.
So DW Wong FY . Alcohol, drugs, and substance use among Asian-American college students. J Psychoactive Drugs (2006) 38(1):35–42. 10.1080/02791072.2006.10399826
130.
Sofianou A Fung TT Tucker KL . Differences in diet pattern adherence by nativity and duration of US residence in the Mexican-American population. J Am Diet Assoc (2011) 111(10):1563–9. 10.1016/j.jada.2011.07.005
131.
Sordo L Indave B Vallejo F Belza M Sanz-Barbero B Rosales-Statkus M et al Effect of country-of-origin contextual factors and length of stay on immigrants’ substance use in Spain. Eur J Public Health (2015) 25(6):930–6. 10.1093/eurpub/ckv144
132.
Takeuchi DT Zane N Hong S Chae DH Gong F Gee GC et al Immigration-related factors and mental disorders among Asian Americans. Am J Public Health (2007) 97(1):84–90. 10.2105/AJPH.2006.088401
133.
Talegawkar SA Kandula NR Gadgil MD Desai D Kanaya AM . Dietary intakes among South Asian adults differ by length of residence in the USA. Public Health Nutr (2016) 19(2):348–55. 10.1017/S1368980015001512
134.
Taylor VM Yasui Y Tu S-P Neuhouser ML Li L Woodall E et al Heart disease prevention among Chinese immigrants. J Community Health (2007) 32(5):299–310. 10.1007/s10900-007-9057-5
135.
Terasaki D Saelens B . Length of residence and vehicle ownership in relation to physical activity among US immigrants. J Immigr Minor Health (2017) 19(2):484–8. 10.1007/s10903-016-0361-y
136.
Tortajada S Llorens N Castellano M Álvarez FJ Aleixandre-Benavent R Valderrama-Zurián JC et al Perception and consumption of alcohol among the immigrant population from Latin America in Valencia region (Spain). Subst Use Misuse (2010) 45(14):2567–78. 10.3109/10826080903550554
137.
Tran DT Jorm L Johnson M Bambrick H Lujic S . Effects of acculturation on lifestyle and health status among older Vietnam-born Australians. Asia Pac J Public Health (2015) 27(2):NP2259–NP74. 10.1177/1010539513491419
138.
Tremblay MS Bryan SN Pérez CE Ardern CI Katzmarzyk PT . Physical activity and immigrant status: Evidence from the Canadian community health survey.Can J Public Health (2006) 97(4):277–82. 10.1007/bf03405603
139.
Tseng M Fang CY . Stress is associated with unfavorable patterns of dietary intake among female Chinese immigrants. Ann Behav Med (2011) 41(3):324–32. 10.1007/s12160-010-9259-4
140.
Tseng M Wright DJ Fang CY . Acculturation and dietary change among Chinese immigrant women in the United States. J Immigr Minor Health (2015) 17(2):400–7. 10.1007/s10903-014-0118-4
141.
Van Hook J Quirós S Dondero M Altman CE . Healthy eating among Mexican Immigrants: Migration in childhood and time in the United States. J Health Soc Behav (2018) 59(3):391–410. 10.1177/0022146518788869
142.
Vargas-Bustamante A . Menu labeling perception and health behaviors among immigrant and US born minority populations: Assessment in two Los Angeles public markets. Salud Publica Mex (2013) 55:s515–s22. 10.21149/spm.v55s4.5157
143.
Vega WA Sribney W . Parental risk factors and social assimilation in alcohol dependence of Mexican Americans. J Stud Alcohol (2003) 64(2):167–75. 10.15288/jsa.2003.64.167
144.
Wong J Wong S . Cardiovascular health of immigrant women: Implications for evidence‐based practice. Clin Gov (2003) 8:112–22. 10.1108/14777270310471595
145.
Wong SS Dixon LB Gilbride JA Chin WW Kwan TW . Diet, physical activity, and cardiovascular disease risk factors among older Chinese Americans living in New York City. J Community Health (2011) 36(3):446–55. 10.1007/s10900-010-9326-6
146.
Yang F-J . Is childhood migration a mental health risk? Exploring health behaviors and psychosocial resources as pathways using the cross-sectional Canadian community health survey. Soc Sci Res (2019) 83:102303. 10.1016/j.ssresearch.2019.04.016
147.
Yang K Laffrey SC Stuifbergen A Im E-O May K Kouzekanani K et al Leisure-time physical activity among midlife Korean immigrant women in the US. J Immigr Minor Health (2007) 9(4):291–8. 10.1007/s10903-007-9039-9
148.
Zan H Fan JX . Reporting more but moving less? The complex relationship between acculturation and physical activity among US adults. Am J Health Promot (2018) 32(2):446–52. 10.1177/0890117117716415
149.
Corral I Landrine H . Acculturation and ethnic-minority health behavior: A test of the operant model.Health Psychol (2008) 27(6):737–45. 10.1037/0278-6133.27.6.737
150.
Landrine H Klonoff EA . Culture change and ethnic-minority health behavior: An operant theory of acculturation.J Behav Med (2004) 27(6):527–55. 10.1007/s10865-004-0002-0
151.
Katikireddi SV Higgins M Smith KE Williams G . Health inequalities: The need to move beyond bad behaviours. J Epidemiol Community Health (2013) 67(9):715–6. 10.1136/jech-2012-202064
152.
Pearlin lI Schieman S Fazio EM Meersman SC . Stress, health, and the life course: Some conceptual perspectives. J Health Soc Behav (2005) 46(2):205–19. 10.1177/002214650504600206
153.
Pascoe EA Smart Richman L . Perceived discrimination and health: A meta-analytic review. Psychol Bull (2009) 135(4):531–54. 10.1037/a0016059
154.
Marmot M . Social determinants of health inequalities. Lancet (2005) 19-25(365):1099–104. 10.1016/S0140-6736(05)71146-6
155.
Juárez S Honkaniemi H Dunlavy A Aldridge R Barreto M Katikireddi S et al Effects of non-health-targeted policies on migrant health: A systematic review and meta-analysis. Lancet Glob Health (2019) 7(4):e420–e35. 10.1016/S2214-109X(18)30560-6
156.
Pablos-Mendez A . Mortality among hispanics. JAMA: J Am Med Assoc (1994) 271(16):1237. 10.1001/jama.271.16.1237b
Summary
Keywords
alcohol, diet, physical activity (PA), smoking, substance use, health risk behaviours, length of stay, immigrants
Citation
Juárez SP, Honkaniemi H, Gustafsson N-K, Rostila M and Berg L (2022) Health Risk Behaviours by Immigrants’ Duration of Residence: A Systematic Review and Meta-Analysis. Int J Public Health 67:1604437. doi: 10.3389/ijph.2022.1604437
Received
27 August 2021
Accepted
28 June 2022
Published
05 August 2022
Volume
67 - 2022
Edited by
Olaf Von Dem Knesebeck, University Medical Center Hamburg-Eppendorf, Germany
Reviewed by
Nico Vonneilich, University Medical Center Hamburg-Eppendorf, Germany
Updates
Copyright
© 2022 Juárez, Honkaniemi, Gustafsson, Rostila and Berg.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sol P. Juárez, sol.juarez@su.se
†These authors share first authorship
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.