Abstract
Objectives: This study aimed to investigate the risk of stillbirth, perinatal and neonatal mortality in immigrant women compared to native-origin women in host countries.
Methods: A systematic literature review and meta-analysis was conducted. Relevant studies were identified using a thorough literature search and their quality was appraised. The analysis of heterogeneous data was carried out using the random effects model and publication bias was assessed using the Harbord-test. Also, the pooled odds ratio of events was calculated through the DerSimonian and Laird, and inverse variance methods.
Results: In the search process 45 studies were retrieved consisting of 8,419,435 immigrant women and 40,113,869 native-origin women. The risk of stillbirth (Pooled OR = 1.35, 95% CI = 1.22–1.50), perinatal mortality (Pooled OR = 1.50, 95% CI = 1.35–1.68), and neonatal mortality (Pooled OR = 1.09, 95% CI = 1.00–1.19) in the immigrant women were significantly higher than the native-origin women in host countries. According to the sensitivity analyses, all results were highly consistent with the main data analysis results.
Conclusion: The immigrant women compared to the native-origin women had the higher risks of stillbirth, perinatal and neonatal mortality. Healthcare providers and policy makers should improve the provision of maternal and neonatal healthcare for the immigrant population.
Introduction
The number of immigrant people across the globe has increased over the past decades and now is at an all-time high [1]. The impact of immigration on people health is far-reaching as immigrants are particularly vulnerable to health inequalities [2]. The immigrant population mostly consists of women in the childbearing age that experience the negative effects of immigration on their maternal and neonatal health [3].
Perinatal mortality has been defined as the number of fetal and early neonatal deaths for every 1,000 births. Stillbirth refers to a baby born dead after the 28th week of gestation and neonatal mortality is considered death in the first 28 days of life. As important indicators of the quality of antenatal, obstetric, and perinatal care, they reflect the overall health status in the community [4]. Also, they are linked to the effective maternal and neonatal care throughout the continuum of care initiated from the pregestational period until postpartum [5–7].
Studies on the risk of perinatal mortality among the newborns of immigrant women have reported controversial results. Some studies show that perinatal mortality among these newborns generally occur more frequently than the newborns of women in host countries [8–20]. Other studies show that immigrant women have the same or even less perinatal mortality than native-origin women [4, 21–26]. Given the lack of conclusive evidence, this systemic review and meta-analysis aimed to investigate the risk stillbirth, and perinatal and neonatal mortality in immigrant women compared to native-origin women in host countries.
Methods
The systematic review was conducted in accordance with the Cochrane methodology for systematic review and meta-analysis. The whole review process was informed by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [27]. The following PICO (Population, Intervention or exposure, Comparison, Outcome) elements were applied as inclusion criteria to this systematic review: P: all women with the history of pregnancy and their neonates; I: international immigration; C: native-origin women; O: perinatal death, still birth, and neonatal mortality.
Eligibility Criteria
Analytic observational studies with cross-sectional, case-control, and cohort designs that addressed the prevalence or risk of at least one of stillbirth, perinatal, and neonatal mortality incidents in immigrant women were considered. Other inclusion criteria were studies published in English language and should present data on immigrant women who crossed international borders compared to native-origin women. Also, they should report the number or prevalence incident of the outcomes of interest in both groups. Movement of women internally within national boundaries led to the exclusion of studies. Also, non-original studies including reviews, commentaries, editorials, letters, meeting abstracts, case reports, and conference proceedings were excluded, because they did not provide accurate and clear data on research variables. Duplicated studies, those with a focus on specific minor populations such as adolescents, and with incomplete data were excluded. No restrictions were applied based on the immigration origin, status, or length of time passed in the host country.
Search Strategy
A thorough literature search was carried out on the databases of PubMed (including MEDLINE), Web of Science, and Scopus until September 2020. To maximize the identification of eligible studies, a manual search in the references lists of selected studies and relevant reviews was performed. Search keywords consisting of free-text and MeSH terms were combined using the Boolean method and were utilized to conduct the search: (migration OR immigration OR migrant OR immigrant OR emigrant OR asylum seeker OR asylum seeking OR asylum OR refugee) AND (stillbirth OR still birth OR stillborn OR fetal death OR perinatal mortality OR perinatal death OR neonatal mortality OR neonatal death OR adverse pregnancy outcomes OR pregnancy outcomes OR pregnancy complications OR adverse neonatal outcome).
Study Selection and Data Extraction
The screening of titles, abstracts, and full texts of studies according to eligibility criteria was performed independently by two authors. A third reviewer was consulted in case of disagreement between two data extractors. Discrepancy was resolved by consensus. The following data were extracted from eligible studies and were exported to a table: design; country; publication year; study period; sample size; population characteristics including age and body mass index (BMI); outcome measurements including the number and prevalence of outcomes of interest. Both raw (unadjusted) and adjusted odd ratio/relative risk/hazard ratio were recorded. For the prevention of extraction errors, the original studies’ data and those data used in the meta-analysis were compared together.
Terms Definition
The immigrant population has been defined as “any person moving across an international border, regardless of the person’s legal status; whether it was voluntary or involuntary and what causes for the movement were; or what the length of stay was” [28]. It constitutes a heterogeneous group including refugees, asylum seekers, illegal and undocumented immigrants, economic and transient immigrants.
The native-origin population has been defined as any person who has two parents born in the host country. Perinatal mortality is defined as intrauterine death at or after 22 weeks of gestational age or any early neonatal death occurring within 7 days after birth [29]. Stillbirth is fetal death at ≥ 28 weeks of gestation or weight ≥1,000 g. If both these criteria are unknown, crown-heel length ≥35 cm is considered [30]. Neonatal mortality is defined as the death of a live born infant, regardless of gestational age at birth, within the first 28 completed days of life [31].
Quality Appraisal
Selected studies were critically appraised in terms of the methodological structure and presentation of results using the modified Newcastle–Ottawa Quality Assessment Scale [32]. Two authors who were blind to the study’s author and institution, and the journal’s title evaluated the quality of each study independently. Studies with scores above 6 were considered high quality, 4–6 moderate quality, and less than 4 low quality.
Patient and Public Involvement Statement
Patients and the public were not involved in this research. Therefore, no ethical permission was required to be obtained.
Statistical Analysis
The software package STATA (version 14; STATA Inc., College Station, TX, United States) was used for statistical data analysis. Heterogeneity was evaluated using I2 index, and p < 0.05 was interpreted as heterogeneity. Heterogeneous and non-heterogeneous results were analyzed using the random/fixed effects models and the pooled effect was calculated. Publication bias was assessed using the Harbord test. The DerSimonian and Laird inverse variance method was used to calculate the pooled odds ratio of incidents (OR, 95% CI). In addition, sensitivity analysis was run to investigate the influence of each individual study on the overall meta-analysis summary estimate. The graph of the influence analysis’ result in which the meta-analysis was re-estimated omitting each study in turn was presented. p < 0.05 was set as the statistical significance level.
Results
Characteristics of Studies
The search process yielded 606 studies (Figure 1). A total of 117 duplicate articles were deleted. Using priori selection criteria, 387 studies were excluded based on the screening of titles and abstracts. Therefore, 102 studies were selected for full text appraisal, but 57 studies were further excluded. Finally, 45 studies were included in the systematic review and meta-analysis involving 8,419,435 immigrant women and 40,113,869 native-origin women. The main characteristics of the selected studies have been outlined in Table 1. The studies were conducted in Europe (n = 37; Spain [23, 33], Finland [25, 34], Israel [9, 15], Turkey [22, 24, 35–38], Sweden [12, 13, 39, 40], Norway [16, 19, 41–45], Belgium [17, 18, 45, 46], United Kingdom [45, 47], Netherlands [20, 45], Denmark [45, 48], Switzerland [45], Austria [45], Germany [45] and Italy [49]), America (n = 8; Canada [21, 26, 50], USA [51–53] and Argentina [4, 54]), Australia (n = 5) [8, 10, 11, 14, 55]), and Taiwan (n = 1) [56, 57]. The results of quality appraisals of the included studies have been summarized in Supplementary Tables S1, S2. A total of 38 (84%) studies had high [4, 8–19, 21, 23, 25, 26, 33–36, 39–48, 50–53, 55–57], 7 (16%) had moderate quality [20, 22, 24, 37, 38, 49, 54], and no study had low quality.
FIGURE 1
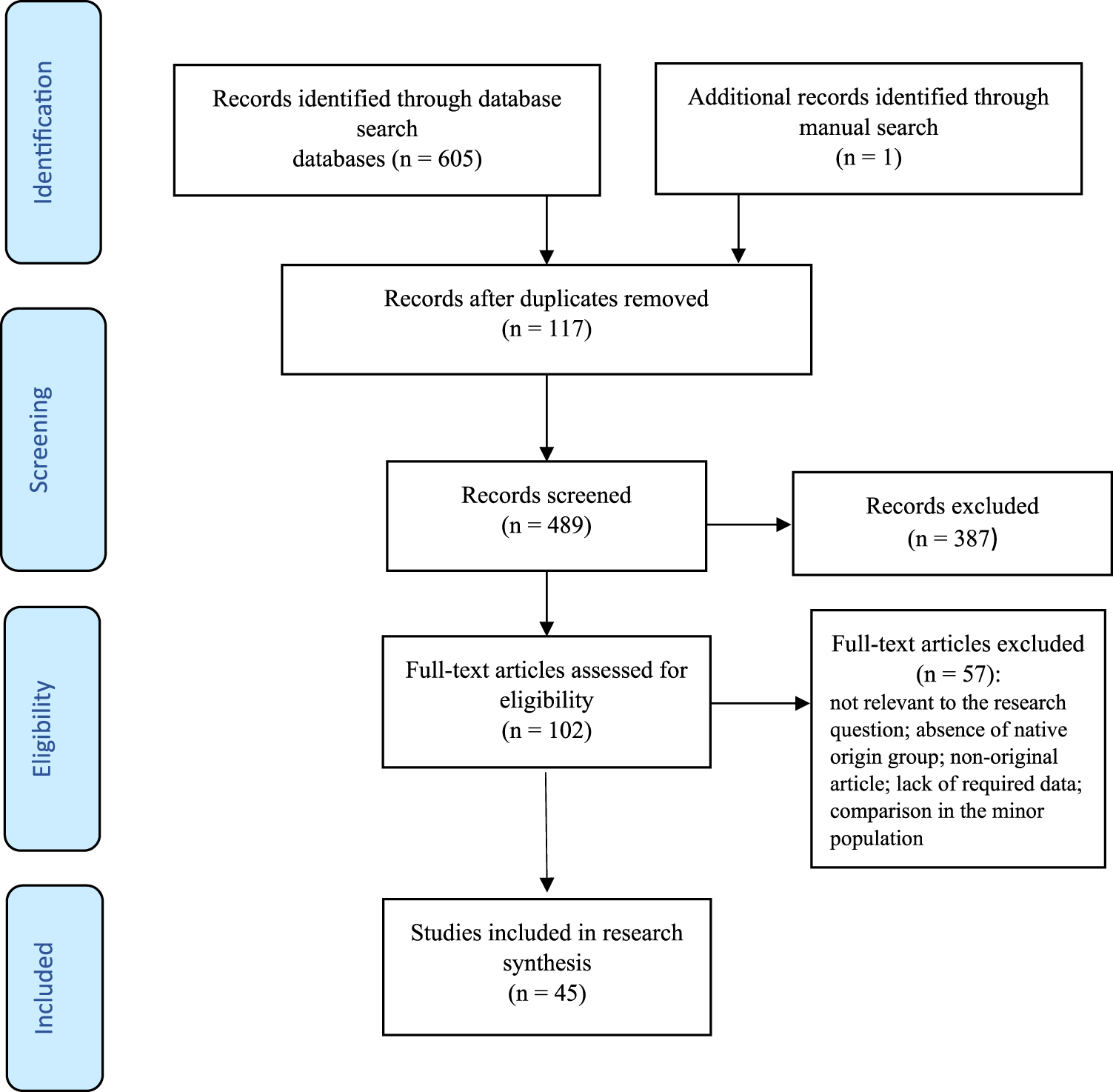
Flowchart of the search process. (Risk of stillbirth, perinatal and neonatal mortality in immigrant women, worldwide, 2021).
TABLE 1
| First author, year | Data sources | Year of data collection | Host country | Native origin group sample size | Origin of immigrants | Immigrant group sample size |
|---|---|---|---|---|---|---|
| Auger, 2020 | Birth and stillbirth registry | 1981–2015 | Canada | 2,623,245 | Arab women | 72,677 |
| Barona-Vilar, 2014 | Perinatal mortality registry | 2005–2008 | Spain | 162,043 | Outside Spain | 40,834 |
| Bastola, 2020 | Medical birth register of Finland | 2004–2014 | Finland | 350,485 | 1. Western EU | 1. 2,290 |
| 2. Eastern EU | 2. 2,566 | |||||
| 3. Russia | 3. 11,994 | |||||
| 4. South Asia | 4. 1,904 | |||||
| 5. East Asia | 5. 4,948 | |||||
| 6. Sub‐Saharan Africa | 6. 3,548 | |||||
| 7. Middle East | 7. 3,465 | |||||
| 8. Latin America | 8. 739 | |||||
| Belihu, 2016 | Victorian routine perinatal data registry | 1999–2007 | Australia | 427,755 | 1. Eritrea | 1. 453 |
| 2. Ethiopia | 2. 1,094 | |||||
| 3. Somalia | 3. 1,861 | |||||
| 4. Sudan | 4. 1,404 | |||||
| Burton, 1999 | New South Wales midwives data collection | 1990–1993 | Australia | 256,843 | Pacific Islands | 5,034 |
| Calderon-Margalit, 2015 | One medical center | 2002–2009 | Israel | 27,307 | Ethiopia | 1,319 |
| Çelik, 2019 | One hospital | 2013–2016 | Turkey | 48,506 | 1. Syria | 1. 718 |
| 2. Iraq | 2. 136 | |||||
| Choi, 2019 | Australian national perinatal data collection | 2004–2013 | Australia | 1,735,724 | 1. Europe | 1. 206,999 |
| 2. Middle East and North Africa | 2. 69,065 | |||||
| 3. China | 3. 47,855 | |||||
| 4. India | 4. 48,428 | |||||
| 5. Philippines | 5. 25,827 | |||||
| 6. Vietnam | 6. 31,729 | |||||
| 7. Asia except middle east | 7. 117,417 | |||||
| 8. Latin America | 8. 14,475 | |||||
| 9. Africa | 9. 39,459 | |||||
| Col Madendag, 2019 | One hospital database | 2018–2019 | Turkey | 4,271 | Syria | 2,040 |
| Dahlen, 2013 | New South Wales midwives data collection | 2000–2008 | Australia | 496,668 | 1. New Zealand | 1. 17,293 |
| 2. England | 2. 15,218 | |||||
| 3. China | 3. 14,526 | |||||
| 4. Vietnam | 4. 13,835 | |||||
| 5. Lebanon | 5. 12,451 | |||||
| 6. Philippines | 6. 9,684 | |||||
| 7. India | 7. 8,301 | |||||
| 8. Other | 8. 103,761 | |||||
| Ekéus, 2011 | Swedish medical birth register, income and population registers | 1992–2005 | Sweden | 1,094,146 | 1. Western Europe | 1. 48,930 |
| 2. Eastern Europe | 2. 47,858 | |||||
| 3. Asia | 3. 22,748 | |||||
| 4. Latin | 4. 13,151 | |||||
| 5. Middle East Asia | 5. 65,937 | |||||
| 6. Africa | 6. 12,062 | |||||
| 7. Somalia | 7. 9,146 | |||||
| Erenel, 2017 | One hospital | 2013–2016 | Turkey | 300 | Syria | 300 |
| Essén, 2000 | Malmö database, Swedish medical birth register | 1990–1995 | Sweden | 4,855 | All foreign origins | 356 |
| Fuster, 2014 | Spanish national institute of statistics | 2007–2012 | Spain | 1,874,913 | All foreign origins | 412,906 |
| Gillet, 2014 | Study center for perinatal epidemiology Belgian civil birth registration system | 2204–2008 | Belgium | 261,566 | 1. Low-income countries | 1. 8,066 |
| 2. Middle-income countries | 2. 41,985 | |||||
| 3. High-income countries | 3. 14,549 | |||||
| Gould, 2003 | California linked infant birth/death certificate files | 1995–1997 | 1. USA, white | 1. 506,365 | 1. India | 1. 12,899 |
| 2. USA, black | 2. 104,888 | 2. Mexico | 2. 433,825 | |||
| Hsieh, 2011 | Birth certificate registration data | 1998–2003 | Taiwan | 1,321,770 | Not mentioned | 93,161 |
| Johnson, 2005 | Birth certificate data | 1993–2001 | 1. USA, black | 1. 2,384 | Somali | 579 |
| 2. USA, white | 2. 2,453 | |||||
| Kanmaz, 2019 | One hospital | 2013–2016 | Turkey | 12,198 | Syria | 4,802 |
| Kiyak, 2020 | One hospital | 2016–2017 | Turkey | 940 | Syria | 616 |
| Liu, 2019 | Swedish pregnancy register | 2014–2017 | Sweden | 254,973 | Not mentioned | 31,897 |
| Liu, 2008 | Birth certificates | 2002–2007 | Taiwan | 27,077 | 1. Mainland China | 1. 1,483 |
| 2. Indonesia | 2. 1,129 | |||||
| 3. Vietnam | 3. 1,081 | |||||
| Lubotzky-Gete, 2017 | One hospital | 1998–2011 | Israel | 63,405 | 1. Ethiopia | 1. 1,667 |
| 2. Former Soviet Union | 2. 12,920 | |||||
| Madan, 2006 | Birth certificates, perinatal mortality data file | 1995–2000 | US-born white | 4,005,671 | 1. Asian-Indian | 1. 76,618 |
| 2. Mexico | 2. 1,408,797 | |||||
| Malin, 2009 | Finnish medical birth register, statistics Finland | 1999–2001 | Finland | 158,469 | 1. Nordic | 1. 475 |
| 2. Western EU | 2. 400 | |||||
| 3. Eastern Europe | 3. 597 | |||||
| 4. Former Soviet Union, Russia | 4. 1,770 | |||||
| 5. Baltic | 5. 496 | |||||
| 6. Middle East, North-Africa | 6. 310 | |||||
| 7. South Asia | 7. 176 | |||||
| 8. China | 8. 135 | |||||
| 9. Iran, Iraq, Afghanistan | 9. 428 | |||||
| 10. Southeast Asia | 10. 336 | |||||
| 11. Vietnam | 11. 302 | |||||
| 12. Africa, excl. Somalia, North Africa | 12. 169 | |||||
| 13. Somalia | 13. 817 | |||||
| 14. Latin America and Caribbean | 14. 121 | |||||
| Mozooni, 2020 | Perinatal, birth, death, hospital, birth defects registrations | 2005–2013 | Australia | 172,571 | 1. White | 1. 48,546 |
| 2. Asia | 2. 18,212 | |||||
| 3. India | 3. 5,503 | |||||
| 4. Africa | 4. 4,155 | |||||
| 5. Māori | 5. 2,941 | |||||
| 6. Other | 6. 9,038 | |||||
| Naimy, 2013 | Medical birth registry of Norway, Norwegian central person registry | 1986–2005 | Norway | 1062744 | 1. Pakistan | 1. 11,351 |
| 2. Vietnam | 2. 6,169 | |||||
| 3. Somalia | 3. 5,410 | |||||
| 4. Sri Lanka | 4. 4,933 | |||||
| 5. Philippines | 5. 4,662 | |||||
| 6. Iraq | 6. 3,829 | |||||
| 7. Thailand | 7. 3,204 | |||||
| 8. Afghanistan | 8. 665 | |||||
| Opondo, 2020 | Statutory birth and death registration data for England and Wales, National Health Service Numbers for Babies (NN4B) birth notifications system, office for national statistics | 2006–2012 | United Kingdom | 3,009,231 | 1. White (other) | 1. 340,526 |
| 2. India | 2. 132,651 | |||||
| 3. Pakistan | 3. 180,651 | |||||
| 4. Bangladesh | 4. 62,948 | |||||
| 5. Black Caribbean | 5. 47,505 | |||||
| 6. Black Africa | 6. 154,076 | |||||
| 7. Mixed or other | 7. 419,970 | |||||
| 8. Not mentioned | 8. 287,756 | |||||
| Ozel, 2018 | One hospital | 2015 | Turkey | 576 | Syria | 576 |
| Racape, 2013 | Birth and death certificates | 1998–2008 | Belgium | 39,893 | 1. Morocco | 1. 12,371 |
| 2. Moroccan naturalised | 2. 15,108 | |||||
| 3. Sub-Sahara | 3. 6,322 | |||||
| 4. Sub-Saharan naturalised | 4. 3,070 | |||||
| 5. Turkey | 5. 3,185 | |||||
| 6. Turkey naturalised | 6. 3,673 | |||||
| Racape, 2016 | Birth and death certificates | 1998–2010 | Belgium | 1,029,471 | 1. Western Europe | 1. 98,189 |
| 2. Western Europe naturalized Belgian | 2. 34,701 | |||||
| 3. Turkey | 3. 20,451 | |||||
| 4. Turkey naturalized Belgian | 4. 21,878 | |||||
| 5. Maghreb | 5. 51,224 | |||||
| 6. Maghreb naturalized Belgian | 6. 46,681 | |||||
| 7. Sub-Saharan Africa | 7. 26,621 | |||||
| 8. Sub-Saharan Africa naturalized Belgian | 8. 11,420 | |||||
| 9. Eastern Europe | 9. 17,420 | |||||
| 10. Eastern Europe naturalized Belgian | 10. 5,412 | |||||
| Raimondi, 2013 | Public maternity hospital | 2009 | Argentine | 1,000 | Not mentioned | 1,000 |
| Råssjö, 2013 | Records of antenatal and obstetric care | 2001–2009 | Sweden | 513 | Somali | 258 |
| Sørbye, 2014 | Statistic Norway, medical birth registry of Norway | 1995–2010 | Norway | 712,430 | Pakistan | 10,615 |
| Vang, 2016 | Birth-infant death records | 1990–2005 | Canada | 2,856,394 | 1. United States | 1. 41,601 |
| 2. North Africa | 2. 17,991 | |||||
| 3. Sub-Saharan Africa | 3. 24,339 | |||||
| 4. Haiti | 4. 20,057 | |||||
| 5. Non-Spanish Caribbean | 5. 10,499 | |||||
| 6. Latin America | 6. 38,702 | |||||
| 7. Pakistan | 7. 7,500 | |||||
| 8. South Asia | 8. 68,558 | |||||
| 9. Central/West Asia | 9. 27,491 | |||||
| 10. East/SE Asia | 10. 138,024 | |||||
| 11. Europe | 11. 108,515 | |||||
| 12. Rest of the world | 12. 10,970 | |||||
| Vangen, 2002 | Medical birth registry of Norway | 1986–1998 | Norway | 702,192 | Somalia | 1,733 |
| Vangen, 2000 | Medical birth registry of Norway | 1986–19958 | Norway | 535,600 | 1. Turkey, Morocco | 1. 2,758 |
| 2. Pakistan | 2. 4,929 | |||||
| 3. India, Sri Lanka | 3. 2,643 | |||||
| 4. Vietnam | 4. 2,704 | |||||
| 5. Philippines | 5. 1,985 | |||||
| 6. Horn of Africa | 6. 1,406 | |||||
| 7. Chile Brazil | 7. 1,466 | |||||
| Verschuuren, 2020 | One midwifery practice, hospital databases | 2012–2016 | Netherlands | 2,323 | 1. Eritrea | 1. 65 |
| 2. Syria | 2. 75 | |||||
| 3. Middle east | 3. 75 | |||||
| 4. Sub-Saharan Africa | 4. 50 | |||||
| 5. Eastern Europe | 5. 43 | |||||
| 6. Other | 6. 18 | |||||
| Vetter, 2013 | 12 public hospitals | 2008 | Argentine | 9,155 | Not mentioned | 1,715 |
| Vik, 2019 | Medical birth registry of Norway and statistics Norway | 1990–2013 | Norway | 1,136,637 | Central Europe, Eastern Europe, Central Asia, Latin America, Caribbean, North Africa, Middle East, South Asia, Sub-Saharan Africa, Southeast Asia, East Asia, Oceania, other | 195,725 |
| Vik, 2020 | Medical birth registry of Norway and statistics Norway | 1990–2016 | Norway | 66,006 | Not mentioned | 30,062 |
| Villadsen, 2010 | Birth registries or surveys | 1990–2005 | 1. Belgium | 1. 238,233 | Turkey | 8,717 |
| 2. Denmark | 2. 812,305 | |||||
| 3. Norway | 3. 675,387 | |||||
| 4. Sweden | 4. 1,344,237 | |||||
| 5. Switzerland | 5. 900,875 | |||||
| 6. Austria | 6. 408,695 | |||||
| 7. United Kingdom | 7. 1,037,348 | |||||
| 8. Germany | 8. 1,296,798 | |||||
| 9. Netherland | 9. 935,858 | |||||
| Villadsen, 2009 | Danish medical birth registry, causes of death registry and socioeconomic and demographic data | 1981–2003 | Denmark | 1,278,539 | 1. Turkey | 1. 22,717 |
| 2. Lebanon | 2. 9,280 | |||||
| 3. Pakistan | 3. 8,481 | |||||
| 4. Former Yugoslavia | 4. 8,020 | |||||
| 5. Somali | 5. 6,415 | |||||
| Wanigaratne, 2018 | IRCC-PRD, Ontario’s healthcare registry, abstract database, general’s vital statistics- death registry | 2002–2014 | Canada | 29,023 | Not mentioned | 29,023 |
| Zanconato, 2011 | One public hospital | 2005–2009 | Italy | 6,365 | 1. Central and Eastern Europe | 1. 1,001 |
| 2. South and East Asia | 2. 539 | |||||
| 3. Middle East and North Africa | 3. 460 | |||||
| 4. Sub-Saharan Africa | 4. 448 | |||||
| 5. Central and South America | 5. 213 |
Baseline characteristic of the studies’ participants. Risk of stillbirth, perinatal and neonatal mortality in immigrant women, worldwide, 2021.
Meta-Analysis of Outcomes
A total of 31 studies [4, 8–13, 20–23, 26, 33–41, 43–46, 48, 49, 51, 52, 55, 57] reported stillbirth in 12,232 out of 2,715,308 immigrant women and 72,100 out of 19,262,686 native-origin women. Although there were statistical significant heterogenicities in the studies (I-squared = 95.5%), no publication bias was found (Harbord test p value = 0.160). The pooled risk of stillbirth among immigrant women was 1.35 folds higher than that of native-origin women (Pooled OR = 1.35, 95% CI = 1.22–1.50) (Figure 2).
FIGURE 2
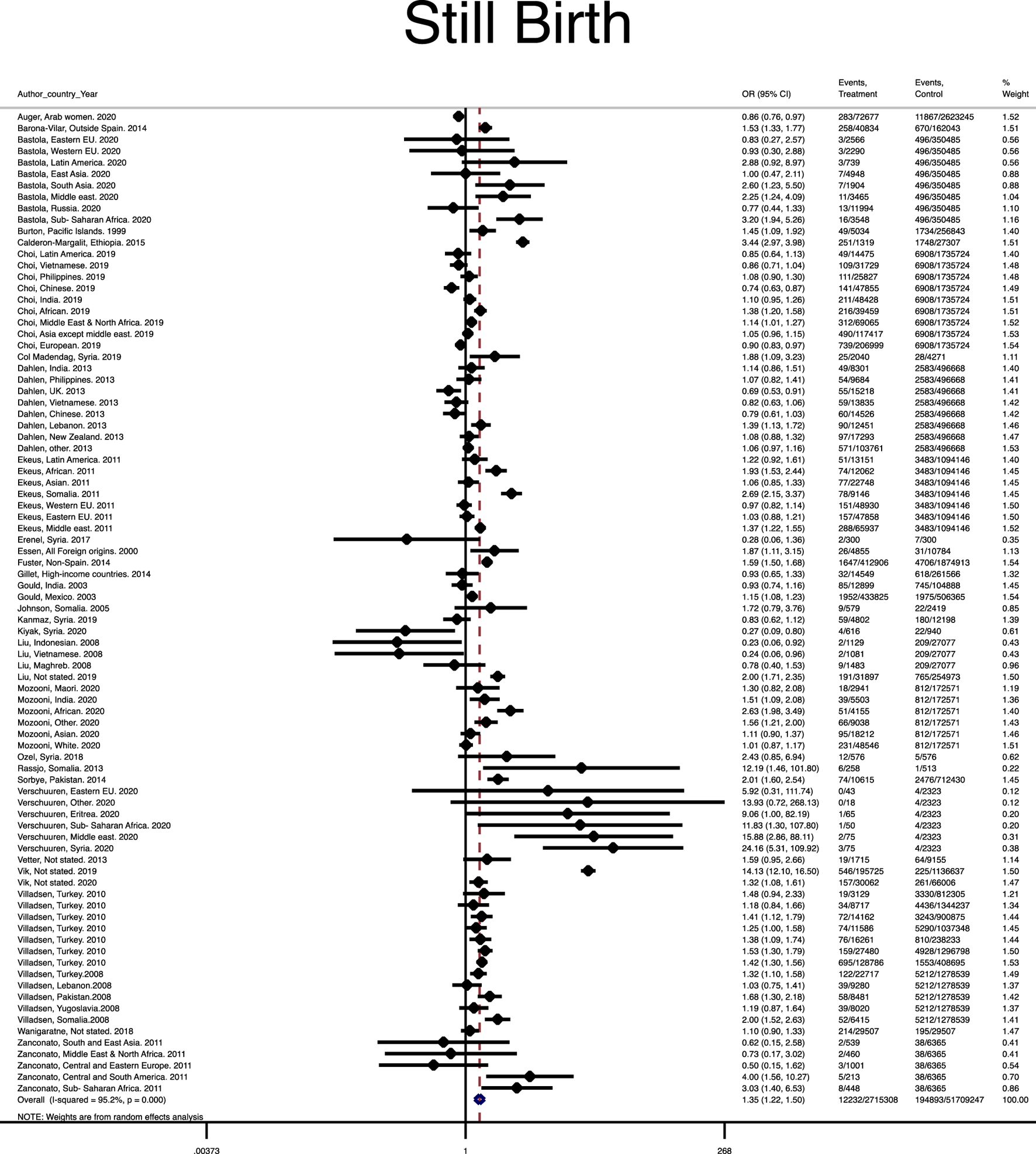
Forest plot of the pooled odds ratio of stillbirth. (Risk of stillbirth, perinatal and neonatal mortality in immigrant women, worldwide, 2021).
A total of 17 studies [4, 8, 10, 11, 26, 33, 34, 42, 43, 46, 47, 50–54, 56] reported the perinatal mortality among 4,399 out of 487,508 immigrant women and 30,838 out of 3,859,199 native-origin women. However, heterogeneity (I-squared = 87.1%) without publication bias (Harbord test p value = 0.340) was found across the studies. The pooled risk of perinatal mortality among immigrant women was significantly 1.5 folds higher than native-origin women (Pooled OR = 1.50, 95% CI = 1.35–1.68) (Figure 3).
FIGURE 3
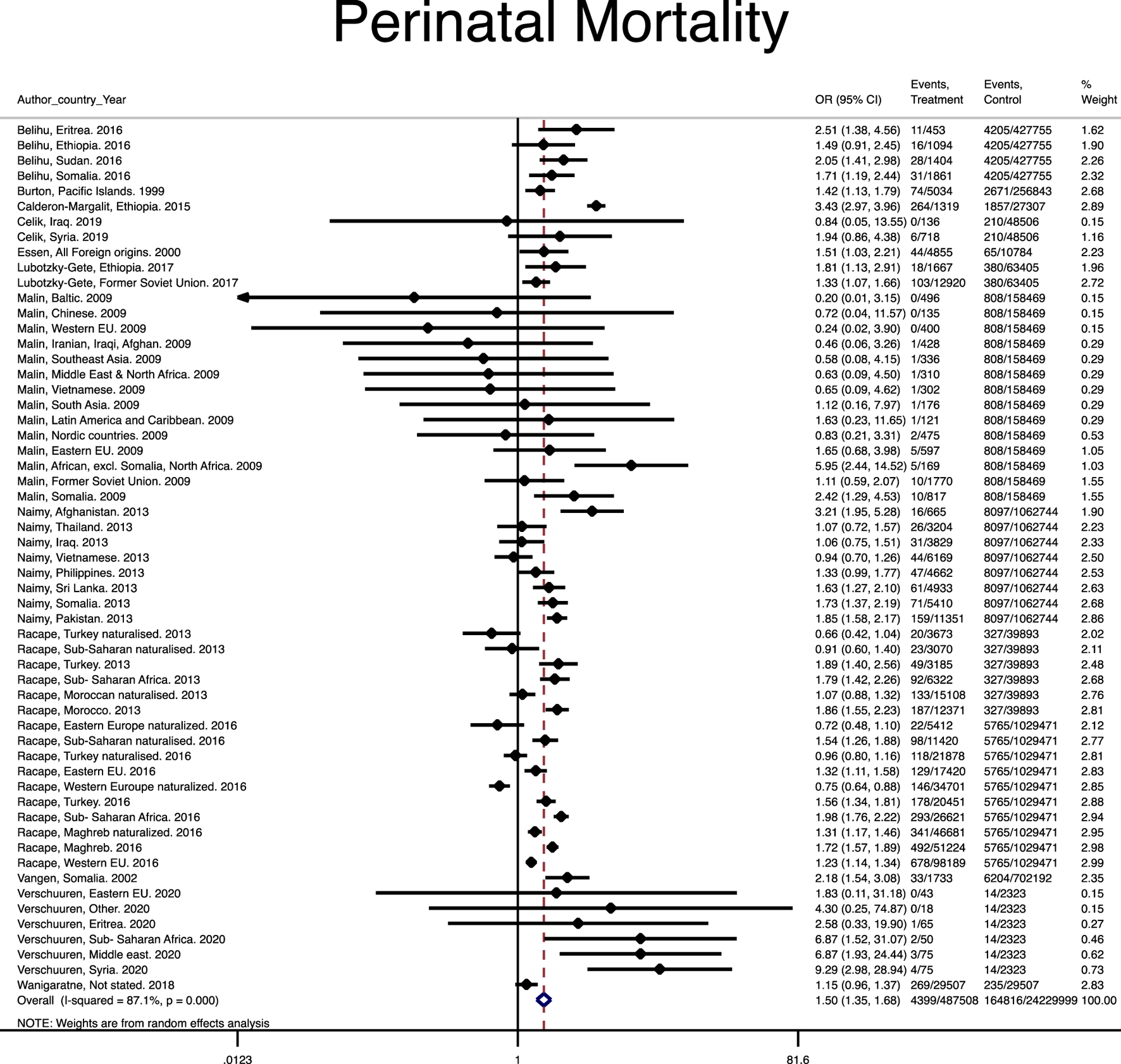
Forest plot of the pooled odds ratio of perinatal mortality. (Risk of stillbirth, perinatal and neonatal mortality in immigrant women, worldwide, 2021).
A total of 14 studies [8, 9, 13–20, 24–26, 48] reported neonatal mortality among 12,491 out of 5,216,619 immigrant women and 70,464 out of 16,991,984 native-origin women. Statistically significant heterogenicities (I-squared = 93.6%), without publication bias were found (Harbord test p value = 0.211) in the studies. Although immigrant women faced a greater risk of neonatal morbidity compared to native-origin women, its risk was not statistically significant (Pooled OR = 1.09, 95% CI = 1.00–1.19) (Figure 4).
FIGURE 4
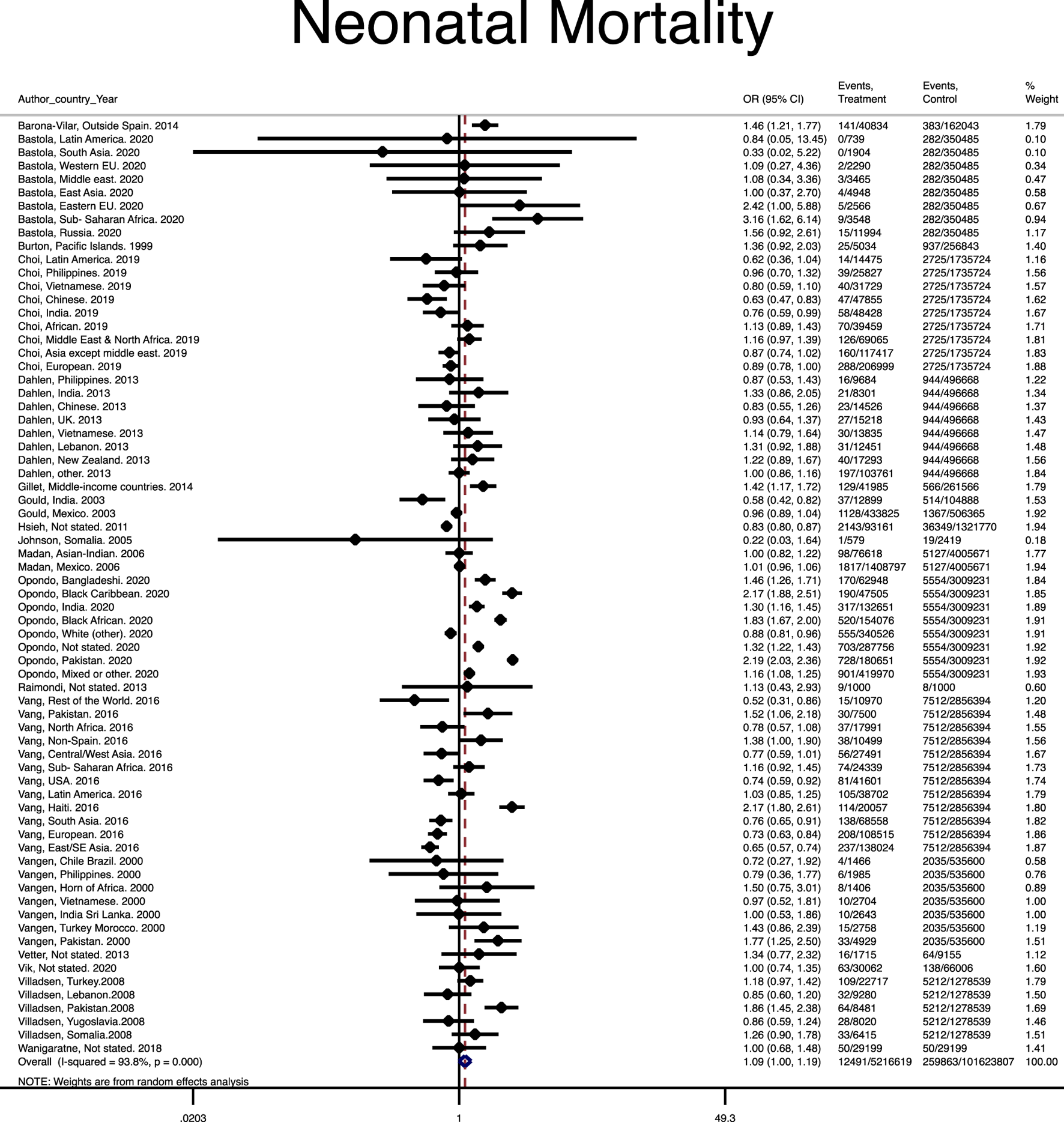
Forest plot of the pooled odds ratio of neonatal mortality. (Risk of stillbirth, perinatal and neonatal mortality in immigrant women, worldwide, 2021).
Sensitivity Analysis
Sensitivity analysis was performed to show the influence of each individual study on the overall meta-analyses’ summary estimates. All results were highly consistent with the main data analysis’ results and no substantial modification of the estimates of change was found after the exclusion of any individual study (Supplementary Figures S1A–C).
Discussion
The results of this systematic review and meta-analysis revealed that the risk of stillbirth, perinatal and neonatal mortality increased among immigrant women compare to native-origin women in host countries.
Despite advances in antenatal and intrapartum care, perinatal mortality continues to be a major burden on the healthcare system. It can have devastating impacts on parents because of its unexpected nature [58, 59]. Adverse outcomes are multifactorial with a number of issues appearing to coalesce to immigrant women. Our review showed that immigrant women represented a high-risk group for stillbirth and perinatal mortality, which needed special care and attention during pregnancy and childbirth. Maternal background factors cause poorer outcomes in immigrant women. These women have medical problems such as infectious diseases or female genital mutilation leading to complications for themselves and their newborns [60–62]. Immigrant women have a poor access to maternity and public healthcare services in host countries [63–65], which can increase the risk of mortality among their newborns due to maternal disorders, unintended pregnancy, grand multiparity and teenage pregnancies [66, 67], preterm birth [68, 69], and undiagnosed congenital fetal anomalies [70, 71].
Health immigration policies of host countries and the immigrant legal status appear to influence their access to maternity health services. Those women without a legal resident permit are most vulnerable [67]. Gieles et al (2019) in a systematic review stated that positive integration policies without discrimination and adoption to the host-country nationality decreased perinatal mortality and morbidity among immigrant women and their newborns [69]. Additionally, late booking and delayed utilization of prenatal care with the presence of cultural and language barriers hinder appropriate access to healthcare services by immigrant women leading to higher mortality among their newborns compared to native-origin women [63]. Despite free access to maternity care in host countries, immigrant women usually utilize less antenatal care [72]. Poor communication between these women and healthcare providers in host countries such as unsupported and fearful interactions, being rude, discriminatory or insensitive to their specific needs can lead to late booking or delay in the use of maternity care services, which have negative impacts on prenatal care utilization [63, 73]. Cultural issues regarding prenatal or antenatal care as the facet of medicalization of childbirth care among immigrant women and different understanding of health and diseases hinder appropriate healthcare interventions in delivery, which are accompanied with higher stillbirth or perinatal mortality incidents in immigrant women [62].
It has been well documented that socio-economically vulnerable populations exhibit a higher mortality rate [74]. Immigrant women also experience a larger burden of poverty-related adverse circumstances such as the low social level, unhealthy lifestyle and behavior, malnutrition, which can play significant roles in poorer mortality outcomes among these women [73–75]. Consistently, perinatal mortality in immigrants from low-income settings of conflicting countries and having economic hardship generally occur more frequently that in the host population [67].
Although it is not most certainly observed in every immigrant group in every host nation, immigrants have often lower education levels and are more often single parents. Therefore, they have the risk factors of perinatal morbidity and stillbirth [76].
Studies mostly show that immigrant women are relatively younger than native-origin women [77–79], which may support the “healthy migrant” hypothesis, suggesting that the health of immigrants prior to immigration may be better than the health of the general population in both the sending and the receiving countries [80]. However, information on the higher rate of perinatal and neonatal mortality and stillbirth among immigrant women can be translated to health disparities that need more attention by healthcare organizations, regulatory bodies, educational institutions, and the society.
The results of our review should be interpreted with caution. Given the lack of data in the included studies, we could not adjust the legal status, reason for immigration, and length of the residence of immigrant women as well as background factors of immigrants and native-origin populations. Also, most data used in this review were based on population and health-related registers, which typically lacked detailed background data on women and their newborns. The frequent movement of immigrants usually leads to less complete registrations of their health status.
In conclusion, our review showed that immigrant women and their newborns had the higher risk of stillbirth, and perinatal and neonatal mortality compared to native-origin women. The result of sensitivity analyses supported the stability and robustness of our review results. Healthcare providers and policy makers should improve the provision of maternal and neonatal healthcare for the immigrant population.
Statements
Author Contributions
SB-G conceptualized the study and designed the protocol. SB-G, MV, and AM ran the search and oversaw screening, data extraction and assessment of bias. RB-Y conducted the statistical data analysis. SB-G drafted the manuscript, while IGK, PP, RB-Y, MHP, AM, and MV reviewed the draft and provided critical feedback. All authors read and approved the final manuscript. The corresponding author SB-G, as guarantor, accepts full responsibility for the finished article, has access to any data and controlled the decision to publish. The corresponding author SB-G attests that all listed authors meet the authorship criteria and that no others meeting the criteria have been omitted.
Acknowledgments
Nord University, Bodø, Norway covered the processing charge to this article.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2022.1604479/full#supplementary-material
References
1
Trost M Wanke EM Ohlendorf D Klingelhöfer D Braun M Bauer J et al Immigration: Analysis, Trends and Outlook on the Global Research Activity. J Glob Health (2018). 8:010414–4. 10.7189/jogh.08.010414
2
Gagnon AJ Zimbeck M Zeitlin J Alexander S Blondel B Buitendijk S et al Migration to Western Industrialised Countries and Perinatal Health: A Systematic Review. Soc Sci Med (2009). 69:934–46. 10.1016/j.socscimed.2009.06.027
3
United Nations High Commission for Refugees. Global Trends: Forced Displacement in 2016. Geneva: United Nations High Commissioner for Refugees (2017).
4
Vetter CL Gibbons L Bonotti A Klein K Belizán JM Althabe F . Obstetric Care for Resident Immigrant Women in Argentina Compared with Argentine Women. Int J Gynecol Obstet (2013). 122:140–4. 10.1016/j.ijgo.2013.03.018
5
Müller F Kleinert E Hillermann N Simmenroth A Hummers E Scharff AZ et al Disease Burden in a Large Cohort of Asylum Seekers and Refugees in Germany. J Glob Health (2021). 11:04002. 10.7189/jogh.11.04002
6
Willcox ML Price J Scott S Nicholson BD Stuart B Roberts NW et al Death Audits and Reviews for Reducing Maternal, Perinatal and Child Mortality. Cochrane Database Syst Rev (2020). 3:Cd012982. 10.1002/14651858.CD012982.pub2
7
Vogel J Souza J Mori R Morisaki N Lumbiganon P Laopaiboon M et al Maternal Complications and Perinatal Mortality: Findings of the World Health Organization Multicountry Survey on Maternal and Newborn Health. Bjog: Int J Obstet Gy (2014). 121:76–88. 10.1111/1471-0528.12633
8
Burton AJ Lancaster P . Obstetric Profiles and Perinatal Mortality Among Pacific Island Immigrants in New South Wales, 1990-93. Aust N Z J Public Health (1999). 23:179–84. 10.1111/j.1467-842x.1999.tb01231.x
9
Calderon-Margalit R Sherman D Manor O Kurzweil Y . Adverse Perinatal Outcomes Among Immigrant Women from Ethiopia in Israel. Birth (2015). 42:125–31. 10.1111/birt.12163
10
Choi SKY Henry A Hilder L Gordon A Jorm L Chambers GM . Adverse Perinatal Outcomes in Immigrants: A Ten‐year Population‐Based Observational Study and Assessment of Growth Charts. Paediatr Perinat Epidemiol (2019). 33:421–32. 10.1111/ppe.12583
11
Dahlen HG Schmied V Dennis C-L Thornton C . Rates of Obstetric Intervention During Birth and Selected Maternal and Perinatal Outcomes for Low Risk Women Born in Australia Compared to Those Born Overseas. BMC Pregnancy Childbirth (2013). 13:100. 10.1186/1471-2393-13-100
12
Ekéus C Cnattingius S Essén B Hjern A . Stillbirth Among Foreign-Born Women in Sweden. Eur J Public Health (2011). 21:788–92. 10.1093/eurpub/ckq200
13
Essén B Hanson BS Ostergren PO Lindquist PG Gudmundsson S . Increased Perinatal Mortality Among Sub-Saharan Immigrants in a City-Population in Sweden. Acta Obstet Gynecol Scand (2000). 79:737–43.
14
Belihu FB Davey M-A Small R . Perinatal Health Outcomes of East African Immigrant Populations in Victoria, Australia: A Population Based Study. BMC Pregnancy Childbirth (2016). 16:86. 10.1186/s12884-016-0886-z
15
Lubotzky-Gete S Shoham-Vardi I Sheiner E . Comparing Pregnancy Outcomes of Immigrants from Ethiopia and the Former Soviet Union to Israel, to Those of Native-Born Israelis. J Immigrant Minor Health (2017). 19:1296–303. 10.1007/s10903-016-0484-1
16
Naimy Z Grytten J Monkerud L Eskild A . Perinatal Mortality in Non-Western Migrants in Norway as Compared to Their Countries of Birth and to Norwegian Women. BMC Public Health (2013). 13:37. 10.1186/1471-2458-13-37
17
Racape J De Spiegelaere M Dramaix M Haelterman E Alexander S . Effect of Adopting Host-Country Nationality on Perinatal Mortality Rates and Causes Among Immigrants in Brussels. Eur J Obstet Gynecol Reprod Biol (2013). 168:145–50. 10.1016/j.ejogrb.2012.12.039
18
Racape J Schoenborn C Sow M Alexander S De Spiegelaere M . Are All Immigrant Mothers Really at Risk of Low Birth Weight and Perinatal Mortality? the Crucial Role of Socio-Economic Status. BMC Pregnancy Childbirth (2016). 16:75. 10.1186/s12884-016-0860-9
19
Vangen S Stoltenberg C Johansen REB Sundby J Stray-Pedersen B . Perinatal Complications Among Ethnic Somalis in Norway. Acta Obstet Gynecol Scand (2002). 81:317–22. 10.1034/j.1600-0412.2002.810407.x
20
Verschuuren AEH Postma IR Riksen ZM Nott RL Feijen-de Jong EI Stekelenburg J . Pregnancy Outcomes in Asylum Seekers in the North of the Netherlands: A Retrospective Documentary Analysis. BMC Pregnancy Childbirth (2020). 20:320. 10.1186/s12884-020-02985-x
21
Auger N Racape J Raynault M-F Bilodeau-Bertrand M Lee GE Janevic T . Stillbirth Among Arab Women in Canada, 1981-2015. Public Health Rep (2020). 135:245–52. 10.1177/0033354919900894
22
Erenel H Aydogan Mathyk B Sal V Ayhan I Karatas S Koc Bebek A . Clinical Characteristics and Pregnancy Outcomes of Syrian Refugees: A Case-Control Study in a Tertiary Care Hospital in Istanbul, Turkey. Arch Gynecol Obstet (2017). 295:45–50. 10.1007/s00404-016-4188-5
23
Fuster V Zuluaga P Román-Busto J . Stillbirth Incidence in Spain: A Comparison of Native and Recent Immigrant Mothers. DemRes (2014). 31:889–912. 10.4054/demres.2014.31.29
24
Çelik İH Arslan Z Ulubaş Işık D Tapisiz OL Mollamahmutoğlu L Bas AY et al Neonatal Outcomes in Syrian and Other Refugees Treated in a Tertiary Hospital in Turkey. Turk J Med Sci (2019). 49:815–20. 10.3906/sag-1806-86
25
Malin M Gissler M . Maternal Care and Birth Outcomes Among Ethnic Minority Women in Finland. BMC Public Health (2009). 9:84. 10.1186/1471-2458-9-84
26
Wanigaratne S Shakya Y Gagnon AJ Cole DC Rashid M Blake J et al Refugee Maternal and Perinatal Health in Ontario, Canada: A Retrospective Population-Based Study. BMJ Open (2018). 8:e018979. 10.1136/bmjopen-2017-018979
27
Moher D Liberati A Tetzlaff J Altman DG . Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA Statement. Bmj (2009). 339:b2535. 10.1136/bmj.b2535
28
International Organization for Migration (IOM). WORLD MIGRATION REPORT 2020 (2020). Available from: https://publications.iom.int/system/files/pdf/wmr_2020.pdf (Accessed 05 09, 2021).
29
World Health Organization. Neonatal and Perinatal Mortality: Country, Regional and Global Estimates (2006). Available from: http://apps.who.int/iris/bitstream/10665/43444/1/9241563206_eng.pdf (Accessed 05 24, 2021).
30
Lawn JE Blencowe H Pattinson R Cousens S Kumar R Ibiebele I et al Stillbirths: Where? When? Why? How to Make the Data Count? The Lancet (2011). 377:1448–63. 10.1016/s0140-6736(10)62187-3
31
Pathirana J Muñoz FM Abbing-Karahagopian V Bhat N Harris T Kapoor A et al Neonatal Death: Case Definition & Guidelines for Data Collection, Analysis, and Presentation of Immunization Safety Data. Vaccine (2016). 34:6027–37. 10.1016/j.vaccine.2016.03.040
32
Stang A . Critical Evaluation of the Newcastle-Ottawa Scale for the Assessment of the Quality of Nonrandomized Studies in Meta-Analyses. Eur J Epidemiol (2010). 25:603–5. 10.1007/s10654-010-9491-z
33
Barona-Vilar C López-Maside A Bosch-Sánchez S Pérez-Panadés J Melchor-Alós I Mas-Pons R et al Inequalities in Perinatal Mortality Rates Among Immigrant and Native Population in Spain, 2005-2008. J Immigrant Minor Health (2014). 16:1–6. 10.1007/s10903-012-9730-3
34
Bastola K Koponen P Gissler M Kinnunen TI . Differences in Caesarean Delivery and Neonatal Outcomes Among Women of Migrant Origin in Finland: A Population‐Based Study. Paediatr Perinat Epidemiol (2020). 34:12–20. 10.1111/ppe.12611
35
Col Madendag I Eraslan Sahin M Madendag Y Sahin E Demir MB Ozdemir F et al The Effect of Immigration on Adverse Perinatal Outcomes: Analysis of Experiences at a Turkish Tertiary Hospital. Biomed Res Int (2019). 2019:2326797. 10.1155/2019/2326797
36
Kanmaz AG İnan AH Beyan E Özgür S Budak A . Obstetric Outcomes of Syrian Refugees and Turkish Citizens. Arch Iran Med (2019). 22:482–8.
37
Kiyak H Gezer S Ozdemir C Gunkaya S Karacan T Gedikbasi A . Comparison of Delivery Characteristics and Early Obstetric Outcomes Between Turkish Women and Syrian Refugee Pregnancies. Niger J Clin Pract (2020). 23:12–7. 10.4103/njcp.njcp_10_18
38
Ozel S Yaman S Kansu-Celik H Hancerliogullari N Balci N Engin-Ustun Y . Obstetric Outcomes Among Syrian Refugees: A Comparative Study at a Tertiary Care Maternity Hospital in Turkey. Rev Bras Ginecol Obstet (2018). 40:673–9. 10.1055/s-0038-1673427
39
Liu C Ahlberg M Hjern A Stephansson O . Perinatal Health of Refugee and Asylum-Seeking Women in Sweden 2014-17: A Register-Based Cohort Study. Eur J Public Health (2019). 29:1048–55. 10.1093/eurpub/ckz120
40
Råssjö EB Byrskog U Samir R Klingberg-Allvin M . Somali Women's Use of Maternity Health Services and the Outcome of Their Pregnancies: a Descriptive Study Comparing Somali Immigrants with Native-Born Swedish Women. Sex Reprod Health (2013). 4:99–106. 10.1016/j.srhc.2013.06.001
41
Sørbye IK Stoltenberg C Sundby J Daltveit AK Vangen S . Stillbirth and Infant Death Among Generations of Pakistani Immigrant Descent: A Population-Based Study. Acta Obstet Gynecol Scand (2014). 93:168–74. 10.1111/aogs.12303
42
Vangen S Stoltenberg C Skrondal A Magnus P Stray-pedersen B . Cesarean Section Among Immigrants in Norway. Acta Obstet Gynecol Scand (2000). 79:553–8. 10.1080/j.1600-0412.2000.079007553.x
43
Vik ES Nilsen RM Aasheim V Small R Moster D Schytt E . Country of First Birth and Neonatal Outcomes in Migrant and Norwegian-Born Parous Women in Norway: A Population-Based Study. BMC Health Serv Res (2020). 20:540. 10.1186/s12913-020-05415-y
44
Vik ES Aasheim V Schytt E Small R Moster D Nilsen RM . Stillbirth in Relation to Maternal Country of Birth and Other Migration Related Factors: a Population-Based Study in Norway. BMC Pregnancy Childbirth (2019). 19:5. 10.1186/s12884-018-2140-3
45
Villadsen SF Sievers E Andersen A-MN Arntzen A Audard-Mariller M Martens G et al Cross-Country Variation in Stillbirth and Neonatal Mortality in Offspring of Turkish Migrants in Northern Europe. Eur J Public Health (2010). 20:530–5. 10.1093/eurpub/ckq004
46
Gillet E Saerens B Martens G Cammu H . Fetal and Infant Health Outcomes Among Immigrant Mothers in Flanders, Belgium. Int J Gynecol Obstet (2014). 124:128–33. 10.1016/j.ijgo.2013.07.031
47
Opondo C Jayaweera H Hollowell J Li Y Kurinczuk JJ Quigley MA . Variations in Neonatal Mortality, Infant Mortality, Preterm Birth and Birth Weight in England and Wales According to Ethnicity and Maternal Country or Region of Birth: An Analysis of Linked National Data from 2006 to 2012. J Epidemiol Community Health (2020). 74:336–45. 10.1136/jech-2019-213093
48
Villadsen SF Mortensen LH Andersen AM . Ethnic Disparity in Stillbirth and Infant Mortality in Denmark 1981-2003. J Epidemiol Community Health (2009). 63:106–12. 10.1136/jech.2008.078741
49
Zanconato G Iacovella C Parazzini F Bergamini V Franchi M . Pregnancy Outcome of Migrant Women Delivering in a Public Institution in Northern Italy. Gynecol Obstet Invest (2011). 72:157–62. 10.1159/000328318
50
Vang ZM . Infant Mortality Among the Canadian-born Offspring of Immigrants and Non-Immigrants in Canada: a Population-Based Study. Popul Health Metrics (2016). 14:32. 10.1186/s12963-016-0101-5
51
Gould JB Madan A Qin C Chavez G . Perinatal Outcomes in Two Dissimilar Immigrant Populations in the United States: A Dual Epidemiologic Paradox. Pediatrics (2003). 111:e676–e682. 10.1542/peds.111.6.e676
52
Johnson EB Reed SD Hitti J Batra M . Increased Risk of Adverse Pregnancy Outcome Among Somali Immigrants in Washington State. Am J Obstet Gynecol (2005). 193:475–82. 10.1016/j.ajog.2004.12.003
53
Madan A Palaniappan L Urizar G Wang Y Fortmann SP Gould JB . Sociocultural Factors that Affect Pregnancy Outcomes in Two Dissimilar Immigrant Groups in the United States. J Pediatr (2006). 148:341–6. 10.1016/j.jpeds.2005.11.028
54
Raimondi d. Rey CE Testa MV Camoia ED Torreguitar A Meritano J . Migrant Population and Perinatal Health. Arch Argent Pediat (2013). 111:213–7. 10.5546/aap.2013.eng.213
55
Mozooni M Pennell CE Preen DB . Healthcare Factors Associated with the Risk of Antepartum and Intrapartum Stillbirth in Migrants in Western Australia (2005-2013): A Retrospective Cohort Study. Plos Med (2020). 17:e1003061. 10.1371/journal.pmed.1003061
56
Hsieh W-S Hsieh C-J Jeng S-F Liao H-F Su Y-N Lin S-J et al Favorable Neonatal Outcomes Among Immigrants in Taiwan: Evidence of Healthy Immigrant Mother Effect. J Women's Health (2011). 20:1083–90. 10.1089/jwh.2011.2809
57
Liu C-Y Chang N-T Chou P . Testing the "Epidemiologic Paradox" of Birth Outcomes Among Asian Immigrant Women in Hsin-Chu County, Taiwan. J Formos Med Assoc (2008). 107:782–90. 10.1016/s0929-6646(08)60191-6
58
Flenady V Wojcieszek AM Middleton P Ellwood D Erwich JJ Coory M et al Stillbirths: Recall to Action in High-Income Countries. Lancet (2016). 387:691–702. 10.1016/S0140-6736(15)01020-X
59
Muglu J Rather H Arroyo-Manzano D Bhattacharya S Balchin I Khalil A et al Risks of Stillbirth and Neonatal Death with Advancing Gestation at Term: A Systematic Review and Meta-Analysis of Cohort Studies of 15 Million Pregnancies. Plos Med (2019). 16:e1002838–e38. 10.1371/journal.pmed.1002838
60
Meints L Chescheir N . Screening for Infectious Diseases in Pregnant, Foreign-Born Women from Multiple Global Areas. J Reprod Med (2010). 55:382–6.
61
Sagnelli E Taliani G Castelli F Bartolozzi D Cacopardo B Armignacco O et al Chronic HBV Infection in Pregnant Immigrants: A Multicenter Study of the Italian Society of Infectious and Tropical Diseases. New Microbiol (2016). 39:114–8.
62
Heslehurst N Brown H Pemu A Coleman H Rankin J . Perinatal Health Outcomes and Care Among Asylum Seekers and Refugees: A Systematic Review of Systematic Reviews. BMC Med (2018). 16:89. 10.1186/s12916-018-1064-0
63
Higginbottom GMA Evans C Morgan M Bharj KK Eldridge J Hussain B . Experience of and Access to Maternity Care in the UK by Immigrant Women: a Narrative Synthesis Systematic Review. BMJ Open (2019). 9:e029478–e78. 10.1136/bmjopen-2019-029478
64
Gissler M Alexander S MacFarlane A Small R Stray-Pedersen B Zeitlin J et al Stillbirths and Infant Deaths Among Migrants in Industrialized Countries. Acta Obstet Gynecol Scand (2009). 88:134–48. 10.1080/00016340802603805
65
Behboudi-Gandevani S Bidhendi-Yarandi R Panahi MH Mardani A Prinds C Vaismoradi M . Perinatal and Neonatal Outcomes in Immigrants from Conflict-Zone Countries: A Systematic Review and Meta-Analysis of Observational Studies. Front Public Health (2022). 10:766943. 10.3389/fpubh.2022.766943
66
Wolff H Epiney M Lourenco AP Costanza MC Delieutraz-Marchand J Andreoli N et al Undocumented Migrants Lack Access to Pregnancy Care and Prevention. BMC Public Health (2008). 8:93. 10.1186/1471-2458-8-93
67
van den Akker T van Roosmalen J . Maternal Mortality and Severe Morbidity in a Migration Perspective. Best Pract Res Clin Obstet Gynaecol (2016). 32:26–38. 10.1016/j.bpobgyn.2015.08.016
68
Li X Sundquist J Sundquist K . Immigrants and Preterm Births: a Nationwide Epidemiological Study in Sweden. Matern Child Health J (2013). 17:1052–8. 10.1007/s10995-012-1087-7
69
Gieles NC Tankink JB van Midde M Düker J van der Lans P Wessels CM et al Maternal and Perinatal Outcomes of Asylum Seekers and Undocumented Migrants in Europe: a Systematic Review. Eur J Public Health (2019). 29:714–23. 10.1093/eurpub/ckz042
70
Collingwood Bakeo A . Investigating Variations in Infant Mortality in England and Wales by Mother's Country of Birth, 1983-2001. Paediatr Perinat Epidemiol (2006). 20:127–39. 10.1111/j.1365-3016.2006.00708.x
71
Nybo Andersen A-M Gundlund A Villadsen SF . Stillbirth and Congenital Anomalies in Migrants in Europe. Best Pract Res Clin Obstet Gynaecol (2016). 32:50–9. 10.1016/j.bpobgyn.2015.09.004
72
Johnsen H Ghavami Kivi N Morrison CH Juhl M Christensen U Villadsen SF . Addressing Ethnic Disparity in Antenatal Care: a Qualitative Evaluation of Midwives' Experiences with the MAMAACT Intervention. BMC Pregnancy Childbirth (2020). 20:118–0. 10.1186/s12884-020-2807-4
73
Korinek K Smith KR . Prenatal Care Among Immigrant and Racial-Ethnic Minority Women in a New Immigrant Destination: Exploring the Impact of Immigrant Legal Status. Soc Sci Med (2011). 72:1695–703. 10.1016/j.socscimed.2011.02.046
74
Oliva-Arocas A Pereyra-Zamora P Copete JM Vergara-Hernández C Martínez-Beneito MA Nolasco A . Socioeconomic Inequalities in Mortality Among Foreign-Born and Spanish-Born in Small Areas in Cities of the Mediterranean Coast in Spain, 2009-2015. Ijerph (2020). 17:4672. 10.3390/ijerph17134672
75
Sow M Racape J Schoenborn C De Spiegelaere M . Is the Socioeconomic Status of Immigrant Mothers in Brussels Relevant to Predict Their Risk of Adverse Pregnancy Outcomes?BMC Pregnancy Childbirth (2018). 18:422–2. 10.1186/s12884-018-2043-3
76
Wahlberg Å Rööst M Haglund B Högberg U Essén B . Increased Risk of Severe Maternal Morbidity (Near-Miss) Among Immigrant Women in Sweden: a Population Register-Based Study. Bjog: Int J Obstet Gy (2013). 120:1605–12. 10.1111/1471-0528.12326
77
Xirasagar S Fu J-C Liu J Probst JC Lin D-P . Neonatal Outcomes for Immigrant vs. Native-Born Mothers in Taiwan: an Epidemiological Paradox. Matern Child Health J (2011). 15:269–79. 10.1007/s10995-010-0612-9
78
Lu Y Qin L . Healthy Migrant and salmon Bias Hypotheses: a Study of Health and Internal Migration in China. Soc Sci Med (2014). 102:41–8. 10.1016/j.socscimed.2013.11.040
79
Helgesson M Johansson B Nordquist T Vingård E Svartengren M . Healthy Migrant Effect in the Swedish Context: A Register-Based, Longitudinal Cohort Study. BMJ Open (2019). 9:e026972–e72. 10.1136/bmjopen-2018-026972
80
Syse A Dzamarija MT Kumar BN Diaz E . An Observational Study of Immigrant Mortality Differences in Norway by Reason for Migration, Length of Stay and Characteristics of Sending Countries. BMC Public Health (2018). 18:508–8. 10.1186/s12889-018-5435-4
Summary
Keywords
meta-analysis, immigration, perinatal mortality, neonatal mortality, stillbirth
Citation
Behboudi-Gandevani S, Bidhendi-Yarandi R, Panahi MH, Mardani A, Gåre Kymre I, Paal P and Vaismoradi M (2022) A Systematic Review and Meta-Analysis of the Risk of Stillbirth, Perinatal and Neonatal Mortality in Immigrant Women. Int J Public Health 67:1604479. doi: 10.3389/ijph.2022.1604479
Received
21 September 2021
Accepted
28 April 2022
Published
18 May 2022
Volume
67 - 2022
Edited by
Mariachiara Di Cesare, University of Essex, United Kingdom
Updates
Copyright
© 2022 Behboudi-Gandevani, Bidhendi-Yarandi, Panahi, Mardani, Gåre Kymre, Paal and Vaismoradi.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Samira Behboudi-Gandevani, samira.behboudi-gandevani@nord.no
ORCID: Samira Behboudi-Gandevani orcid.org/0000-0003-3526-640X
Razieh Bidhendi-Yarandi orcid.org/0000-0002-2533-167X
Abbas Mardani orcid.org/0000-0003-2861-6037
Piret Paal orcid.org/0000-0002-1341-3248
Mojtaba Vaismoradi orcid.org/0000-0002-5157-4886
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.