Abstract
Objectives: To record the prevalence and risk factors of substance use amongst homeless persons during the COVID-19 pandemic.
Methods: The ECHO study consisted in two independent cross-sectional waves of data collection in the regions of Paris, Lyon, and Strasbourg during the Spring of 2020 (n = 530) and 2021 (n = 319). Factors associated with substance use were explored using generalised logistic regression models.
Results: The most prevalent substance used was tobacco (38%–43%), followed by alcohol (26%–34%). The use of both substances positively associated with each other, although risk factors varied depending on the substance. The only factors consistently associated with alcohol and tobacco use were being male, exposure to theft/assault and participants’ region of origin. Whilst the rate of tobacco use was relatively stable between Spring 2020 and 2021, alcohol use was more common in 2021.
Conclusion: These findings highlight a high prevalence of substance use amongst homeless persons. People experiencing homelessness face specific challenges in the context of the pandemic, alongside greater vulnerability to illness and low healthcare access, therefore the need to improve prevention and support services for substance abuse within this population is vital.
Introduction
Evidence suggests that the COVID-19 pandemic has significantly impacted rates of substance use in the general population [1–4]. However, these changes are complex and ongoing. On the one hand, environmental stress is a known risk factor for substance use disorders [5], with increases in alcohol and tobacco consumption recorded during natural disasters [6, 7] terrorist incidents [8, 9] and humanitarian conflicts [10, 11]. The stress of the COVID-19 pandemic, alongside associated increases in social isolation [12], may have therefore contributed to increasing rates of substance use [13]. COVID-19 preventative measures, such as lockdowns, staff shortages and reduced opening hours, were also predicted to disrupt access to support and drug services [14–16]. Nevertheless, the pandemic is likely to have decreased drug availability, due to reduced drug trafficking and market shortages [17], alongside reducing opportunities for consumption, with users themselves having less freedom of movement, disrupted income and fewer social interactions. For these reasons, the effect of the pandemic on substance use warrants investigation.
One of the populations most vulnerable to substance use is those without stable housing. Government estimates found the number of homeless people in Metropolitan France rose from 93,000 in 2001 to 141,500 in 2012 [18]. And within the Paris area, an estimated 29% of homeless persons suffer from addiction, with 18% of those surveyed regularly consuming at least one illegal substance [19]. In parallel, rates of frequent smoking are significantly higher amongst homeless persons (∼84%) than in the French general population (∼25%) [20, 21]. Considering that smoking is the leading cause of preventable death in Europe [22–24], associated strongly to social inequalities, examining the extent to which patterns of tobacco use have evolved in the context of the COVID-19 pandemic among homeless groups is of public health interest. Not only are homeless persons more susceptible to tobacco-related illness and subsequent fatality [25–27], but the financial burden of addiction may also prolong financial insecurity and therefore housing instability [22].
Many of the factors explaining the association between homelessness and substance use are likely to have been impacted by the COVID-19 pandemic. Not only are periods of homelessness often accompanied by increased stress, but fewer supporting factors remain. Financial difficulties, increased isolation and social stigma all inhibit resilience, leaving those experiencing homeless increasingly vulnerable to addiction. Studies have shown that housing instability and food insecurity increased the risk of turning to substance use to cope with depression and anxiety during the pandemic [1, 28]. Moreover, government policies surrounding housing have greatly fluctuated since the initial outbreak of COVID-19, and homeless persons have had to recurrently adapt. Qualitative studies have shown that, whilst temporary shelters created as a COVID-19 preventative measure may have had an initially positive effect on addictive substance use, the subsequent eviction of homeless persons resulted in them either resuming or increasing their drug consumption [29]. Findings taken from multiple time-points throughout the duration of the pandemic are therefore necessary to both understand the permanence of its impact and help inform public health measures.
Here we present data on the prevalence and associated risk factors for tobacco and alcohol use amongst persons experiencing homelessness during the COVID-19 pandemic. Importantly, the ECHO study spans two distinct periods: the onset of the pandemic (Spring, 2020) and the following Spring (2021). Through this, we were able to collect data from persons sleeping rough as well as those living in shelters, thereby providing valuable information on a group for which evidence regarding the experience of the COVID-19 pandemic is currently limited.
Methods
Study Design
The ECHO study is a cross-sectional investigation conducted amongst persons without stable housing in France. The findings presented here are based on two waves of data collection, taken during the Spring of 2020 (02/05/20–07/06/20) (W1) and 2021 (09/03/21–31/05/21) (W2). Whilst the samples for each wave were distinct, the methodology was generally consistent between the two. Participants were recruited from shelters located in the regions of Paris (W1 n = 12; W2 = 9), Lyon (W1 = 5; W2 = 10) and Strasbourg (W1 = 1). Recruitment for W2 also incorporated day centres (n = 7), allowing the inclusion of those sleeping rough. Interviews were conducted both in person (W1 = 98%; W2 = 100%) or by telephone (W1 = 2%), in French, English or participants’ chosen language, with the help of independent interpreters, to minimise bias due to language barriers (W1 = 33%, W2 = 13%). Over 20 languages were used, most frequently Arabic, Pashto and Dari. Participants were excluded if aged under 18 years, significantly inebriated or presenting cognitive disorders that prevented consent. The study protocol was approved by the Ethical Research Committee of the University of Paris (CER-2020-41).
Assessment of Substance Use
The assessment of both substance use and risk factors was done via direct, one-on-one interviews with participants. All questions were based on a pre-determined, quantitative questionnaire, designed in each study wave by the ECHO research team. Whilst the questionnaire could have been self-administered, interviews were conducted to reduce exclusion based on participants’ language or literacy. In both study waves, participants were asked to report their current use of tobacco and alcohol on a 3-point scale ranging from “every day,” “sometimes”; or “no”. For multivariate analyses, “every day” and “sometimes” were combined, generating two categories for current use (yes/no). As a secondary objective of this study, participants also reported cannabis use on the same scale, however, due to its illegality, a “does not wish to answer” option was available in W1. For W2, questions on substance use were exclusive to the supplementary questionnaire, and refusal to answer was registered as missing data.
Risk Factors
Factors considered potentially relevant to patterns of substance use were the following: age (18–29; 30–49; 50 + years), sex (male; female), partnership status (stable partner; single), family status (no children; living with children; has children but living separately), educational level (no school/incomplete primary education; primary/high school education; College/higher education), employment (none; only before lockdown; both before and during lockdown), duration of stay in France (<1 year; 1–5 years; 5+ years, including French natives), French language aptitude (low; moderate/fluent), administrative status (French native; residence permit holder; asylum seeker; no residence permit; other), health insurance (yes; no), chronic illness (yes; no), food insecurity (yes; no), feelings of safety (yes; no), exposure to theft or assault during the first lockdown (yes; no), contact with friends/family (yes; no), and participants’ previous accommodation (centre/association; unestablished shelter e.g., camps, squats; street; friends/family/other).
French language aptitude was calculated from the sum score of self-reported French speaking, reading and writing ability, each rated on a 4-point Likert scale. Participants’ degree of loneliness was measured based on the UCLA loneliness scale [30]. Health literacy was calculated as a sum of participants’ scores to either the fifth (W1) or fourth and seventh (W2) dimensions of the Health Literacy Questionnaire [31], with the threshold between low and high set as an average agreement of ≤50% for W1 and ≤33% for W2. Depression was assessed via the nine-item Patient Health Questionnaire (PHQ-9) in W1 (cut-off score 10 [32]), and the four-item PHQ-4 in W2 (cut-off score 5). Both are validated for use in multicultural settings [33, 34]. Finally, participants region of origin was divided into France; Europe excluding France; the Middle East; North Africa; Sub-Saharan Africa; and Other (categories defined in Supplementary Table S1).
Data Analyses
To identify factors associated with alcohol and tobacco use, the following approach was implemented. First, differences in the prevalence of substance use between Spring 2020 and 2021 were examined using Chi-square (X2) analysis. We then tested associations with factors considered relevant a priori, in relation to substance use, using generalised logistic regression models, implementing separate models for each study wave. Missing covariate values were imputed using Multivariate Imputation by Chained Equations (MICE) [35].
Participants from American, South-East Asian, and Western Pacific regions were excluded due to insufficient sample size (W1 n = 5; W2 = 12). Variables included in multivariate statistical models were determined via univariate X2 analyses, as supported by Hosmer and Lemeshow [36, 37]. An 80% confidence limit was used [38], to prevent the arbitrary exclusion of important variables [39, 40]. For measures of prevalence, cannabis use was also included, allowing us to further investigate interactions between respective substances.
All data analyses were performed on R Version 4.1.1 [41, 42].
Results
Sample
Overall, 1564 persons were invited to take part in the ECHO study. Following participant refusal or unavailability, 535 participants were interviewed in Spring 2020, of which 530 had sufficient data on substance use, and 523 in Spring 2021, of which 319 had sufficient data on substance use. Demographic information on both study samples is available in Table 1.
TABLE 1
| Spring 2020 (n = 530) | Spring 2021 (n = 319) | p | |
|---|---|---|---|
| Sex | |||
| Male | 75% (377) | 67% (215) | * |
| Female | 25% (126) | 33% (104) | |
| Age range (years) | |||
| 18–29 | 43% (218) | 23% (73) | *** |
| 30–49 | 42% (209) | 49% (155) | |
| 50+ | 15% (76) | 28% (90) | |
| Partnership status | |||
| Yes, has a stable partner | 37% (178) | 29% (87) | * |
| No stable partner | 63% (306) | 71% (209) | |
| Family status | |||
| No children | 49% (230) | 46% (146) | 0.13 |
| Has children, but not living with them | 30% (143) | 37% (117) | |
| Currently living with their children | 21% (99) | 17% (55) | |
| Highest education level | |||
| No school or incomplete primary education | 29% (143) | 14% (44) | *** |
| Primary or high school education | 54% (269) | 57% (181) | |
| College or higher education | 17% (82) | 29% (93) | |
| Employment status | |||
| Unemployed | 73% (360) | 79% (254) | N/A |
| Employed before lockdown | 20% (97) | 21% (66) | |
| Employed before and during lockdown | 7% (35) | ||
| Perceived food insecurity | |||
| Not food insecure | 62% (307) | 43% (139) | *** |
| Food insecure | 38% (191) | 57% (181) | |
| Accommodation before current centre | |||
| Other centre/charity | 20% (99) | 18% (59) | *** |
| Unestablished shelter/squat | 24% (119) | 2% (6) | |
| Street | 41% (207) | 73% (234) | |
| Friends/family/other | 16% (78) | 7% (21) | |
| Time since arrival to centre | |||
| Less than 1 month | 53% (260) | — | N/A |
| 1 month–1 year | 29% (142) | — | |
| Over 1 year | 18% (89) | — | |
| Region of birth | |||
| French native | 11% (57) | 16% (52) | *** |
| Europe (other than France) | 11% (59) | 8% (25) | |
| Middle Easta | 35% (185) | 10% (33) | |
| Northern Africab | 10% (55) | 19% (62) | |
| Sub-Saharan Africa | 31% (162) | 45% (143) | |
| Other | 2% (12) | 2% (5) | |
| Administrative status | |||
| French native | 11% (56) | 16% (52) | *** |
| Residence permit | 23% (117) | 30% (97) | |
| Asylum seeker | 31% (156) | 5% (16) | |
| No residence permit | 26% (128) | 43% (139) | |
| Other | 8% (42) | 5% (16) | |
| Health status | |||
| Chronic illness (no) | 74% (370) | 47% (150) | *** |
| Chronic illness (yes) | 26% (127) | 53% (167) | |
| Healthcare | |||
| Medically insured/coveredc | 68% (343) | 87% (278) | *** |
| Uninsured | 32% (159) | 13% (40) | |
| Health literacy | |||
| Low | 15% (71) | — | N/A |
| High | 85% (396) | — | |
| Symptoms of depression | |||
| No | 70% (352) | 69% (220) | 0.67 |
| Yes | 30% (148) | 31% (100) | |
| French aptitude (self-reported) | |||
| Low | 54% (286) | 10% (33) | *** |
| Moderate /Fluent | 46% (239) | 90% (286) | |
| Trusts government information on COVID-19 | |||
| Yes | 78% (365) | 63% (185) | *** |
| No | 22% (100) | 38% (111) | |
| Duration of stay in France | |||
| <1 year | 43% (222) | 20% (63) | *** |
| 1–5 years | 31% (159) | 29% (92) | |
| 5 + years | 27% (139) | 51% (163) | |
| Loneliness | |||
| Not lonely, both now and before | 32% (161) | 22% (93) | *** |
| As lonely as before | 15% (76) | 17% (69) | |
| More lonely than before | 37% (186) | 30% (126) | |
| Less lonely than before | 15% (77) | 31% (130) | |
| Social contact | |||
| In regular contact with friends and family | 88% (435) | — | N/A |
| No contact with friends and family | 12% (62) | — | |
| Safety | |||
| Has felt safe since lockdown | 71% (354) | — | N/A |
| Has felt unsafe since lockdown | 29% (147) | — | |
| Exposure to assault | |||
| No theft or assault since lockdown | 88% (438) | — | N/A |
| Theft or assault since lockdown | 12% (58) | — | |
Demographic characteristics of study participants. All p values shown are based on Chi-Square (X2) analysis. (France, 2020–2021).
Middle Eastern countries relevant to this sample: Afghanistan, Iran, Iraq, Pakistan, Palestine, Saudi Arabia, Somalia, Sudan.
North African countries relevant to this sample: Algeria, Libya, Morocco, Tunisia.
Including State Medical Assistance (AME) for undocumented migrants.
Rates of Substance Use
Rates of substance use are shown in Table 2. Tobacco was the most commonly used substance in both study waves (42% of participants in Spring 2020; 38% in 2021), followed by alcohol (26%; 34%), and cannabis (10%; 9%). Univariate analyses found tobacco use to be significantly associated with the use of both alcohol (p < 0.001) and cannabis (p < 0.001) in both waves. Alcohol use also significantly associated with cannabis use (p < 0.001).
TABLE 2
| Tobacco % (n) | Alcohol % (n) | Cannabis % (n) | ||||
|---|---|---|---|---|---|---|
| Spring 2020 | Spring 2021 | Spring 2020 | Spring 2021 | Spring 2020 | Spring 2021 | |
| Total users Of which was used… | 42% (223) | 38% (120) | 26% (136) | 34% (109) | 10% (55) | 9% (30) |
| In isolation | 48% (106) | 40% (48) | 31% (42) | 41% (45) | 4% (2) | 0 |
| With tobacco | REF | REF | 69% (94) (p < 0.001) | 57% (62) (p < 0.001) | 95% (52) (p < 0.001) | 93% (28) (p < 0.001) |
| With alcohol | 42% (94) (p < 0.001) | 52% (62) (p < 0.001) | REF | REF | 55% (30) (p < 0.001) | 67% (20) (p < 0.001) |
| With cannabis | 23% (52) (p < 0.001) | 23% (28) (p < 0.001) | 22% (30) (p < 0.001) | 18% (20) (p < 0.001) | REF | REF |
Rates of tobacco, alcohol, and cannabis use amongst study participants during the COVID-19 pandemic during Spring 2020 (n = 530) and 2021 (n = 319). All p values shown are based on univariate regression analysis. (France. 2020–2021).
Differences between rates of substance use between the two study waves are shown in Figure 1. When compared to 2020, alcohol use was more prevalent in 2021 (p < 0.001).
FIGURE 1
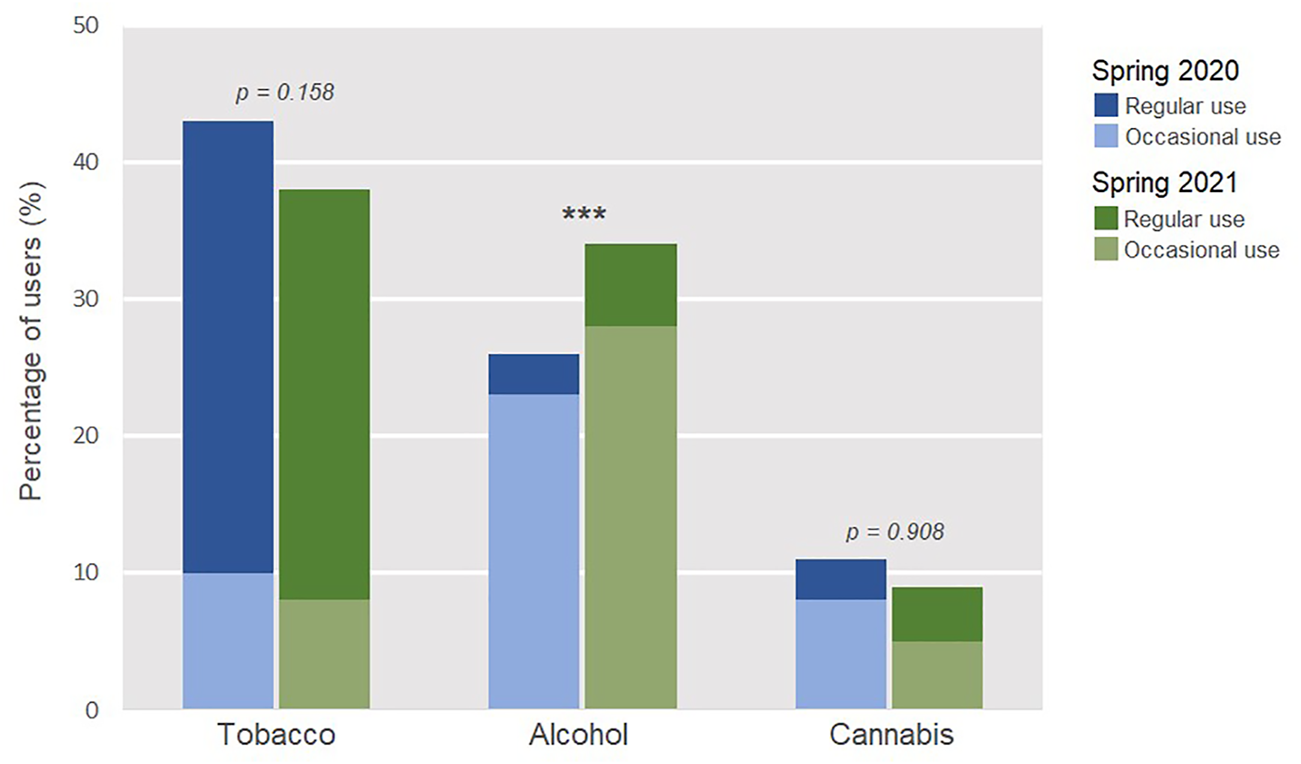
Rates of tobacco, alcohol and cannabis use amongst homeless persons interviewed in the Spring of 2020 (n = 530) and 2021 (n = 319). Chi-Square (X2) analysis. (France. 2020–2021).
Risk Factors of Substance Use
Factors associated with alcohol and tobacco use, determined via multivariate regression, are shown in Table 3. In Spring 2020, characteristics associated with tobacco use were being male (aOR:5.04; 95% CI: 2.43–10.46), not having a stable partner (aOR:2.01; 95% CI: 1.16–3.46), being medically uninsured (aOR:2.10; 95% CI: 1.21–3.64) and exposure to theft or assault (aOR:2.55; 95% CI: 1.32–4.93). Compared to French natives, participants born in the Middle East (aOR:0.43; 95% CI: 0.21–0.88) or Sub-Saharan Africa (aOR:0.22; 95% CI: 0.11–0.41) were less likely to smoke tobacco, whilst those born in other European countries were more likely (aOR:4.54; 95% CI: 2.03–10.14). Participants who had lived in France for more than 5 years were also more likely to smoke than those living in France for less than 1 year (aOR:2.34; 95% CI: 1.03–5.31). In Spring 2021, tobacco use associated with being male (aOR:4.42; 95% CI: 2.09–9.37) and medically uninsured (aOR:2.88; 95% CI: 1.09–7.64).
TABLE 3
| Tobacco | Alcohol | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Spring 2020a | Spring 2021b | Spring 2020a | Spring 2021b | ||||||
| aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | ||
| Sex | Female | 1 | 1 | 1 | 1 | ||||
| Male | 5.04 | 2.43–10.46 | 4.42 | 2.09–9.37 | 3.44 | 1.63–7.25 | 2.53 | 1.26–5.07 | |
| Partnership status | Yes, has a stable partner | 1 | 1 | 1 | 1 | ||||
| No stable partner | 2.01 | 1.16–3.46 | 1.67 | 0.77–3.61 | 1.06 | 0.61–1.85 | 0.96 | 0.46–2.01 | |
| Family status | No children | 1 | 1 | 1 | 1 | ||||
| Has children, but not living with them | 0.97 | 0.53–1.80 | 1.14 | 0.52–2.50 | 1.31 | 0.72–2.38 | 1.07 | 0.50–2.29 | |
| Currently living with their children | 0.59 | 0.24–1.45 | 0.63 | 0.21–1.84 | 1.00 | 0.41–2.45 | 0.65 | 0.24–1.78 | |
| Highest education level | No school/incomplete primary education | 1 | 1 | 1 | 1 | ||||
| Primary or high school education | 1.29 | 0.76–2.19 | 2.24 | 0.85–5.95 | 1.15 | 0.66–2.02 | 3.80 | 1.44–10.00 | |
| College/Higher education | 0.82 | 0.39–1.74 | 1.51 | 0.54–4.22 | 1.47 | 0.69–3.14 | 2.33 | 0.84–6.47 | |
| Age range (years) | 18–29 | 1 | 1 | 1 | 1 | ||||
| 30–49 | 1.33 | 0.78–2.28 | 1.10 | 0.49–2.47 | 1.09 | 0.64–1.86 | 1.87 | 0.86–4.08 | |
| 50+ | 0.67 | 0.28–1.62 | 1.72 | 0.66–4.50 | 0.55 | 0.22–1.36 | 1.59 | 0.63–4.01 | |
| Experiencing food insecurity | No | 1 | 1 | 1 | 1 | ||||
| Yes | 1.01 | 0.63–1.62 | 1.23 | 0.66–2.29 | 1.28 | 0.79–2.07 | 0.81 | 0.45–1.46 | |
| Loneliness | Not lonely (before or after) | 1 | 1 | 1 | 1 | ||||
| As lonely as before | 1.17 | 0.58–2.38 | 0.97 | 0.40–2.37 | 1.23 | 0.61–2.48 | 1.14 | 0.49–2.68 | |
| More | 1.00 | 0.56–1.79 | 0.98 | 0.45–2.12 | 0.99 | 0.54–1.81 | 1.46 | 0.71–3.03 | |
| Less | 0.99 | 0.48–2.04 | 0.84 | 0.26–2.67 | 1.02 | 0.49–2.16 | 1.27 | 0.42–3.82 | |
| Region of birth | French native | 1 | 1 | 1 | 1 | ||||
| Europe (other than France) | 4.54 | 2.03–10.14 | 0.95 | 0.35–2.59 | 1.41 | 0.68–2.93 | 0.66 | 0.24–1.76 | |
| Middle Eastc | 0.43 | 0.21–0.88 | 0.79 | 0.33–1.90 | 0.91 | 0.46–1.82 | 0.61 | 0.24–1.56 | |
| North Africad | 0.88 | 0.43–1.83 | 1.40 | 0.65–3.00 | 0.63 | 0.29–1.37 | 0.24 | 0.11–0.55 | |
| Sub-Saharan Africa | 0.22 | 0.11–0.41 | 0.26 | 0.13–0.52 | 1.11 | 0.60–2.03 | 0.75 | 0.39–1.45 | |
| Time since arrival to France | Less than 1 year | 1 | 1 | 1 | 1 | ||||
| 1–5 years | 1.71 | 0.95–3.09 | 0.70 | 0.26–1.91 | 1.07 | 0.59–1.92 | 1.25 | 0.46–3.42 | |
| 5+ years | 2.34 | 1.03–5.31 | 1.19 | 0.44–3.23 | 1.11 | 0.48–2.56 | 1.83 | 0.67–5.00 | |
| Healthcare | Medically insured/coverede | 1 | 1 | 1 | 1 | ||||
| Uninsured | 2.10 | 1.23–3.60 | 2.88 | 1.09–7.64 | 1.11 | 0.65–1.92 | 1.34 | 0.53–3.34 | |
| Symptoms of depression | no | 1 | 1 | 1 | 1 | ||||
| Yes | 1.07 | 0.64–1.80 | 1.26 | 0.66–2.42 | 1.66 | 1.00–2.75 | 0.77 | 0.41–1.45 | |
| Administration status | French native | 1 | 1 | 1 | 1 | ||||
| Residence permit | 0.59 | 0.32–1.08 | 0.88 | 0.44–1.78 | 1.01 | 0.55–1.83 | 0.69 | 0.35–1.35 | |
| Asylum seeker | 0.87 | 0.45–1.66 | 0.81 | 0.21–3.04 | 0.92 | 0.49–1.75 | 0.28 | 0.06–1.26 | |
| No residence permit | 0.89 | 0.46–1.72 | 0.59 | 0.32–1.09 | 0.81 | 0.42–1.56 | 0.62 | 0.34–1.15 | |
| Other | 0.82 | 0.37–1.83 | 0.66 | 0.20–2.15 | 1.19 | 0.55–2.60 | 0.62 | 0.19–2.03 | |
| Trusts government information on COVID-19 | Yes | 1 | 1 | 1 | 1 | ||||
| No | 1.38 | 0.82–2.33 | 1.02 | 0.56–1.85 | 1.40 | 0.83–2.36 | 1.44 | 0.81–2.57 | |
| Exposure to assault | No theft or assault since lockdown | 1 | 1 | 1 | 1 | ||||
| Theft or assault since lockdown | 2.55 | 1.32–4.93 | — | — | 1.83 | 1.01–3.31 | — | ||
| Accommodation before current | Other organised center | 1 | 1 | 1 | 1 | ||||
| Unestablished shelter | 0.55 | 0.28–1.10 | 0.43 | 0.07–2.53 | 0.81 | 0.41–1.63 | 0.23 | 0.04–1.43 | |
| Street | 0.59 | 0.31–1.11 | 0.86 | 0.41–1.81 | 0.77 | 0.40–1.46 | 0.83 | 0.39–1.75 | |
| Friends/family/other | 0.60 | 0.27–1.31 | 0.35 | 0.09–1.40 | 1.01 | 0.47–2.16 | 0.98 | 0.25–3.84 | |
Risk factors of tobacco and alcohol use amongst study participants. Multivariate, logistic regression models (aOR, 95% CI). (France. 2020–2021).
Values with statistical significance shown in bold.
n = 530.
n = 319.
Middle Eastern countries relevant to this sample: Afghanistan, Iran, Iraq, Pakistan, Palestine, Saudi Arabia, Somalia, Sudan.
North African countries relevant to this sample: Algeria, Libya, Morocco, Tunisia.
Including State Medical Assistance (AME) for undocumented migrants.
Characteristics associated with alcohol use in Spring 2020 were being male (aOR:3.44; 95% CI: 1.63–7.25), exposure to theft or assault (aOR:1.83; 95% CI: 1.01–3.31) and experiencing symptoms of depression (aOR: .66; 95% CI: 1.00–2.75). In Spring 2021, alcohol use associated with being male (aOR:2.53; 95% CI: 1.26–5.07) and having had primary or high school education (aOR:3.80; 95% CI: 1.44–10.00) as opposed to no schooling. Compared to French natives, North African participants were less likely to drink alcohol (aOR:0.24; 95% CI: 0.11–0.55).
Discussion
This study aimed to describe the use of psychoactive substances amongst persons with unstable housing during the course of the COVID-19 pandemic. Participants were most likely to use tobacco (38–43%), followed by alcohol (26–34%). The only factor consistently associated with use of both tobacco and alcohol in both waves was being male. Tobacco use was also associated with exposure to theft or assault during the first lockdown, being medically uninsured, living in France for over 5 years, and not having a stable partner. For alcohol use, risk factors were exposure to theft or assault, having symptoms of depression and having primary or secondary school education (as opposed to no schooling or incomplete primary education). Participants migrating from Europe were also more likely to smoke tobacco, whilst those born in the Middle East or Sub-Saharan Africa significantly less, and those from North Africa were less likely to drink alcohol.
Rates of Substance Use
Tobacco was the most frequent substance used in both ECHO study waves. Cross-sectional data on the French general population during Spring 2020 saw 21% were tobacco smokers (occasional and regular) [4]. Our findings then suggest a rate amongst homeless persons roughly double that of the general population. Considering that homeless persons present higher rates of medical comorbidities [25, 26, 45] and are therefore more at risk of tobacco-related illness or fatality [26, 46], these findings are cause for concern. Additionally, despite universal health care, socioeconomically disadvantaged groups are less likely to have access to smoking cessation programs, leading to large inequalities in smoking which appear to have increased in the context of the COVID-19 pandemic [47]. Regarding alcohol, rates within ECHO were also higher than national levels (17% regular drinkers) [48].
Differences in Behaviour Across the Pandemic
Whilst the rates of tobacco use were similar between Spring 2020 and 2021 (38%–43%), alcohol use was more frequent amongst participants in 2021 (34%) than 2020 (26%). Several key factors may account for the higher rate of alcohol use seen in Spring 2021; first, during the initial lockdown period, restrictions may have decreased the availability of alcohol, both physically (bar/shop closures; exit permits) and financially (reduced hours; job loss) [17]. Many of these restrictions were either lifted or relaxed by Spring 2021, during which France experienced its third lockdown. This can be seen, for example, in the rate of employment. Among the ECHO population surveyed in Spring 2020, 93% were unemployed, compared to just 79% in Spring 2021. Whilst employment status did not associate with alcohol use in our study population, nor amongst non-homeless populations during the pandemic [49], factors associated with fewer restrictions (such as increased socialisation and disposable income) may have enabled more frequent drinking [50]. The higher rates of alcohol use amongst those surveyed in 2021 may also be specific to each groups’ respective living situation. All participants in the first wave were housed in temporary shelter, which may have had a positive influence on alcohol consumption. A stable, communal living environment can provide greater support than is often available for those sleeping rough, alongside that from social workers specifically hired by the organisations themselves [51]. On-site case-management and social support, given through the Housing First initiative, has been shown to reduce alcohol-use amongst previously-unsheltered homeless persons [52, 53]. Furthermore, qualitative findings collected during April–August 2020 show homeless-centre users found support services acted as a ‘lifeline’ during the pandemic, providing invaluable stability during a time of such disruption [54]. In comparison, the ECHO sample interviewed in Spring 2021 had a variety of living situations. Alongside a reduced level of support, this may elevate rates of alcohol use bidirectionally: those who drink may struggle more to find or maintain shelter, whilst those without temporary shelter may then be more likely to drink [55] Moreover, the discontinuation of the housing services initially provided in response to the pandemic (of which the first-wave participants benefitted) may have triggered alcohol consumption. In support of this, Scallan et al. [29] found disruptions to emergency housing, provided temporarily during the pandemic, resulted in increased addictive substance use. Together, our findings may then indicate the importance of a consistent, supportive living environment for the promotion of healthy behaviours, particularly following the fluctuations in housing caused by the pandemic.
Several of these factors, however, would also apply to tobacco, despite no significant difference being noted. Our findings also contrast with those from the general French population, which found tobacco smokers were more likely to report an increase in use (27%) since the onset of the pandemic, whilst alcohol use generally decreased—at least in frequency [52]. This may then indicate that alcohol drinking was a more popular coping mechanism for the progressive, long-term strain of the pandemic amongst homeless populations [54]. In support of this, drinking to cope during the pandemic was seen to associate with depression [49], for which the ECHO population showed higher-than-national levels [55]. Alcohol use within both study populations may have also depended more on social liberty (the ability to socialise; beg for money) and financial security than tobacco. In fact, several studies showed social isolation was not a significant risk factor for changing tobacco consumption during the pandemic, with one even finding it to be the most popular reason for decreasing cigarette use [56, 57].
Factors Associated With Substance Use
Gender and Assault
Among risk factors of substance use examined in our study, being male was the only factor associated with both alcohol and tobacco use across both waves. Accordingly, cross-sectional data collected in 2009 from homeless persons in Paris found men were more likely to consume at least one recreational drug, and be dependent on alcohol [19]. In contrast, rates of smoking within the general French population show no significant difference between men and women [4], with Canadian findings also showing that the use of substances as a coping mechanism during the pandemic did not differ by gender [58]. This association may then be more specific to homeless persons. However, these results do not mean that homeless women are not vulnerable to substance abuse [59]. In our sample, the only other factor associated with both tobacco and alcohol use was an exposure to theft or assault. Whilst previous literature supports this [60], studies suggest the association between assault and substance use is stronger amongst women [61, 62]. Considering homeless women also present a far greater risk for assault than homeless men [63, 64], this link between substance use and assault should be kept as an important consideration for residents of women’s shelters. In particular, women are disproportionately affected by intimate partner violence (IPV) than men [65, 66]. This is particularly relevant, as not only are both poverty and homelessness risk factors for IPV, but rates have climbed significantly since the onset of the pandemic [65, 67].
Migrant Status
The lower rate of alcohol use observed amongst participants born in Northern Africa may result from the entirety of this group having migrated from Muslim-majority countries, where alcohol consumption is actively discouraged [68]. Nevertheless, reports have shown that migrants from Muslim-majority countries who do drink alcohol are more likely to engage dangerous drinking-behaviours [69], so these results should be interpreted with caution. For tobacco use, Middle Eastern or Sub-Saharan African participants showed significantly lower rates than French natives, whilst those born in Europe showed rates significantly higher. This is in line with pre-pandemic findings, which showed migrants from sub-Saharan Africa to be significantly less likely to smoke than French nationals [70]. This may also explain the association between smoking and the amount of time participants had spent in France; those who had lived in France for over 5 years were more likely to smoke than new arrivals (<1 year), therefore French natives may have partly driven these results.
Another explanation for the relationship between migrants’ region of origin and substance use may be the motives for migration. These are likely to depend on the region itself [71, 72], and may contribute differentially to one’s tendency to seek external coping mechanisms. For example, post-traumatic stress disorder (PTSD) is a known trigger for substance abuse [73], and is also established to result from experiences of migration [74]. Persons migrating due to war or domestic violence may then be at greater risk for addictive behaviours. In support of this, research has shown that levels of PTSD among homeless migrant mothers in Paris depended significantly on country of origin and motivation for departure [75].
Regardless, the higher rate of smoking seen amongst those migrating from Europe is still a cause for concern. Migrant populations have both lower rates of medical insurance and greater difficulties accessing medical care [76]. Moreover, a lack of medical insurance was also seen to be a risk factor for tobacco use in both waves. The COVID-19 pandemic is likely to have accentuated these inequalities further. Findings from the UK show the shift to more virtual healthcare during the pandemic exacerbated barriers to health-care access amongst migrants [77, 78]. Within homeless populations, those migrating from Europe may then be even more vulnerable to tobacco-related illness and mortality.
Mental Health
Symptoms of depression were associated with a higher likelihood of alcohol use during the early stages of the pandemic in our study. During this period, depression was also found to be associated with increased alcohol consumption in the general population [4]. Within the ECHO study sample, both waves showed rates of depression (30–31%) higher than national averages (∼20%) [79]. Serious mental disorders are known risk factors for homelessness, propagating the associated issues with employment and access to medical care and social support [80, 81]. Even pre-pandemic, a Parisian study found half of homeless persons surveyed with psychotic disorders were addicted to at least one drug, with 30% alcohol-dependent [19]. Moreover, 68% of ECHO study participants in Spring 2020 and 78% in 2021 reported feeling some degree of loneliness, an established long-term risk factor for depression [82, 83] and addictive behaviours [84]. These figures align with findings that loneliness increased during the COVID-19 pandemic especially amongst those with low socioeconomic status [85, 86].
Wider Implications
These results may be useful to guide both the prevention and treatment of substance abuse in homeless populations following the COVID-19 pandemic. Existing preventative measures for addictive behaviour might not be effective; studies have shown that whilst homeless adults who have experienced more frequent homeless episodes have higher odds of receiving anti-smoking support, they show lower rates of quitting [26]. Moreover, several of the risk factors identified, such as exposure to assault and symptoms of depression, have also increased in prevalence during the pandemic [66, 67, 87, 88].
Whilst risk factors associated with substance use varied between tobacco and alcohol, the use of different substances strongly associated with each other. Research suggests many of the genetic and environmental vulnerabilities towards using different addictive substances are shared [89, 90], therefore the risk factors identified for tobacco and alcohol use within this sample may remain pertinent to other substances. Considering the concurrent use of multiple substances also increases the chance of subsequent injury [91], interventions considering all potential risk factors may be more successful in preventing substance-related morbidity and mortality.
Limitations and Strengths
Our study has several limitations which need to be addressed. First, the primary focus of the ECHO study was not to investigate substance use. Therefore, our assessment was relatively limited, comprising of one multiple-choice measure per substance. Despite this, the more generalised questionnaire design allowed us to account for a wider range of variables in the limited interview time available, often not examined in relation to substance use. Secondly, ECHO comprises two cross-sectional waves of data collection, based on separate samples. This therefore limits our assessment of longitudinal patterns of substance use. The most significant difference between the two study waves was participants’ housing situation; whilst wave one included only persons living in temporary accommodation at the time of investigation, wave two recruited persons from a wider range of situations. However, it is important to note that during the Spring of 2020, France had an active policy of providing temporary shelter to all persons sleeping rough, in order to limit the propagation of COVID-19. This sample may thus be more reflective of the general homeless population than those typically residing in temporary accommodation. In support of this, 41% of wave one participants were living on the street before their current shelter, thereby indicating the inclusion of various experiences of homelessness.
Finally, this study may be biased due to our reliance on participants’ self-reports. In comparison to biological markers, self-reports are known to generate underestimations of substance use [43]. Moreover, within our study, both data collection points occurred during Ramadan, a month associated with abstinence from drugs within the Muslim community. Although no data on participants’ religious practice were collected, 61% of our sample originated from a predominantly Muslim country. If practising Islam, these participants are then potentially more likely to have both reduced their consumption during this period, and under-report their levels of use due to social or cultural desirability bias [44]. This tendency towards underestimation may have also been accentuated by the precariousness of our study population’s accommodation, as participants may have feared that reporting recreational drug use would have jeopardised their right to shelter. To counteract this, before every interview, participants were reminded that their responses were anonymous and would not impact their right to accommodation, and that they were free to refuse any question.
Nevertheless, our study has numerous strengths which support the validity of our findings. The data available on substance use within homeless populations is limited, and whilst our findings cannot be extrapolated to pre- or post-pandemic periods, factors associated with substance use may remain relevant. Moreover, the inclusion of multiple different substances within the same sample provides a particularly valuable, often-unreported comparison between substances with consistent demographics. Our study was conducted in two large metropolitan regions of France, thereby limiting the role of specific contextual factors on the selection of the homeless population living in accommodation centres. Finally, we interviewed participants who could not speak French or English, through professional interpreters, making it possible to collect data among recent migrants who constitute the largest share of the current homeless population in France.
Conclusion
Our study shows elevated rates of substance use among homeless persons during the COVID-19 pandemic. Tobacco was the most commonly used substance, with rates roughly double that of the general population. The use of different substances also positively associated with each other, with the majority of users using more than one substance. Factors associated with tobacco and alcohol use varied, except being male and exposed to theft or assault, which increased the risk of using both substances. Higher rates of alcohol use were seen in the later stage of the pandemic, which may associate with participants’ greater housing insecurity during this wave. Together these findings provide valuable information on those most vulnerable to substance abuse within homeless populations. Considering the increased risk for both alcohol and tobacco-related injury amongst vulnerable persons, adapting interventions to better prevent substance use amongst those experiencing homelessness in the context of the COVID-19 pandemic is a public health necessity.
Statements
Ethics statement
The studies involving human participants were reviewed and approved by the Ethical Research Committee of the University of Paris (CER-2020-41). All participants provided their written informed consent to participate in this study.
Author contributions
Conception and design of study: MM, TA, and SD. Acquisition of data: MM, CD-P, TA, CL, NF, and SD. Analysis and/or interpretation of data: HS and SD. Drafting the manuscript: HS and SD. Revising the manuscript: HS, SD, MM, CD-P, TA, CL, and NF. Approval of the version of the manuscript to be published: HS, SD, MM, CD-P, TA, CL, and NF.
Funding
This work was supported by the French collaborative Institute on Migration, the French Public Health Agency, the French National Research Agency (ANR, grant no. ANR-20-COV9-0005-01), and the European Commission Horizon 2020 H2020-SC1-PHE-CORONAVIRUS-2020-2 call (project PERISCOPE, grant no. 101016233).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2022.1604684/full#supplementary-material
References
1
McKnight-Eily LR Okoro CA Strine TW Verlenden J Hollis ND Njai R et al Racial and Ethnic Disparities in the Prevalence of Stress and Worry, Mental Health Conditions, and Increased Substance Use Among Adults during the COVID-19 Pandemic - United States, April and May 2020. MMWR Morb Mortal Wkly Rep (2021) 70(5):162–6. 10.15585/mmwr.mm7005a3
2
Adinolfi AC Bezerra AG Curado DF de Souza AAL Galduróz JCF . Drug Use Frequency Variation and Mental Health during the COVID-19 Pandemic: an Online Survey. Int J Ment Health Addict (2021) 2021:1–15. 10.1007/s11469-021-00546-7
3
Bommele J Hopman P Walters BH Geboers C Croes E Fong GT et al The Double-Edged Relationship between COVID-19 Stress and Smoking: Implications for Smoking Cessation. Tob Induc Dis (2020) 18:63. 10.18332/tid/125580
4
Guignard R Andler R Quatremère G Pasquereau A du Roscoät E Arwidson P et al Changes in Smoking and Alcohol Consumption during COVID-19-Related Lockdown: a Cross-Sectional Study in France. Eur J Public Health (2021) 31:1076–83. 10.1093/eurpub/ckab054
5
Cerda M Tracy M Galea S . A Prospective Population Based Study of Changes in Alcohol Use and Binge Drinking after a Mass Traumatic Event. Drug Alcohol Depend (2011) 115:1–8. 10.1016/j.drugalcdep.2010.09.011
6
Flory K Hankin BL Kloos B Cheely C Turecki G . Alcohol and Cigarette Use and Misuse Among Hurricane Katrina Survivors: Psychosocial Risk and Protective Factors. Subst Use Misuse (2009) 44(12):1711–24. 10.3109/10826080902962128
7
Beaudoin CE . Hurricane Katrina: Addictive Behavior Trends and Predictors. Public Health Rep (2011) 126(3):400–9. 10.1177/003335491112600314
8
Dewart T Frank B Schmeidler J . The Impact of 9/11 on Patients in New York City’s Substance Abuse Treatment Programs. Am J Drug Alcohol Abuse (2006) 32(4):665–72. 10.1080/00952990600919435
9
Vlahov D Galea S Resnick H Ahern J Boscarino JA Bucuvalas M et al Increased Use of Cigarettes, Alcohol, and Marijuana Among Manhattan, New York, Residents after the September 11th Terrorist Attacks. Am J Epidemiol (2002) 155(11):988–96. 10.1093/aje/155.11.988
10
Greene MC Haddad S Busse A Ezard N Ventevogel P Demis L et al Priorities for Addressing Substance Use Disorder in Humanitarian Settings. Confl Health (2021) 15(1):71. 10.1186/s13031-021-00407-z
11
Lo J Patel P Roberts B . A Systematic Review on Tobacco Use Among Civilian Populations Affected by Armed Conflict. Tob Control (2016) 25(2):129–40. 10.1136/tobaccocontrol-2014-052054
12
Eitan S Emery MA Bates MS Horrax C . Opioid Addiction: Who Are Your Real Friends?Neurosci Biobehav Rev (2017) 83:697–712. 10.1016/j.neubiorev.2017.05.017
13
Spagnolo PA Montemitro C Leggio L . New Challenges in Addiction Medicine: COVID-19 Infection in Patients with Alcohol and Substance Use Disorders—The Perfect Storm. Am J Psychiatry (2020) 177(9):805–7. 10.1176/appi.ajp.2020.20040417
14
Green TC Bratberg J Finnell DS . Opioid Use Disorder and the COVID 19 Pandemic: A Call to Sustain Regulatory Easements and Further Expand Access to Treatment. Subst Abus (2020) 41(2):147–9. 10.1080/08897077.2020.1752351
15
Volkow ND . Collision of the COVID-19 and Addiction Epidemics. Ann Intern Med (2020) 173(1):61–2. 10.7326/M20-1212
16
The implications of COVID-19 for people who use drugs (PWUD) and drug service providers. European Monitoring Centre for Drugs and Drug Addiction [Internet]. [cited 2021 Oct 20] (2021). Available from: https://www.emcdda.europa.eu/publications/topic-overviews/covid-19-and-people-who-use-drugs_en.
17
Chiappini S Guirguis A John A Corkery JM Schifano F . COVID-19: the Hidden Impact on Mental Health and Drug Addiction. Front Psychiatry (2020) 11:767. 10.3389/fpsyt.2020.00767
18
Yaouancq F Duée M . Les sans-domicile en 2012: une grande diversité de situations. France: Institut National de la statistique et des études économiques, France, Portrait social (2014).
19
Laporte A Vandentorren S Détrez M-A Douay C Le Strat Y Le Méner E et al Prevalence of Mental Disorders and Addictions Among Homeless People in the Greater Paris Area, France. Int J Environ Res Public Health (2018) 15(2):241. 10.3390/ijerph15020241
20
Francès P Daguzan P Bismuth S . Medical and Social Management of Homeless Individuals. A One Year Prospective Observational Study in the South Part of France, Pyrénées-Orientales. Rev Prat (2013) 63(1):29–34.
21
Andler R . Baisse de la prévalence du tabagisme quotidien parmi les adultes : Résultats du baromètre de santé publique france 2018 /reduction of daily smoking rate among adults: Results from the 2018 santé publique France Health Barometer. France: Santé publique France (2019).
22
Baggett TP Rigotti NA Campbell EG . Cost of Smoking Among Homeless Adults. N Engl J Med (2016) 374(7):697–8. 10.1056/NEJMc1508556
23
Chazalon S . Le programme national de réduction du tabagisme : retour sur trois années d’une stratégie d’ensemble pour réduire l’impact du tabac en France /the National tobacco reduction programme: Assessment of a three year comprehensive strategy to reduce the impact of tobacco in France. Santé publique France. (2018) 3:14–5.
24
Janssen F . L’influence du tabac sur la mortalité en Europe. Popul Societes (2019) 2019(571):1–4. 10.3917/popsoc.571.0001
25
Muñoz M Crespo M Pérez-Santos E . Homelessness Effects on Men’s and Women’s Health. Int J Ment Health (2005) 34(2):47–61. 10.1080/00207411.2005.11043400
26
Baggett TP Tobey ML Rigotti NA . Tobacco Use Among Homeless People — Addressing the Neglected Addiction. N Engl J Med (2013) 369(3):201–4. 10.1056/NEJMp1301935
27
Baggett TP Liauw SS Hwang SW . Cardiovascular Disease and Homelessness. J Am Coll Cardiol (2018) 71(22):2585–97. 10.1016/j.jacc.2018.02.077
28
Levy I Cohen-Louck K Bonny-Noach H . Gender, Employment, and Continuous Pandemic as Predictors of Alcohol and Drug Consumption during the COVID-19. Drug Alcohol Depend (2021) 228:109029. 10.1016/j.drugalcdep.2021.109029
29
Scallan E Bodkin C Wiwcharuk J O’Shea T Lennox R . Finding Stability amidst the COVID-19 Pandemic: The Impact of Emergency Temporary Housing for People Who Use Drugs. Drug Alcohol Rev (2021) 41:7–8. 10.1111/dar.13335
30
Hughes ME Waite LJ Hawkley LC Cacioppo JT . A Short Scale for Measuring Loneliness in Large Surveys: Results from Two Population-Based Studies. Res Aging (2004) 26(6):655–72. 10.1177/0164027504268574
31
Debussche X Lenclume V Balcou-Debussche M Alakian D Sokolowsky C Ballet D et al Characterisation of Health Literacy Strengths and Weaknesses Among People at Metabolic and Cardiovascular Risk: Validity Testing of the Health Literacy Questionnaire. SAGE Open Med (2018) 6:2050312118801250. 10.1177/2050312118801250
32
Manea L Gilbody S McMillan D . Optimal Cut-Off Score for Diagnosing Depression with the Patient Health Questionnaire (PHQ-9): a Meta-Analysis. CMAJ (2012) 184(3):e191–6. 10.1503/cmaj.110829
33
Huang FY Chung H Kroenke K Delucchi KL Spitzer RL . Using the Patient Health Questionnaire-9 to Measure Depression Among Racially and Ethnically Diverse Primary Care Patients. J Gen Intern Med (2006) 21(6):547–52. 10.1111/j.1525-1497.2006.00409.x
34
Löwe B Montan I Rose M Spitzer C Glaesmer H Wingenfeld K et al A 4-item Measure of Depression and Anxiety: Validation and Standardization of the Patient Health Questionnaire-4 (PHQ-4) in the General Population. J Affect Disord (2009) 122:86–95. 10.1016/j.jad.2009.06.019
35
Buuren S Groothuis-Oudshoorn C . MICE: Multivariate Imputation by Chained Equations in R. J Stat Softw (2011) 45. 10.18637/jss.v045.i03
36
Hosmer DW Lemeshow S . Applied Survival Analysis: Regression Modelling of Time to Event Data. Hoboken, New Jersey: Wiley (2002).
37
Hosmer DW Lemeshow S Sturdivant RX . Applied Logistic Regression. Hoboken, New Jersey: John Wiley & Sons (2013).
38
Bursac Z Gauss CH Williams DK Hosmer DW . Purposeful Selection of Variables in Logistic Regression. Source Code Biol Med (2008) 3(1):17. 10.1186/1751-0473-3-17
39
Bendel RB Afifi AA . Comparison of Stopping Rules in Forward “Stepwise” Regression. J Am Stat Assoc (1977) 72(357):46–53. 10.2307/2286904
40
Mickey RM Greenland S . The Impact of Confounder Selection Criteria on Effect Estimation. Am J Epidemiol (1989) 129(1):125–37. 10.1093/oxfordjournals.aje.a115101
41
R Core Team. European Environment Agency [Internet] (2020). Available from: https://www.eea.europa.eu/data-and-maps/indicators/oxygen-consuming-substances-in-rivers/r-development-core-team-2006.
42
Wickham H François R Henry L Müller K . RStudio. Dplyr: A Grammar of Data Manipulation [Internet] (2021). Available from: https://CRAN.R-project.org/package=dplyr.
43
Khalili P Nadimi AE Baradaran HR Janani L Rahimi-Movaghar A Rajabi Z et al Validity of Self-Reported Substance Use: Research Setting versus Primary Health Care Setting. Subst Abuse Treat Prev Pol (2021) 16(1):66. 10.1186/s13011-021-00398-3
44
Rodriguez LM Neighbors C Foster DW . Priming Effects of Self-Reported Drinking and Religiosity. Psychol Addict Behav (2014) 28(1):1–9. 10.1037/a0031828
45
Perri M Dosani N Hwang SW . COVID-19 and People Experiencing Homelessness: Challenges and Mitigation Strategies. Can Med Assoc J (2020) 192(26):e716–9. 10.1503/cmaj.200834
46
Tibbetts KK Ottoson RA Tsukayama DT , 26. Minneapolis, Minnesota, USA (2017–20182020). p. 420–6. 10.3201/eid2603.190643Public Health Response to Tuberculosis Outbreak Among Persons Experiencing Homelessness, Minneapolis, Minnesota, USA, 2017-2018.Emerg Infect Dis3
47
Pasquereau A Andler R Guignard R Soullier N Gautier A Richard JB et al Consommation de tabac parmi les adultes en 2020 : résultats du Baromètre de Santé publique France //Tobacco use among adults in 2020: Results from the Santé publique France Health Barometer. Bull épidémiologique hebdomadaire (2021) 8:132–9.
48
Beck F Richard J-B Guignard R Le Nézet O Spilka S . Levels of Drugs Use in France in 2014. Paris, France: Observatoire français des drogues et des toxicomanies (2015).
49
McBride O Bunting E Harkin O Butter S Shevlin M Murphy J et al Testing Both Affordability- Availability and Psychological-Coping Mechanisms Underlying Changes in Alcohol Use during the COVID-19 Pandemic. PLoS ONE (2022) 17(3):e0265145. 10.1371/journal.pone.0265145
50
Gomez R Thompson SJ Barczyk AN . Factors Associated with Substance Use Among Homeless Young Adults. Subst Abus (2010) 31(1):24–34. 10.1080/08897070903442566
51
Sudhinaraset M Wigglesworth C Takeuchi DT . Social and Cultural Contexts of Alcohol Use: Influences in a Social-Ecological Framework.Alcohol Res (2016) 38(1):35–45.
52
Pearson C Montgomery AE Locke G . Housing Stability Among Homeless Individuals with Serious Mental Illness Participating in Housing First Programs. J Community Psychol (2009) 37(3):404–17. 10.1002/jcop.20303
53
Collins SE Clifasefi SL Dana EA Andrasik MP Stahl N Kirouac M et al Where Harm Reduction Meets Housing First: Exploring Alcohol’s Role in a Project-Based Housing First Setting. Int J Drug Pol (2012) 23(2):111–9. 10.1016/j.drugpo.2011.07.010
54
Parkes T Carver H Masterton W Falzon D Dumbrell J Grant S et al ‘They Already Operated like it Was a Crisis, Because it Always Has Been a Crisis’: a Qualitative Exploration of the Response of One Homeless Service in Scotland to the COVID-19 Pandemic. Harm Reduct J (2021) 18(1):26. 10.1186/s12954-021-00472-w
55
Tyler KA Johnson KA . Pathways in and Out of Substance Use Among Homeless-Emerging Adults. J Adolesc Res (2006) 21(2):133–57. 10.1177/0743558405285494
56
Ghadban YA Zgheib N Romani M Akl IB Nasr R . Impact of the COVID-19 Pandemic on Smoking Behavior and Beliefs Among the American University of Beirut Community. Tob Prev Cessat (2022) 8:02–8. 10.18332/tpc/144499
57
Sun Y Wang MP Cheung YTD Ho SY Luk TT Zhao S et al Changes in Tobacco Use at the Early Stage of the COVID-19 Pandemic: Results of Four Cross-Sectional Surveys in Hong Kong. Tob Induc Dis (2022) 20:26–9. 10.18332/tid/145935
58
Prowse R Sherratt F Abizaid A Gabrys RL Hellemans KGC Patterson ZR et al Coping with the COVID-19 Pandemic: Examining Gender Differences in Stress and Mental Health Among university Students. Front Psychiatry (2021) 12(439):650759. 10.3389/fpsyt.2021.650759
59
The Council of Economic Advisers. The State of Homelessness in America: Current Statistics on the Prevalence and Characteristics of People Experiencing Homelessness in the United States. Washington, DC: The Council of Economic Advisers (2019).
60
Berenson AB San Miguel VV Wilkinson GS . Violence and its Relationship to Substance Use in Adolescent Pregnancy. J Adolesc Health (1992) 13(6):470–4. 10.1016/1054-139x(92)90009-z
61
Liebschutz J Savetsky JB Saitz R Horton NJ Lloyd-Travaglini C Samet JH . The Relationship between Sexual and Physical Abuse and Substance Abuse Consequences. J Subst Abuse Treat (2002) 22(3):121–8. 10.1016/s0740-5472(02)00220-9
62
Acierno R Kilpatrick DG Resnick H Saunders B De Arellano M Best C . Assault, PTSD, Family Substance Use, and Depression as Risk Factors for Cigarette Use in Youth: Findings from the National Survey of Adolescents. J Trauma Stress (2000) 13(3):381–96. 10.1023/A:1007772905696
63
Tinland A Boyer L Loubière S Greacen T Girard V Boucekine M et al Victimization and Posttraumatic Stress Disorder in Homeless Women with Mental Illness Are Associated with Depression, Suicide, and Quality of Life. Neuropsychiatr Dis Treat (2018) 14:2269–79. 10.2147/NDT.S161377
64
Feantsa . Women Experiencing Violence and Homelessness: Interlinked and Unaddressed Gender Specific Needs. Brussels, Belgium: FEANTSA (2019).
65
Bradbury‐Jones C Isham L . The Pandemic Paradox: The Consequences of COVID‐19 on Domestic Violence. J Clin Nurs (2020) 29:2047–9. 10.1111/jocn.15296
66
Devries KM Mak JY Bacchus LJ Child JC Falder G Petzold M et al Intimate Partner Violence and Incident Depressive Symptoms and Suicide Attempts: A Systematic Review of Longitudinal Studies. Plos Med (2013) 10(5):e1001439. 10.1371/journal.pmed.1001439
67
Gulati G Kelly BD . Domestic Violence against Women and the COVID-19 Pandemic: What Is the Role of Psychiatry?Int J L Psychiatry (2020) 71:101594. 10.1016/j.ijlp.2020.101594
68
Al-Ansari B Thow A-M Day CA Conigrave KM . Extent of Alcohol Prohibition in Civil Policy in Muslim Majority Countries: the Impact of Globalization. Addiction (2016) 111(10):1703–13. 10.1111/add.13159
69
Michalak L Trocki K . Alcohol and Islam: An Overview. Contemp Drug Probl (2006) 33(4):523–62. 10.1177/009145090603300401
70
Khlat M Bricard D Legleye S . Smoking Among Immigrant Groups in Metropolitan France: Prevalence Levels, Male-To-Female Ratios and Educational Gradients. BMC Public Health (2018) 18:479. 10.1186/s12889-018-5379-8
71
Schapendonk J . Turbulent Trajectories: African Migrants on Their Way to the European Union. Societies (2012) 2(2):27–41. 10.3390/soc2020027
72
Bygnes S Flipo A . Political Motivations for Intra-European Migration. Acta Sociol (2017) 60(3):199–212. 10.1177/0001699316659909
73
Roberts NP Roberts PA Jones N Bisson JI . Psychological Interventions for post-traumatic Stress Disorder and Comorbid Substance Use Disorder: A Systematic Review and Meta-Analysis. Clin Psychol Rev (2015) 38:25–38. 10.1016/j.cpr.2015.02.007
74
Bustamante LHU Cerqueira RO Leclerc E Brietzke E . Stress, Trauma, and Posttraumatic Stress Disorder in Migrants: a Comprehensive Review. Braz J Psychiatry (2017) 40(2):220–5. 10.1590/1516-4446-2017-2290
75
Roze M Melchior M Vuillermoz C Rezzoug D Baubet T Vandentorren S . Post-traumatic Stress Disorder in Homeless Migrant Mothers of the Paris Region Shelters. Int J Environ Res Public Health (2020) 17(13):4908. 10.3390/ijerph17134908
76
André J-M Azzedine F . Access to Healthcare for Undocumented Migrants in France: a Critical Examination of State Medical Assistance. Public Health Rev (2016) 37(1):5. 10.1186/s40985-016-0017-4
77
Fu L Lindenmeyer A Phillimore J Lessard-Phillips L . Vulnerable Migrants’ Access to Healthcare in the Early Stages of the COVID-19 Pandemic in the UK. Public Health (2022) 203:36–42. 10.1016/j.puhe.2021.12.008
78
Lessard-Phillips L Fu L Lindenmeyer A Phillimore J . Barriers to Wellbeing: Migration and Vulnerability during the Pandemic. London: The Nuffield Foundation (2021). p. 20.
79
Scarlett H Davisse-Paturet C Longchamps C Aarbaoui TE Allaire C Colleville A-C et al Depression during the COVID-19 Pandemic Amongst Residents of Homeless Shelters in France. J Affect Disord Rep (2021) 6:100243. 10.1016/j.jadr.2021.100243
80
Buckner JC Bassuk EL Zima BT . Mental Health Issues Affecting Homeless Women: Implications for Intervention. Am J Orthopsychiatry (1993) 63(3):385–99. 10.1037/h0079445
81
Suglia SF Duarte CS Sandel MT . Housing Quality, Housing Instability, and Maternal Mental Health. J Urban Health (2011) 88(6):1105–16. 10.1007/s11524-011-9587-0
82
Wang J Mann F Lloyd-Evans B Ma R Johnson S . Associations between Loneliness and Perceived Social Support and Outcomes of Mental Health Problems: a Systematic Review. BMC Psychiatry (2018) 18(1):156. 10.1186/s12888-018-1736-5
83
Mushtaq R Shoib S Shah T Mushtaq S . Relationship between Loneliness, Psychiatric Disorders and Physical Health ? A Review on the Psychological Aspects of Loneliness. J Clin Diagn Res (2014) 8(9):e01–4. 10.7860/jcdr/2014/10077.4828
84
Hosseinbor M Yassini Ardekani SM Bakhshani S Bakhshani S . Emotional and Social Loneliness in Individuals with and without Substance Dependence Disorder. Int J High Risk Behav Addict (2014) 3(3):e22688. 10.5812/ijhrba.22688
85
Bu F Steptoe A Fancourt D . Loneliness during Lockdown: Trajectories and Predictors during the COVID-19 Pandemic in 35,712 Adults in the UK. medRxiv (2020). 2020.05.29.20116657.
86
Bu F Steptoe A Fancourt D . Who Is Lonely in Lockdown? Cross-Cohort Analyses of Predictors of Loneliness before and during the COVID-19 Pandemic. medRxiv (2020). 2020.05.14.20101360.
87
Santomauro DF Herrera AMM Shadid J Zheng P Ashbaugh C Pigott DM et al Global Prevalence and burden of Depressive and Anxiety Disorders in 204 Countries and Territories in 2020 Due to the COVID-19 Pandemic. Lancet (2021) 398(10312):1700–12. 10.1016/S0140-6736(21)02143-7
88
Salari N Hosseinian-Far A Jalali R Vaisi-Raygani A Rasoulpoor S Mohammadi M et al Prevalence of Stress, Anxiety, Depression Among the General Population during the COVID-19 Pandemic: a Systematic Review and Meta-Analysis. Glob Health (2020) 16(1):57. 10.1186/s12992-020-00589-w
89
Tsuang MT Lyons MJ Meyer JM Doyle T Eisen SA Goldberg J et al Co-occurrence of Abuse of Different Drugs in Men: The Role of Drug-specific and Shared Vulnerabilities. Arch Gen Psychiatry (1998) 55(11):967–72. 10.1001/archpsyc.55.11.967
90
Kendler KS Karkowski LM Corey LA Prescott CA Neale MC . Genetic and Environmental Risk Factors in the Aetiology of Illicit Drug Initiation and Subsequent Misuse in Women. Br J Psychiatry (1999) 175(4):351–6. 10.1192/bjp.175.4.351
91
Ogbu UC Lotfipour S Chakravarthy B . Polysubstance Abuse: Alcohol, Opioids and Benzodiazepines Require Coordinated Engagement by Society, Patients, and Physicians. West J Emerg Med (2015) 16(1):76–9. 10.5811/westjem.2014.11.24720
Summary
Keywords
mental health, COVID–19, substance use, homelessness, migrant, France
Citation
Scarlett H, Melchior M, Davisse-Paturet C, Aarbaoui TE, Longchamps C, Figueiredo N and Ducarroz S (2022) Substance Use Among Residents of Homeless Shelters During the COVID-19 Pandemic: Findings From France. Int J Public Health 67:1604684. doi: 10.3389/ijph.2022.1604684
Received
10 December 2021
Accepted
26 July 2022
Published
25 August 2022
Volume
67 - 2022
Edited by
Franco Mascayano, New York State Psychiatric Institute (NYSPI), United States
Reviewed by
Rodrigo Goycolea, Central University of Chile, Chile
Updates
Copyright
© 2022 Scarlett, Melchior, Davisse-Paturet, Aarbaoui, Longchamps, Figueiredo and Ducarroz.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Honor Scarlett, honor.scarlett@iplesp.upmc.fr; Simon Ducarroz, simon.ducarroz@univ-lyon1.fr
This Original Article is part of the IJPH Special Issue “The Impact of the COVID-19 Pandemic on Mental Health”
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.