Abstract
Objectives: The Conservation of Resources (COR) theory suggests that stress results from threatened or actual loss of resources following significant life events. This study used COR theory as the framework to explore the reflection of loss of resources during the COVID-19 pandemic on psychological distress and resilience, in an adult Jewish Israeli population.
Methods: We examined the association between background variables, stress, loneliness, concern, COVID-19-related post traumatic symptoms (PTS), resilience factors and COR via an online survey among 2,000 adults during April 2020.
Results: Positive relationships were identified between resource loss and PTS (r = 0.66, p < 0.01), and between resource gain and resilience (r = 0.30, p < 0.01). Psychological variables were significantly associated with PTS and explained 62.7% of the variance, F (20, 1,413) = 118.58, p < 0.001.
Conclusion: Loss of resources, stress, loneliness and concern were found to be risk factors for distress and PTS, whereas resilience factors played a protective role. We thus recommend using the COR theory to explore COVID-19 effects elsewhere.
Introduction
The socio-psychological consequences of the COVID-19 pandemic are widespread, possibly affecting mental health not only now but into the future [1]. Although the population of Israel is known for its resilience to security-related crises, it is not known how they would face an epidemic threat. With the growing availability of the vaccine, it is important to deepen our understanding of the psycho-social distress and coping of the population. Hopefully, such understanding will lead to wide-scale interventions to help restore psychological equilibrium as the world moves towards learning to live with COVID-19.
The COVID-19 pandemic could leave many people with psychological scars, such as depression [2] anxiety, stress, traumatic symptoms [3], and loneliness [4], which are common reactions to a health crisis. The pandemic raised the general anxiety levels [5]. Thus, uncertainties about the future, anxiety and fear may last even after COVID-19 is eradicated or contained. Loneliness as well, has been found to be a central risk factor for depression, anxiety, and comorbidity during the COVID-19 pandemic [4]. The widely adopted social and physical distancing, lockdowns, isolation and quarantine have not surprisingly resulted in severe psychiatric disorders [6], as did the emotional burden of loneliness [7]. However, mental health researchers suggest viewing the COVID-19 crisis from a broader trauma perspective [8]. Seen this way, infectious disease epidemics can be highly traumatic experiences for individuals and lead to post-traumatic stress disorder (PTSD) and chronic psychological distress, especially for those already vulnerable or who are most deeply impacted by the disease and its co-travellers [9].
The COVID-19 pandemic and its effects on people’s lives highlight the need to deepen our knowledge in the concepts of resilience and human resources and their impact on distress and coping. Personal Resilience is defined as a trajectory of healthy functioning after a highly adverse event [10]. Lahad [11] claims that some individuals have a unique resource repertoire that helps them deal with crises. Studies of personal resilience during the COVID-19 pandemic have shown a link between high personal resilience and decreased anxiety, distress, feelings of danger, depression and anxiety [12].
Community resilience is defined as “the community’s ability to withstand crises or disruptions” [13], and is another resource that may be supportive for individuals during a global pandemic, particularly when people were asked to remain in their physically close domain.
The Conservation of Resources theory (COR) [15] has often been adopted to study major and traumatic stress in crisis situations, and has been referenced as a framework for understanding stress in many studies. According to COR theory, people strive to retain, protect, and build resources and are threatened by the potential or actual loss of these valued resources. Resources may be material (e.g., money, housing), social (e.g., social support, status) or psychological (e.g., personal mastery, sense of autonomy) [15]. Loss of resources, or threat of such loss, is a crucial variable, predicting psychological distress, and will lead to investing more resources, making those already lacking in resources even more vulnerable to loss spirals [15]. Concrete primary-resource losses and secondary losses that occur later, were found to best predict psychological distress during major crisis [16].
COR theory also emphasizes resource gain, such that gain of important resources and associated positive emotions may increase in value in the face of loss. When resource loss occurs, the ability to gain resources becomes increasingly important, providing an emotional respite and the ability to achieve goals [17]. As such, following a crisis, resource loss is seen as more impactful than resource gain, which is seen to have more modest, even if important influence.
Despite its important contribution, the association between COR theory and the COVID-19 pandemic has been studied only to a limited extent [18–21]. The physical health, economic and socio-psychological consequences of COVID-19 inevitably result in multiple forms of loss of resources (e.g., loss of a loved one, health, financial stability, job, social connection and sense of security), which may increase the likelihood of developing traumatic symptoms and psychological distress [9].
Among the studies examining the impact of the COVID-19 pandemic on mental health, the impact of resource loss and gain (COR) has received little attention. To fill this gap, the present study examined COR and its association with personal and community resilience as well as psychological distress.
The study objectives are:
(1) To examine the association between COR and psychological distress related to COVID-19,
(2) To examine the association between COR and resilience during the COVID-19 pandemic.
Hypotheses:
Adjusted for demographic and psychological variables, resource loss will be associated with an increase in psychological distress, and resource gain will be associated with an increase in resilience factors.
Methods
Data Collection
Data were collected through an online survey distributed for 4 days in April 2020, to participants in Israel at the time of the pandemic. The survey was sent through Midgam Project Web Panel, an Israeli company specializing in internet research via an online panel (www.midgampanel.com), where panelists are paid to participate in periodic surveys. Participants are sampled using a stratified quota sampling. The study was pre-approved by the Institutional Review Board (IRB) of the Faculty of Health Sciences at Ben-Gurion University of the Negev. An introduction at the beginning of the survey described the study’s objectives and specified that completing the questionnaire was voluntary and could be terminated at any time. According to the checklist for reporting results of internet [22], it was possible to change the answers before submitting the questionnaire. The questionnaires were anonymous to the research team, and each user could participate only once using a unique identifier.
Participants
Of the 2,302 panelists who responded to the survey, 2,000 participants provided complete responses (86.9%). Participants were Jewish adults (aged 17–74 years), residents of Israel, representing the adult Jewish population in Israel in the examined age range.
Measures
Resource Loss and Gain
A modified version of the Conservation of Resources Evaluation Questionnaire (COR-E) [23] was used, with 7 items representing perceived loss of resources and 7 items representing perceived gain of resources relevant to the pandemic. Loss of resources (such as loss of meaning and purpose, financial stability, etc.) was rated on a 5-point Likert scale (0—I did not lose at all, 4—I lost very much). The gain items (such as meaning and purpose, closeness to family and friends) were rated on a 5-point Likert scale (0—I did not gain at all, 4—I gained very much). Internal reliability for resource loss (α = 0.87) and for resource gain (α = 0.84) in study population were good.
COVID-19-Related Traumatic Symptoms
The items used to measure traumatic symptoms related to COVID-19 were taken from three validated questionnaires: CAPS-5 [24], PDS [25], and Patient Health Questionnaire - PHQ-9 [26]. The 18 items (e.g., “I have troubling thoughts about events related to Corona”) examined the existence of continuous traumatic symptoms associated with COVID-19 according to DSM-5 criteria [27]. The responses were rated on a four-point Likert scale (0—not at all, 3—very much). Internal reliability was high (α = 0.90).
COVID-19 Related Concern
The 7-item measurement tool was the situational anxiety questionnaire [28], based on the Spielberger [29] State-Trait Anxiety Inventory (STAI). The 7 items (e.g., “I am worried about the spread of the coronavirus”) were rated on a 5-point Likert scale (0—not at all, 4—very much). Internal reliability was high (α = 0.88).
Loneliness
The revised UCLA Loneliness Scale [30] was used to measure loneliness. Of the 20 items in the scale, three were used in the current study (e.g., “How many times in the last month have you felt: that you have no one to turn to”), were rated on a 5-point Likert scale (0—never, 4—always). Internal reliability was good (α = 0.80).
Personal Resilience
Personal resilience was measured by the 10-item Conor Davidson scale (CD-RISC10, [31]. The statements (e.g., “I can deal with unpleasant feelings”) were rated on a 5-point Likert scale (0—not at all, 4—largely correct). Internal reliability in the present study was high (α = 0.88).
Community Resilience
A modified version of the Conjoint Community Resiliency Assessment Measure (CCRAM-10 [14]; was used. The 6 items (e.g., “The community in which I live in is functioning properly”) were rated on a 5-point Likert scale (0—strongly disagree, 4—strongly agree). Internal reliability was high (α = 0.89).
Background Information
Participants were asked about their background. Questions referred to gender, marital status, dependents, housing, education, religiosity, birthplace, health status, income, history of quarantine, and volunteer activity.
Data Analysis
Data were analyzed using Statistical Package for the Social Sciences (SPSS) version 25 and JASP version 13. Only completed questionnaires were analyzed. Mean and Standard Deviation indices were calculated.
Cronbach’s alpha was used to examine each component of the survey instrument -COR-E, COVID-19-related traumatic symptoms, COVID-19 related concern, loneliness, personal resilience and community resilience reliability. Pearson correlation coefficients were calculated and used to examine the association between resource loss, resource gain, resilience factors, psychological distress factors and background variables. Additional Pearson tests were performed to examine the association between traumatic symptoms and resource loss items, the association between traumatic symptoms and concern items, and between personal resilience and resource gain statements. Subsequently, hierarchical linear regression modeling was performed to predict COVID-19-related traumatic symptoms adjusted to demographic and psychological variables. In the first step, the demographic variables were brought under control, and in the second step, the psychological and other variables were introduced. p-values are reported at a significance level of p = 0.05 and p = 0.01.
Results
Study Variables
As presented in Table 1, the mean age of the participants was 42.25 years (SD = 15.73, range 17–74 years). About half of the respondents were men (n = 995, 49.75%). Most participants (n = 1,055, 59%) were married or cohabiting. The majority of the participants reported attaining post-secondary (n = 564, 28.2%) or academic education (n = 885, 44.25%). About 75% (n = 1,489) of the sample reported being generally healthy. As related to the pandemic—14.9% (n = 299) were quarantined at the time of measurement; only 0.4% (n = 8) of the participants were tested positive to COVID-19 by the time of the survey (early April 2020).
TABLE 1
| Variables | N | % |
|---|---|---|
| Gender | ||
| Female | 1,004 | 50.20 |
| Male | 995 | 49.75 |
| Marital status | ||
| Married/cohabiting | 1,055 | 59.05 |
| Single | 915 | 40.95 |
| Age | ||
| 15–24 | 305 | 15.25 |
| 25–34 | 436 | 21.80 |
| 35–44 | 397 | 19.85 |
| 45–54 | 320 | 16.00 |
| 55–64 | 309 | 15.45 |
| 65+ | 233 | 11.65 |
| Children under 16 | ||
| 0 | 884 | 44.20 |
| 1 | 315 | 15.70 |
| 2 | 227 | 11.30 |
| 3 | 130 | 6.50 |
| 4+ | 69 | 3.30 |
| Number of people at home | ||
| 0 | 86 | 4.30 |
| 1 | 272 | 13.60 |
| 2 | 478 | 23.90 |
| 3 | 343 | 17.10 |
| 4 | 330 | 16.50 |
| 5 | 286 | 14.30 |
| 6+ | 203 | 10.00 |
| Dependents | ||
| Special needs | 72 | 3.60 |
| Dependent child | 519 | 25.95 |
| Dependent adult | 197 | 9.85 |
| Over 70 | 175 | 8.75 |
| House type | ||
| Apartment | 1,393 | 69.65 |
| House | 572 | 28.60 |
| Garden/view in the house | 1,604 | 80.20 |
| Education | ||
| University/college | 885 | 44.25 |
| Post-secondary education | 564 | 28.20 |
| High school | 494 | 24.70 |
| Elementary school | 21 | 1.05 |
| Religiosity | ||
| Religious | 793 | 29.16 |
| Secular | 1,207 | 60.35 |
| Birthplace | ||
| Israel | 1,613 | 80.65 |
| Not in Israel | 387 | 19.35 |
| Health status | ||
| Healthy | 1,489 | 74.45 |
| Chronic illness | 477 | 23.85 |
| Income | ||
| Above average | 296 | 14.80 |
| Average | 544 | 27.20 |
| Below average | 944 | 47.20 |
| Quarantined | 299 | 14.95 |
| SARS-CoV-2 positive | 8 | 0.40 |
| Volunteering in a routine | 471 | 23.50 |
| Volunteering during COVID-19 | 309 | 15.40 |
Demographic characteristics of respondents (N = 2000). Conservation of resources during the COVID-19 pandemic, Israel, 2020.
Table 2 presents descriptive statistics and Pearson correlations between study variables. As seen in Table 2, resource gain’s mean score (M = 1.71, SD = 1.01) was higher than resource’s loss mean score (M = 1.03, SD = 0.86).
TABLE 2
| Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | Range | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. COVID-19-related concern | 1.94 | 1.90 | 0–4 | |||||||
| 2. Stress | 1.49 | 0.94 | 0.66** | 0–4 | ||||||
| 3. Loneliness | 1.36 | 0.96 | 0.29** | 0.49** | 0–4 | |||||
| 4. Personal resilience | 3.09 | 0.67 | −0.18** | −0.31** | −0.29** | 0–4 | ||||
| 5. Resources loss | 1.03 | 0.86 | 0.34** | 0.52** | 0.50** | −0.37** | 0–4 | |||
| 6. Resources gain | 1.71 | 1.01 | 0.07** | −0.07** | −0.14** | 0.21** | −0.08** | 0–4 | ||
| 7. Community resilience | 2.46 | 0.94 | −0.08** | −0.16** | −0.21** | 0.23** | −0.25** | 0.30** | 0–4 | |
| 8. COVID-19 related traumatic symptoms | 0.72 | 0.53 | 0.47** | 0.69** | 0.56** | −0.44** | 0.66** | −0.09** | −0.22** | 0–3 |
Means, standard deviations, and Pearson correlations between study variables. Conservation of resources during the COVID-19 pandemic, Israel, 2020.
*p < 0.05, **p < 0.01.
Figure 1, focuses on the relationships between resource loss and study variables and demonstrates the large positive correlation between resource loss, COVID-19-related traumatic symptoms (r = 0.66, p < 0.01); stress (r = 0.52, p < 0.01); loneliness (r = 0.50, p < 0.01); COVID-19 related concern (r = 0.33, p < 0.01). Negative associations were found between resource loss and personal resilience (r = −0.37, p < 0.01) and between resource loss and community resilience (r = −0.25, p < 0.01).
FIGURE 1
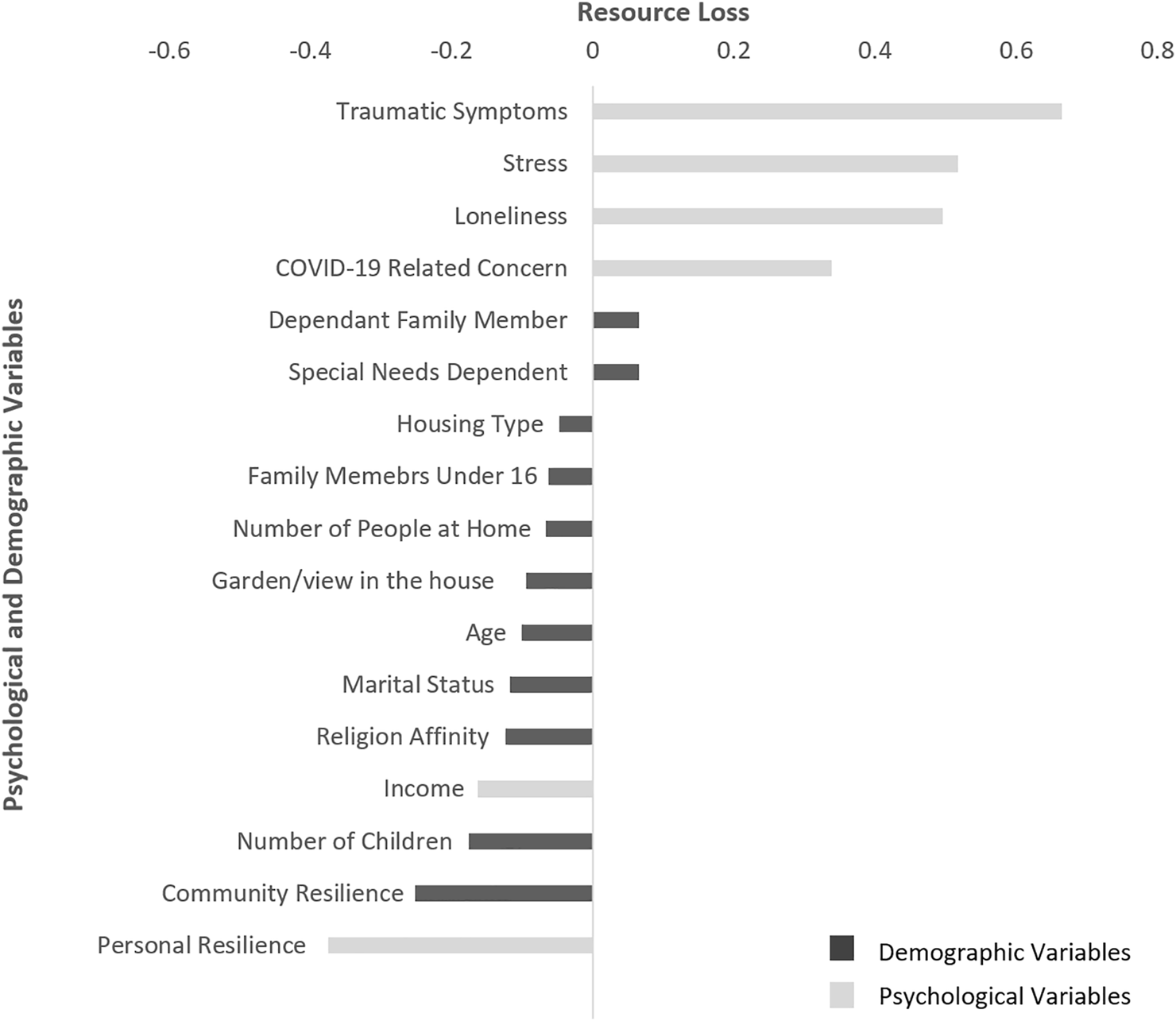
Correlations between demographic and psychological variables and resource loss. Conservation of resources, psychological distress and resilience during the COVID-19 pandemic, Israel, 2020.
Figure 2 portrays the relationships between resources gain and study variables. Positive correlations were noted between resource gain and community resilience (r = 0.30, p < 0.01) as well as between resource gain and personal resilience (r = 0.30, p < 0.01).
FIGURE 2
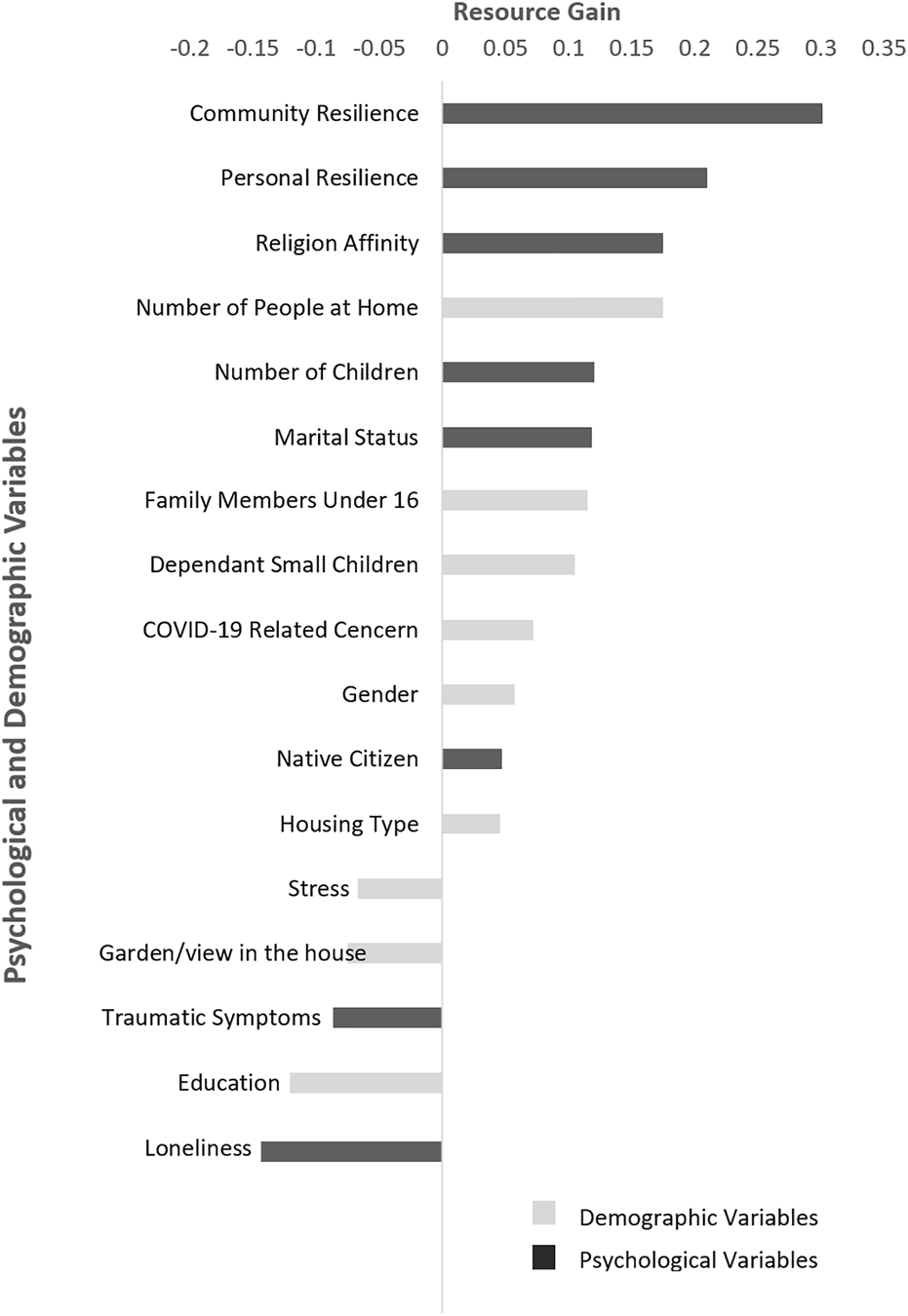
Correlations between demographic and psychological variables and resource gain. Conservation of resources psychological distress and resilience during the COVID-19 pandemic. Israel, 2020.
Resource Gain and Loss Items and Their Relationships to Resilience Variables
To examine the relationships between resource gain and personal resilience, a Pearson correlation test was performed. Figure 3 shows the relationships between resource gain items and personal resilience. The strongest correlation was found between personal resilience and “doing enjoyable or important things” (r = 0.18, p < 0.01).
FIGURE 3
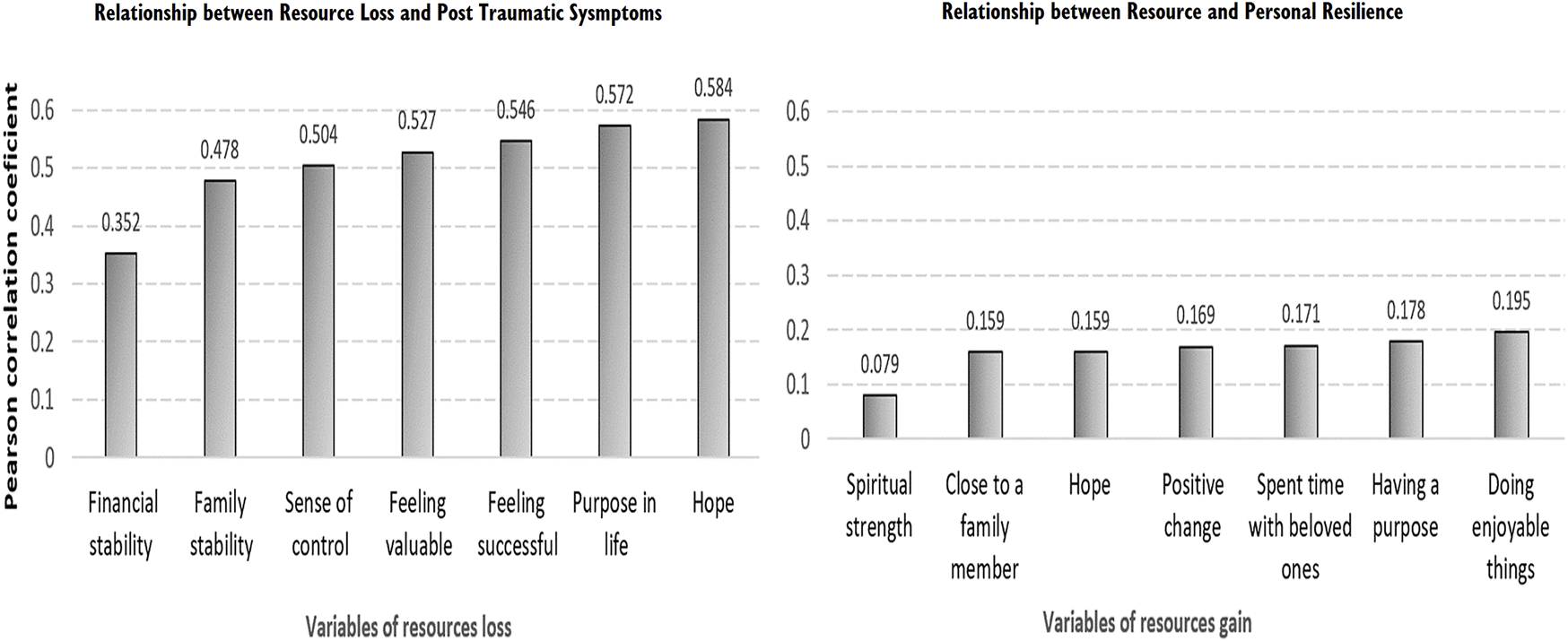
Relationship between resource loss and PTS and personal resilience. conservation of resources psychological distress and resilience during the COVID-19 pandemic, Israel, 2020.
To examine the links between traumatic stress symptoms and resource loss items, additional Pearson tests were performed. Figure 3 further demonstrates that loss of hope had the highest association with the possibility of COVID-19 related traumatic symptoms (r = 0.58, p < 0.01), followed by a loss of a sense of meaning or purpose in life (r = 0.57, p < 0.01), and a loss of a sense of success (r = 0.54, p < 0.01), and value (r = 0.52, p < 0.01). Financial stability had the lowest association with COVID-19-related traumatic symptoms (r = 0.35, p < 0.01).
Significant, yet weak, correlations were found between health status and most of the study variables. Specifically, healthy individuals were found to have less resource loss (r = −0.07, p < 0.01), more resource gain (r = 0.09, p < 0.01), less COVID-19-related traumatic symptoms (r = −0.11, p < 0.01), less COVID-19 related concern (r = −0.09, p < 0.01), less loneliness (r = −0.06, p < 0.01), higher personal resilience (r = 0.05, p < 0.05) and higher community resilience (r = 0.05, p < 0.05), than individuals whose health status was poor.
Traumatic Symptoms Related to COVID-19 Situation
To examine which of the demographic and psychological variables is associated with COVID-19-related traumatic symptoms, a hierarchical linear regression was performed. In the first step, the demographic variables were entered, and in the second step, the psychological and other variables were added.
Background variables explained 6.8% of the variance in COVID-19-related traumatic symptoms, F (12, 1,421) = 9.68, p < 0.001. Specifically, having a dependent family member or dependent person with special needs (β = 0.09, p < 0.01), religiosity (β = -0.10, p < 0.01), low income (β = −0.07, p < 0.01), and being female (β = 0.10, p < 0.01) were related to more severe traumatic symptoms (see Table 3).
Table 3
| Variable | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
| B | (β) | S.E.B. | B | (β) | S.E.B. | |
| Step 1 | ||||||
| Age | −0.00 | −0.05 | 0.00 | −0.00 | −0.03 | 0.00 |
| No. of household members under 16 | 0.00 | −0.01 | 0.01 | 0.00 | 0.00 | 0.01 |
| Dependent family member | 0.17 | 0.09** | 0.04 | 0.06 | 0.03* | 0.03 |
| Dependent person with special needs | 0.25 | 0.09** | 0.07 | 0.08 | 0.03 | 0.04 |
| Housing type | −0.06 | −0.06* | 0.03 | −0.00 | −0.00 | 0.02 |
| Garden/view in the house | 0.05 | 0.03 | 0.03 | −0.03 | −0.02 | 0.02 |
| Religiosity | −0.05 | −0.10** | 0.01 | −0.01 | −0.02 | 0.01 |
| Living alone | −0.01 | 0.03 | 0.01 | −0.01 | −0.03 | 0.00 |
| Marital status | −0.03 | −0.02 | 0.03 | −0.02 | −0.02 | 0.02 |
| Income | −0.03 | −0.07** | 0.01 | 0.00 | 0.00 | 0.00 |
| Gender (female) | 0.10 | 0.10** | 0.02 | 0.03 | 0.32 | 0.01 |
| No. of children | −0.02 | −0.07 | 0.01 | 0.01 | 0.04 | 0.00 |
| Step 2 | ||||||
| COVID-19-related concern | 0.03 | 0.05* | 0.01 | |||
| Loneliness | 0.08 | 0.15** | 0.01 | |||
| Stress | 0.17 | 0.32** | 0.01 | |||
| Personal resilience | −0.12 | −0.16** | 0.01 | |||
| Community resilience | −0.01 | −0.02 | 0.01 | |||
| Resource loss | 0.20 | 0.33** | 0.01 | |||
| Resource gain | 0.00 | 0.01 | 0.00 | |||
| R 2 | 0.07** | 0.62** | ||||
| ΔR2 | 0.07** | 0.55** | ||||
| F | 9.68** | 118.5** | ||||
Hierarchical Regression Coefficients associated with COVID-19-related Traumatic Symptoms according to Demographic and Psychological Variables (N = 1,425). Conservation of Resources Psychological Distress and Resilience during the COVID-19 pandemic, Israel, 2020.
*p < 0.05 **p < 0.01.
Loneliness and stress, significantly contributed to COVID-19-related traumatic symptoms and explained 62.7% of the variance, F (20, 1,413) = 118.58, p < 0.001. Specifically, COVID-19-related stress (β = 0.32, p < 0.01) and resource loss (β = 0.33, p < 0.01) had the most significant individual contribution to COVID-19-related traumatic symptoms. Additional unique contributions were found with loneliness (β = 0.15, p < 0.01), low personal resilience (β = −0.16, p < 0.01). All of which were significantly associated with COVID-19- related traumatic symptoms.
Discussion
The Conservation of Resources theory [15], emphasizing the association of the potential or actual loss or gain of resources with individuals’ well-being, was supported in the current study of the COVID-19 pandemic. We examined the associations between resources loss and gain, psychological distress, and resilience factors among Jewish adults in Israel at the early stage of COVID-19 when the country was in lockdown and vaccines were a far-off dream.
The COVID-19 pandemic can be highly stressful for all individuals. However, our study suggests that those who suffered more were females, people with lower-income, more secular affiliation, or a person with special needs dependent on them.
Our findings correspond with the psycho-social disturbances that were found in previous studies, particularly among those who had low socioeconomic status, job loss, or unemployment status following traumatic exposure [32]. In addition, they reflect reduced access to psycho-social and financial resources [33]. Resources like job and income are part of the individual’s self-identity, and their loss may reduce self-esteem, sense of security and sense of meaning in life. From this perspective, we can identify the COVID-19 pandemic as an existential crisis [34].
Level of religiosity was found to be negatively associated with traumatic symptoms. Religions can create a sense of meaning and trust in high powers [35]. Our study showed that spirituality seems to play a role in alleviating suffering and minimizing the consequences of social isolation [36].
During COVID-19, families are under multiple-stressors: trying to adapt to the uncertainty caused by the lockdowns, the fear for their members’ health, experiencing losses and the challenges of strengthening vital bonds, and overcoming difficulties [37]. Our results suggest that families with a dependent member, and of lower income, were more vulnerable than others. Preexisting vulnerabilities within families increase susceptibility to psycho-social disruptions during the COVID-19 pandemic [38]. In our study we found that large, religious, and upper-middle-class families have been able to gain more resources, comparing with low-class families with a dependent or disabled family member.
Being a female was found to be a risk factor for reporting more traumatic symptoms [39]. On the other hand, women reported higher resource gain scores than men. A possible hypothesis for these findings suggests that women’s greater tendency to ruminative thinking and their coping style, centered on emotion, facilitates both stress and growth [40]. Another possible explanation for women’s higher ability to feel stress and to perceive resource gain is that during the COVID-19 pandemic, the domestic challenges became the focus of coping, and there, traditionally, the woman has more tasks that were intensified during the lockdown situation (e.g. looking after kids and close relatives, cooking, etc.). Based on these mixed findings we would like to stress that it reflects the first wave of the epidemic, and it is still unclear how women will be affected by the epidemic over time.
Our first hypothesis, that a strong association will be found between resource loss and psychological distress levels, was confirmed by the current study. Furthermore it indicated that the psychological variables, especially loss of valued resources (such as hope, sense of meaning or purpose in life), had the most significant contribution as a risk factor for COVID-19-related traumatic symptoms. Additionally, significant positive correlations were found between resource loss and psychological distress such as traumatic symptoms related to COVID-19: loneliness, stress, and COVID-19-related concerns) about the spread of the coronavirus, changes in daily routine, personal and relative’s health and threaten on life).
Our findings thus support the Conservation of Resources theory (COR) which emphasizes that loss of resources can challenge the ability of individuals to cope with and recover from traumatic situations [15]. In a stressful global pandemic, multiple types of loss threatened or caused a depletion of people’s resources, and was associated with an increase in stress levels. Psycho-social resource loss can be seen as a spiral of deficit the longer the crisis persists and affects other areas of life [41].
Our findings suggest that resource loss was highly associated with loneliness, a crucial factor in the COVID-19 epidemic [42]. Of all the losses examined in the current study, loss of hope had the highest association with COVID-19-related traumatic symptoms. Hope as a resilience factor might reduce psychological distress [43], and hopeful people are better able to respond to challenging situations.
Previous studies have shown a chain mediation model using other variables, showing that health information and the perceived impact of the pandemic were mediators that contributed to mental health [44], and other variables (such as coping strategies) have mediation effect on our research variables [45]. Further studies will focus on the identification the moderating and mediating variables of our study’s variables over time.
Our second hypothesis focused on the association between resource gain and resilience factors, was also confirmed. A significant positive correlation was found between resource gain, community resilience, and personal resilience. As predicted by the COR theory, resource gain’s influence was substantively less powerful than that of resource loss [23]. However, our findings suggest that overall, the Israeli Jewish population exhibited a greater resource gain than resource loss in the first wave of the COVID-19.
The correlation found between resource gain and resilience factors highlights the importance of resource gain aspect when dealing with crises. People who had higher resource gain reported doing more enjoyable or valuable things and having a sense of purpose in life. These results are supported by the post-traumatic growth concept (PTG) [46], which focuses on positivity when individuals experience adversity and contains a transformative potential, whereby a person grows in appreciation of life, envisioning new possibilities, personal strength, and spiritual understanding [46].
Personal and community resilience were found to be the best protective factors for decreased psychological distress. Our findings support other studies that presented the crucial role of resilience factors, especially of personal resilience, on mental health when coping with COVID-19 threats [47].
Resilience refers to the extent to which people could manage to create and sustain resource gains, it acted as a vital protector that enables the ability to “bounce forward” despite the pandemic challenges and maintain functioning.
As data for this study were collected at the early stages of the pandemic, the rate of illness and death at the time was still low compared to later stages. Future work should follow these measures repeatedly and address the association between aspects such as COVID-19 morbidity and mortality and changing socio-economic status on the variables measured in this study.
Limitations
The use of an online approach to data collection through the MIDGAM web panel limited us to the population in their database which represents the computer literate Jewish population only. Nevertheless, the vast majority of Israels’ population uses the Internet (84% in January 2020, 88.0% in January 2021) [48]. The MIDGAM web panel [49] has access to hundreds of thousands of Israelis who are interested in partaking in online studies, usually for monetary reimbursement and provides a statistically representative sample of the adult Jewish population in Israel, so in terms of the population of this study, it is deemed sufficient. Furthermore, at the time of the study, when people were confined home, it was the best possible way, as only 53% of the households have a landline [50].
Previous studies during the COVID-19 pandemic highlighted this susceptibility of selection bias, claiming that large sample sizes, not necessarily compensate for that bias and might even exacerbate it [51]. Our findings thus have the potential to not fully represent the general population and to limit the interpretations of the findings to the population described above (higher educational level for example). Despite that, based on previous studies using this panel company [5], we feel that it is safe to assume that the sample offers insights which are representative of the adult Jewish population in Israel. Beyond that, it is important to remember that we did not try to characterize the population or to infer about it as a population but rather examined a human psycho-social experience and the relationship between people’s available resources, their psychological distress and resilience. Therefore, the meaning of this potential bias could be marginal. Nevertheless, it is necessary to test our findings on diverse samples in order to confirm the study’s validity on other populations.
Conclusion and Recommendations
The COR theoretical framework offers a prism for understanding people’s coping with traumatic experiences, and offers important insights that can serve to plan support for individuals and communities in the context of COVID-19. The study supports the need for handling the COVID-19 mental health consequences as part of the national systemic response. Interventions should focus on both the physical and environmental levels (money, agile working conditions etc.) and people’s internal resources (such as creating new meanings in life) in order to reduce psychological negative effects. Precisely at time of crises, resources are inaccessible and are critical to recovery. The ongoing loss should be ceased in the early stages, before the acceleration of resource loss and negative effect of loss spirals. Acquiring new psychological resources may be a tool in cultivating mental well-being. This awareness-raising may be part of the role of policymakers, education and health systems leaders and it should be conveyed by the media as well.
Our study shows that it is important to develop resilience skills, cultivate hope and create mental-health interventions to vulnerable populations that have experienced a loss of resources due to this pandemic and those who suffer from loneliness. Actually, the findings that reflect the constant vulnerability of part of the population to distress and their limited access to resources, should raise concern, as it reflects the need for policy of caring for populations which are vulnerable to crises. Local leaders and digital communities’ leaders should take a role in strengthening community resilience in order to support mental well-being. The long-term social and psychological effects of COVID-19 are only starting to be known, yet based on the current research and other studies, and given the critical protective role of resilience, we recommend examining the concept of family resilience in the face of social challenges during a global epidemic.
Statements
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Review Board (IRB) of the Faculty of Health Sciences at Ben-Gurion University of the Negev, Israel. The patients/participants provided their written informed consent to participate in this study.
Author contributions
HEF: Study idea, literature search, study design, data analysis and interpretation, drafting the manuscript. ML: Study design, data interpretation, reviewing and editing of various drafts, contribute to Introduction and Discussion sections. DL: Data analysis and interpretation, contribute to the Methods and the Results sections. SH: Reviewing and editing of various drafts, contribute to Introduction and Discussion sections. LA-D: Study design, data analysis and interpretation, reviewing and editing of various drafts, contribute to the Introduction and the Results sections. All authors contributed to the manuscript and approved it for submission.
Funding
This work was supported by the PREPARED Center for Emergency response research at Ben-Gurion University of the Negev, Israel.
Conflict of interest
Author SH was employed by the company STress Anxiety and Resilience Consultants-STAR.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.
Holmes EA O’Connor RC Perry VH Tracey I Wessely S Arseneault L et al Multidisciplinary Research Priorities for the COVID-19 Pandemic: a Call for Action for Mental Health Science. The Lancet Psychiatry7 (2020). p. 547–60.
2.
Bueno-Notivol J Gracia-García P Olaya B Lasheras I López-Antón R Santabárbara J . Prevalence of Depression during the COVID-19 Outbreak: A Meta-Analysis of Community-Based Studies. Int J Clin Health Psychol (2021)(1) 100196. 10.1016/j.ijchp.2020.07.007
3.
Chi X Becker B Yu Q Willeit P Jiao C Huang L et al Prevalence and Psychosocial Correlates of Mental Health Outcomes Among Chinese College Students during the Coronavirus Disease (COVID-19) Pandemic. Front Psychiatry (2020) 803. 10.3389/fpsyt.2020.00803
4.
Palgi Y Shrira A Ring L Bodner E Avidor S Bergman Y et al The Loneliness Pandemic: Loneliness and Other Concomitants of Depression, Anxiety and Their Comorbidity during the COVID-19 Outbreak. J Affective Disord275 (2020). p. 109–11.
5.
Shahar G Aharonson-Daniel L Greenberg D Shalev H Malone PS Tendler A et al Changes in General and Virus-specific Anxiety during the Spread of COVID-19 in Israel: A Seven-Wave Longitudinal Study. Am J Epidemiol (2021).
6.
Galea S Merchant RM Lurie N , The Mental Health Consequences of COVID-19 and Physical Distancing: The Need for Prevention and Early Intervention. JAMA Intern Med180 (2020). p. 817–8.
7.
Banerjee D Rai M . Social Isolation in Covid-19: The Impact of Loneliness. Int J Soc Psychiatry (2020) 52:525–7. 10.1177/0020764020922269
8.
Horesh D Brown AD . Traumatic Stress in the Age of COVID-19: A Call to Close Critical Gaps and Adapt to New Realities.. Psychol Trauma (2020) 12(4):331–5. 10.1037/tra0000592
9.
Boyraz G Legros DN . Coronavirus Disease (COVID-19) and Traumatic Stress: Probable Risk Factors and Correlates of Posttraumatic Stress Disorder. J Loss Trauma (2020) 25(6–7):503–22. 10.1080/15325024.2020.1763556
10.
Bonanno GA Loss, Trauma, and Human Resilience: Have We Underestimated the Human Capacity to Thrive after Extremely Aversive Events? 59. American Psychologist (2004). p. 20–8.
11.
Lahad M . From Victim to victor: The Development of the BASIC PH Model of Coping and Resiliency. Traumatology (Tallahass Fla) (2017) 23(1):27–34. 10.1037/trm0000105
12.
Barzilay R Moore TM Greenberg DM DiDomenico GE Brown LA White LK et al Resilience, COVID-19-Related Stress, Anxiety and Depression during the Pandemic in a Large Population Enriched for Healthcare Providers. Transl Psychiatry (2020) 10(1):291. 10.1038/s41398-020-00982-4
13.
Leykin D Lahad M Cohen O Goldberg A Aharonson-Daniel L . Conjoint Community Resiliency Assessment Measure-28/10 Items (CCRAM28 and CCRAM10): A Self-Report Tool for Assessing Community Resilience. Am J Community Psychol (2013) 52(3):313–23. Available from. 10.1007/s10464-013-9596-0
14.
Leykin D Lahad M Cohen O Goldberg A Aharonson-Daniel L . Conjoint Community Resiliency Assessment Measure-28/10 Items (CCRAM28 and CCRAM10): A Self-Report Tool for Assessing Community Resilience. Am J Community Psychol (2013) 52(3–4):313–23. 10.1007/s10464-013-9596-0
15.
Hobfoll SE . Conservation of Resources A New Attempt at Conceptualizing Stress (1989).
16.
Galea S Ahern J Resnick H Kilpatrick D Bucuvalas M Gold J et al Psychological Sequelae of the September 11 Terrorist Attacks in New York City. N Engl J Med (2002) 346:982–7. 10.1056/NEJMsa013404
17.
Wells JD Hobfoll SE Lavin J . When it rains, it Pours: The Greater Impact of Resource Loss Compared to Gain on Psychological Distress. Pers Soc Psychol Bull (1999) 25(9):1172–82. 10.1177/01461672992512010
18.
Mao Y He J Morrison AM Andres Coca-Stefaniak J . Effects of Tourism CSR on Employee Psychological Capital in the COVID-19 Crisis: from the Perspective of Conservation of Resources Theory. Curr Issues Tourism (2021) 24(19):2716–34. 10.1080/13683500.2020.1770706
19.
Sun S Zhang SX Jahanshahi AA Jahanshahi M . Drilling under the COVID-19 Pandemic: A Diary Study of Professional Football Players’ Mental Health and Workout Perforance. Stress Health (2022) 38(1):3–18. 10.1002/smi.3059
20.
Chwaszcz J Palacz-Chrisidis A Wiechetek M Bartczuk RP Niewiadomska I Wośko P et al The Quality of Life, Resources, and Coping during the First Weeks of the COVID-19 Pandemic in People Seeking Psychological Counselling before the Pandemic. Int J Occup Med Environ Health (2021) 34(2):275–87. 10.13075/ijomeh.1896.01700
21.
Wanberg CR Csillag B Douglass RP Zhou L Pollard MS . Socioeconomic Status and Well-Being during COVID-19: A Resource-Based Examination. J Appl Psychol (2020) 105:1382–96. 10.1037/apl0000831
22.
Eysenbach G . Improving the Quality of Web Surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res (2004) 6(3):e34. 10.2196/jmir.6.3.e34
23.
Hobfoll SE Lilly RS . Resource Conservation as a Strategy for Community Psychology. J Community Psychol (1993) 21(2):128–48. 10.1002/1520-6629(199304)21:2<128::aid-jcop2290210206>3.0.co;2-5
24.
Weathers FW Litz BT Herman DS Huska JA Keane TM . The PTSD Checklist (PCL): Reliability, Validity, and Diagnostic Utility.
25.
Foa EB McLean CP Zang Y Zhong J Powers B Kauffman BY et al Psychometric Properties of the Posttraumatic Diagnostic Scale for DSM–5 (PDS–5). Psychol Assess (2016) 28(10):1166–71. 10.1037/pas0000258
26.
Kroenke K Spitzer RL Williams JBW . The PHQ-9 Validity of a Brief Depression Severity Measure.
27.
Goral A Lahad M Aharonson-Daniel L . Differences in Posttraumatic Stress Characteristics by Duration of Exposure to Trauma. Psychiatry Res (2017) 258:101–7. 10.1016/j.psychres.2017.09.079
28.
Bareket-Bojmel L Shahar G Margalit M . COVID-19-related Economic Anxiety Is as High as Health Anxiety: Findings from the USA, the UK, and Israel. Int J Cogn Ther (2020) 14:566–74. 10.1007/s41811-020-00078-3
29.
Spielberger CD Gorsuch RL Luchene RE . State-trait Anxiety Inventory for Adults. Redwood City, CA: Mind-Garden (1983).
30.
Russell D Peplau LA Cutrona CE . The Revised UCLA Loneliness Scale: Concurrent and Discriminant Validity Evidence. J Pers Soc Psychol (1980) 39:472–80. 10.1037//0022-3514.39.3.472
31.
Connor KM Davidson JRT . Development of a New Resilience Scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety (2003) 18(2):76–82. 10.1002/da.10113
32.
McDowell CP Herring MP Lansing J Brower CS Meyer JD . Associations between Employment Changes and Mental Health: US Data from during the COVID-19 Pandemic. Front Psychol (2021) 631510. 10.3389/fpsyg.2021.631510
33.
Bonanno GA Galea S Bucciarelli A Vlahov D . What Predicts Psychological Resilience after Disaster? the Role of Demographics, Resources, and Life Stress. J Consult Clin Psychol (2007) 75(5):671–82. 10.1037/0022-006X.75.5.671
34.
Mojtahedi D Dagnall N Denovan A Clough P Hull S Canning D et al The Relationship between Mental Toughness, Job Loss, and Mental Health Issues during the COVID-19 Pandemic. Front Psychiatry (2021) 607246. 10.3389/fpsyt.2020.607246
35.
Fardin MA . COVID-19 Epidemic and Spirituality: A Review of the Benefits of Religion in Times of Crisis. Jundishapur J Chronic Dis Care (2020) 9(2). 10.5812/jjcdc.104260
36.
Lucchetti G Góes LG Amaral SG Ganadjian GT Andrade I Almeida POde A et al Spirituality, Religiosity and the Mental Health Consequences of Social Isolation during Covid-19 Pandemic. Int J Soc Psychiatry (2021) 67(6):672–9. 10.1177/0020764020970996
37.
Walsh F . Loss and Resilience in the Time of COVID-19: Meaning Making, Hope, and Transcendence. Fam Process (2020) 59(3):898–911. 10.1111/famp.12588
38.
Ameis SH Lai MC Mulsant BH Szatmari P . Coping, Fostering Resilience, and Driving Care Innovation for Autistic People and Their Families during the COVID-19 Pandemic and beyond. Mol Autism (2020) 11(1):61–9. 10.1186/s13229-020-00365-y
39.
González-Sanguino C Ausín B Castellanos MÁ Saiz J López-Gómez A Ugidos C et al Mental Health Consequences during the Initial Stage of the 2020 Coronavirus Pandemic (COVID-19) in Spain. Brain Behav Immun (2020) 87:172–6. 10.1016/j.bbi.2020.05.040
40.
Vishnevsky T Cann A Calhoun LG Tedeschi RG Demakis GJ . Gender Differences in Self-Reported Posttraumatic Growth: a Meta-Analysis. Psychol Women Q (2010) 34. Wiley Periodicals, Inc.
41.
Hobfoll SE . The Psychology and Philosophy of Stress. Springer Science & Business Media (2004). Google Scholar [Internet]. [cited 2021 Oct 26]. Available from: https://scholar.google.com/scholar?hl=en&as_sdt=0%2C5&q=Hobfoll%2C+S.+E.+The+psychology+and+philosophy+of+stress%2C+culture%2C+and+community.+Plenum+Press.&btnG=.
42.
Dahlberg L . Loneliness during the COVID-19 Pandemic. Aging Ment Health (2021) 25(7):1161–64. 10.1080/13607863.2021.1875195
43.
Mayer CH Daphna-Tekoah S Braun-Lewensohn O Abu-Kaf S Kalagy T . Hope and Resilience during a Pandemic Among Three Cultural Groups in Israel: The Second Wave of Covid-19. Front Psychol (2021) 12:637349. [Internet]. 10.3389/fpsyg.2021.637349
44.
Wang C Chudzicka-Czupała A Tee ML Inmaculada López Núñez M Tripp C Fardin MA et al A Chain Mediation Model on COVID-19 Symptoms and Mental Health Outcomes in Americans. Asians and Europeans. 10.1038/s41598-021-85943-7
45.
Lorente L Vera M Peiró T . Nurses´ Stressors and Psychological Distress during the COVID-19 Pandemic: The Mediating Role of Coping and Resilience. J Adv Nurs (2021) 77(3):1335–44. 10.1111/jan.14695
46.
Tedeschi RG Calhoun LG Posttraumatic Growth: Conceptual Foundations and Empirical Evidence, 15. Lawrence Erlbaum Associates. Inc. Psychological Inquiry (2004).
47.
Hasanah VR Boriboon G Jubaedah Y Wulandari H . Analysis of the Resilience Conditions of Individual, Family, and Community during the Covid-19 Pandemic. J Nonformal Edu (2021) 7(1):94–102. 10.15294/jne.v7i1.27853
48.
Digital. Israel — Data Reportal – Global Digital Insights (2022). [Internet]. [cited 2022 Apr 25]. Available from: https://datareportal.com/reports/digital-2022-israel.
49.
Midgam Panel. Midgam Project Web Panel. [Internet]. [cited 2022 May 14]. Available from: http://www.midgampanel.com/research/en/index.asp.
50.
Botosh N Goldshmidt R Ezenkot M . Fiber-optic and Fifth-Generation Internet Infrastructures - Economic Benefits and Policy-Making Tools (Hebrew). [Internet]. Jerushalem. Available from: www.knesset.gov.il/mmm (Accessed June 27, 2022).
51.
Schaurer I Weiß B . Investigating Selection Bias of Online Surveys on Coronavirus-Related Behavioral Outcomes. Surv Res Methods (2020) 14(2):103–8.
Summary
Keywords
loneliness, COVID-19, resilience, stress, Conservation of Resources theory, personal resilience, community resilience CCRAM, traumatic symptoms
Citation
Egozi Farkash H, Lahad M, Hobfoll SE, Leykin D and Aharonson-Daniel L (2022) Conservation of Resources, Psychological Distress, and Resilience During the COVID-19 Pandemic. Int J Public Health 67:1604567. doi: 10.3389/ijph.2022.1604567
Received
31 October 2021
Accepted
03 August 2022
Published
31 August 2022
Volume
67 - 2022
Edited by
Franco Mascayano, New York State Psychiatric Institute (NYSPI), United States
Reviewed by
Ricardo Rafael, Rio de Janeiro State University, Brazil
Pier Luigi Sacco, University of Studies G.d’Annunzio Chieti and Pescara, Italy
Updates
Copyright
© 2022 Egozi Farkash, Lahad, Hobfoll, Leykin and Aharonson-Daniel.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hadas Egozi Farkash, hadaseg@post.bgu.ac.il; Mooli Lahad, mooli.lahad@icspc.org
This Original Article is part of the IJPH Special Issue “The Impact of the COVID-19 Pandemic on Mental Health”
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.