Abstract
Objectives: The objective of this study was to examine the association between several country-level systemic indices and the deaths from COVID-19 across African countries.
Method: Regression analyses were conducted to test the association between selected indices and deaths from COVID-19 across African countries. All tests were run at the α = 0.05 level of significance.
Result: We found a statistically significant correlation between total COVID-19 deaths per million and Stringency Index (p-value <0.001) and Human Development Index (p-value <0.001). Multiple regression analysis showed that Stringency Index was the only variable that remained significant when other factors are controlled for in the model.
Conclusion: Countries in Africa with poorer governance, inadequate pandemic preparedness and lower levels of development have unexpectedly fared better with respect to COVID-19 deaths mainly because of having a younger population than the countries with better indices.
Introduction
The first case of the novel coronavirus disease (COVID-19) was reported in Wuhan, China. The disease is caused by the Severe Acute Respiratory Syndrome coronavirus 2 (SARS-CoV-2). On the African continent, the first case of the disease was confirmed in Egypt on the 14th of February 2020 [1]. Since then, the infection has spread to several African countries. As of February 2022, there have been more than 11.1 million total cases and over 247,000 mortalities recorded across Africa [2]. While vaccines are being rapidly rolled-out, non-pharmaceutical interventions like the closure of schools, travel restrictions, bans on public gatherings, and stay-at-home (lockdown) orders etc. are still being applied to varying degrees to manage the spread of the virus [3, 4]. These strategies are aimed at reducing the spread of the disease and protecting high-risk individuals and have varied across the continent in the degree of implementation and effectiveness based on differing country dynamics [5, 6].
African countries have some of the poorest health indices in the world. This is evident in the poor performance of their health systems and the ineffectiveness of their governance systems [7]. The continent also houses the largest percentage of the poorest people in the world and has had challenges in the progress towards achieving the Sustainable Development Goals [8]. These factors have an impact on the effectiveness of response efforts [9]. While Africa has not recorded high mortalities in comparison to Europe and South America, reported mortality has varied across the continent [10]. Cumulative confirmed deaths in Africa as of February 2022 was 239,838 for Africa and 1.63 Million and 1.22 million for Europe and America, respectively [11].
COVID-19 mortality across the globe has been shown to vary between countries. Non-pharmaceutical measures have been shown to be effective in curbing the transmission of the virus, and by extension reduce the mortalities associated with the pandemic, and the effect of this has varied by the level of stringency of these measures and the time of implementation [12, 13]. The mortality from COVID-19 has also varied due to other factors which include proportion of the elderly in the population, prevalence of co-morbidities like malignancies, diabetes, and social and systemic factors which include the level of health system preparedness, pandemic response time, the stringency of the non-pharmaceutical preventive measures, the effectiveness of governance [12, 14, 15].
These systemic factors especially the ones dealing with the quality of governance, pandemic preparedness, quality of healthcare, and level of human development have been shown to be highly relevant to the management of disease outbreaks and overall healthcare outcomes across the world [16–19]. For the convenience of nomenclature for this study these factors will all be collectively referred to as systemic factors.
Several indices have been developed to measure and assess some of these selected systemic factors, these include Government Response Stringency Index (SI), Human Development Index (HDI), Global Health Security Index (GHSI) and the Ibrahim Index of African Governance (IIAG). The Government Response Stringency Index (SI) was created by the Oxford research group as a composite measure of restriction policies made towards limiting the spread of the virus [20]. Two recent studies have revealed that lower degree of government stringency and slower response times were associated with more deaths from COVID-19 while the level of preparedness for epidemics had no effect on recorded deaths [21, 22].
The Global Health Security Index (GHSI) is a comprehensive assessment of capabilities in different countries to prevent and respond to the threats of infectious diseases, it was developed by the Nuclear Threat Initiative (NTI), Johns Hopkins Center for Health Security (JHU) and the Economist Intelligence Unit (EIU) [23]. A study of the GHSI of Organization for Economic Cooperation and Development OECD countries’ performance during the pandemic showed a discrepancy in GHSI rating of some countries and their actual performance as some countries with high GHSI scores did not fare well in managing the spread of COVID-19 [24].
The Human Development Index (HDI) was developed by the United Nations Development Program (UNDP) to measure the aspects of human development and standards of living in member states [25]. Studies conducted by Liu et al and Imtyaz et al demonstrated a positive relationship between high development index and higher death outcomes for COVID-19 [26, 27]. Considering the significance of governance and government capacity to appropriately responding to threats and matters, the Ibrahim Index of African Governance (IIAG) is a useful metric to consider in understanding how effective African governments are in in this regard [28]. The Mo Ibrahim foundation that is behind the index released a report on COVID-19 in Africa highlighting challenges with managing the pandemic on the continent which include poor access to healthcare, inadequate infrastructure, poor data practices and weak health systems [29].
There is a paucity of studies addressing the impact of these systemic factors on COVID death outcomes on the continent. This study aims to examine the association between systemic factors using indices like SI, GHSI, HDI, IIAG and the deaths from COVID-19 across African countries. Understanding how these selected systemic factors correlate with deaths due to COVID-19 can help inform decisions on system strengthening policies and governance across the continent in managing the pandemic and other infectious diseases that plague the continent. Understanding such associations can also help emphasize the importance of the state capacity, state response, and the quality of governance in effective epidemic response and management.
Methods
Study Design
We conducted an ecological analysis of COVID-19 mortality and selected governance variables across 54 African countries. This included data available data from when the pandemic began up to the 31st of October 2020. The end date was chosen based on when most African countries had lifted lockdown measures.
Data Collection
Data were obtained from openly available sources. The COVID-19, population and Human Development Index data were obtained from; Our World in Data website which aggregates COVID-19 data from the European Centre for Disease Prevention and Control (ECDC) [10]. The dataset consisted of aggregated data from various sources such as World Health Organization (WHO), European Center for Disease Prevention and Control, the Centers for Disease Control and Prevention (CDC), and various other governmental and non-governmental organizations. The data covers 54 countries on the African continent. The Health Security Index data were obtained from the Global Health Security Index database, while the Ibrahim Index of African Governance (IIAG) index data were obtained from the IIAG website [23, 28].
Data Analysis
We applied linear and multiple regression to analyze the association between the dependent variable which is deaths from COVID-19 (total COVID-19 deaths per million), and the independent variables which are Government Response Stringency Index, Global Health Security Index, Human Development Index, and Ibrahim Index of African Governance, with percentage of population aged above 65 as the covariate. The total deaths per millions was used for this analysis to ensure an adjustment for population density differences for the COVID-19 deaths across the different countries. For Stringency Index 18 countries were excluded as there was no data available for them.
We log-transformed the total COVID-19 deaths per million (TCDPerMill) outcome variable, using log-linear regression to examine the relationship between the outcome and independent variables and to ensure that we passed the assumptions of simple and multiple linear regression. This was done to normalize the data and manage the skewness of the data. All tests were run at the α = 0.05 level of significance. We also conducted an analysis of variance to evaluate and validate the model. To determine the overall regression equation, we used the Unstandardized coefficients to see the effects of each of the independent variables on the outcome. All statistical analyses were conducted using SAS software 9.4 (SAS Institute Inc., Cary NC).
Results
Data on TCDpermill, percentage of population aged 65 and older, SI, GHSI, IIAG and HDI data for 54 African countries are shown in Table 1.
TABLE 1
| Country | TCDperMill | Age65older | SI | GHSI | IIAG | HDI |
|---|---|---|---|---|---|---|
| Algeria | 44.606 | 6.211 | 75 | 23.6 | 56.2 | 0.754 |
| Angola | 8.367 | 2.405 | 65.74 | 25.2 | 40 | 0.581 |
| Benin | 3.382 | 3.244 | 43.52 | 28.8 | 58.6 | 0.515 |
| Botswana | 10.206 | 3.941 | 52.78 | 31.1 | 66.9 | 0.717 |
| Burkina Faso | 3.205 | 2.409 | 22.22 | 30.1 | 54 | 0.423 |
| Burundi | 0.084 | 2.562 | 14.81 | 22.8 | 36.9 | 0.417 |
| Cameroon | 16.048 | 3.165 | 45.37 | 34.4 | 43.5 | 0.556 |
| Cape Verde | 170.867 | 4.46 | 71.3 | 29.3 | 73.1 | 0.654 |
| Central African Republic | 12.837 | 3.655 | 27.3 | 30.7 | 0.367 | |
| Chad | 5.966 | 2.486 | 66.67 | 28.8 | 33.9 | 0.404 |
| Comoros | 8.05 | 2.963 | 27.2 | 43.2 | 0.503 | |
| Congo | 16.672 | 3.402 | 47.22 | 23.6 | 36.1 | 0.606 |
| Cote d'Ivoire | 4.701 | 2.933 | 35.5 | 53.9 | 0.492 | |
| Democratic Republic of Congo | 3.417 | 3.02 | 26.5 | 31.7 | 0.457 | |
| Djibouti | 61.741 | 4.213 | 43.52 | 23.2 | 41.3 | 0.476 |
| Egypt | 61.152 | 5.159 | 75.93 | 39.9 | 47.4 | 0.696 |
| Equatorial Guinea | 59.16 | 2.846 | 16.2 | 28.7 | 0.591 | |
| Eritrea | 3.607 | 81.48 | 22.4 | 25.8 | 0.44 | |
| Ethiopia | 12.734 | 3.526 | 57.41 | 40.6 | 46.6 | 0.463 |
| Gabon | 24.711 | 4.45 | 69.44 | 20 | 47.7 | 0.702 |
| Gambia | 49.241 | 2.339 | 56.48 | 34.2 | 55.9 | 0.46 |
| Ghana | 10.298 | 3.385 | 38.89 | 35.5 | 64.3 | 0.592 |
| Guinea | 5.482 | 3.135 | 35.65 | 32.7 | 42.5 | 0.459 |
| Guinea-Bissau | 20.833 | 3.002 | 20 | 41.4 | 0.455 | |
| Kenya | 18.244 | 2.686 | 68.52 | 47.1 | 58.5 | 0.59 |
| Lesotho | 20.072 | 4.506 | 40.74 | 30.2 | 52.3 | 0.52 |
| Liberia | 16.213 | 3.057 | 57.41 | 35.1 | 47.9 | 0.435 |
| Libya | 123.267 | 4.424 | 79.63 | 25.7 | 35.2 | 0.706 |
| Madagascar | 8.812 | 2.929 | 52.78 | 40.1 | 44.4 | 0.519 |
| Malawi | 9.618 | 2.979 | 50.93 | 28 | 51.5 | 0.477 |
| Mali | 6.716 | 2.519 | 34.26 | 29 | 46.6 | 0.427 |
| Mauritania | 35.056 | 3.138 | 27.5 | 41.6 | 0.52 | |
| Mauritius | 7.863 | 10.945 | 34.9 | 77.2 | 0.79 | |
| Morocco | 98.21 | 6.769 | 65.74 | 43.7 | 61 | 0.667 |
| Mozambique | 2.911 | 3.158 | 53.7 | 28.1 | 49 | 0.437 |
| Namibia | 52.343 | 3.552 | 35.6 | 65.1 | 0.647 | |
| Niger | 2.85 | 2.553 | 11.11 | 32.2 | 47.8 | 0.354 |
| Nigeria | 5.55 | 2.751 | 50.93 | 37.8 | 45.5 | 0.532 |
| Rwanda | 2.702 | 2.974 | 34.2 | 60.5 | 0.524 | |
| Sao Tome and Principe | 73.006 | 2.886 | 17.7 | 60.4 | 0.589 | |
| Senegal | 19.291 | 3.008 | 37.96 | 37.9 | 63.2 | 0.505 |
| Seychelles | 8.606 | 31.9 | 72.3 | 0.797 | ||
| Sierra Leone | 9.277 | 2.538 | 31.48 | 38.2 | 51 | 0.419 |
| Somalia | 6.544 | 2.731 | 32.41 | 16.6 | 19.2 | |
| South Africa | 324.236 | 5.344 | 54.8 | 65.8 | 0.699 | |
| South Sudan | 5.181 | 3.441 | 35.19 | 21.7 | 20.7 | 0.388 |
| Sudan | 19.088 | 3.548 | 32.41 | 26.2 | 32.5 | 0.502 |
| eSwatini (Swaziland) | 100.848 | 3.163 | 31.1 | 43.8 | 0.588 | |
| Tanzania | 0.352 | 3.108 | 36.4 | 53 | 0.538 | |
| Togo | 6.644 | 2.839 | 32.5 | 50.1 | 0.503 | |
| Tunisia | 111.434 | 8.001 | 75 | 33.7 | 70.4 | 0.735 |
| Uganda | 2.405 | 2.168 | 57.41 | 44.3 | 51.8 | 0.516 |
| Zambia | 18.984 | 2.48 | 28.7 | 52 | 0.588 | |
| Zimbabwe | 16.282 | 2.822 | 38.2 | 46.1 | 0.535 |
TCDpermill, percentage of population aged 65 and older, SI, GHSI, IIAG and HDI data for African countries (An Assessment of Systemic Factors and COVID-19 Mortality in Africa, Africa, 2021).
The regression equation predicting TCDPerMill from all the independent variables is as follows:
The Regression analysis (Figure 1) showed a statistically significant correlation between TCDPerMill and SI (coefficient = 0.024, p-value −0.000), and HDI relationship (coefficient = 3.303, p-value 0.000). No statistically significant relationship (coefficient = 0.007, p-value 0.537) was also found between TCDPerMill and GHSI (coefficient = 0.007, p-value 0.537), and IIAG (coefficient = 0.012, p-value 0.094).
FIGURE 1
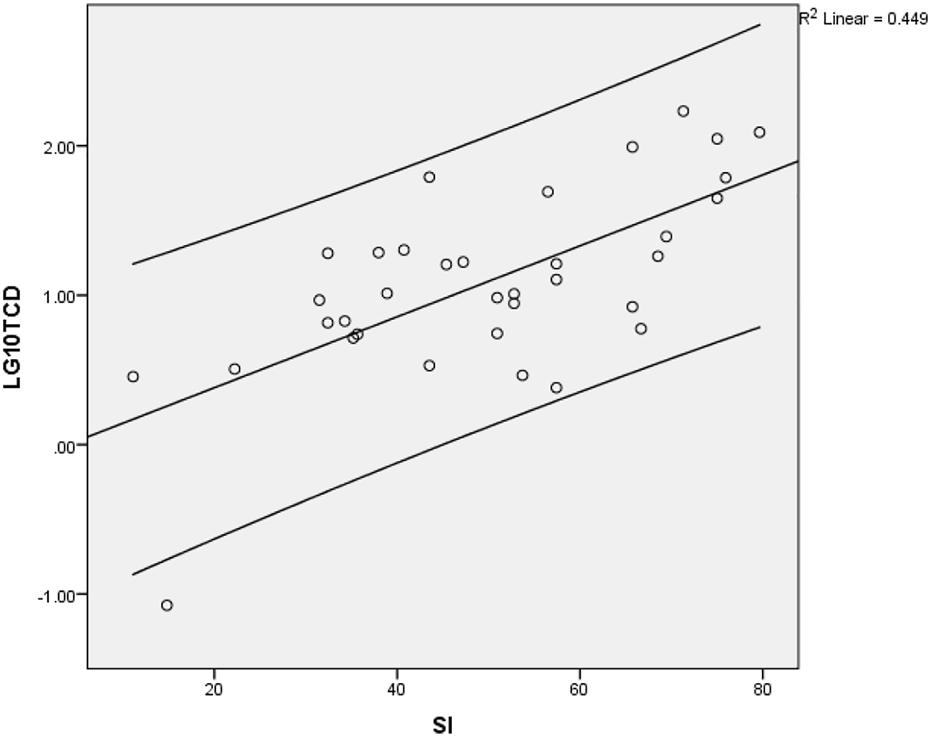
Relationship between stringency index and Total Covid Deaths per million. The dependent variable used here is the log10 of TCDPerMill (An Assessment of Systemic Factors and COVID-19 Mortality in Africa, Africa, 2021).
Multiple linear regression was carried out to investigate whether SI, GHSI, HDI, IIAG and percentage of population aged above 65 could predict COVID-19 deaths in African countries. The results (Table 2) of the regression showed that the model was a significant predictor of COVID-19 deaths (F [5, 28] = 7.586, p = 0.00001). SI was the only variables that was significant in the model. Based on the model SI yields a 0.46 increase in TCDperMillion for every unit increase while controlling for the other variables and the covariate (Age65Older).
TABLE 2
| (Constant) | −0.637 (0.536) |
| Age65older | 0.188 (0.086) |
| SI | 0.016a (0.007) |
| GHSI | 0.002 (0.013) |
| IIAG | 0.005 (0.009) |
| HDI | −0.126 (1.321) |
| R- Squared | 0.575 |
| No of Observations | 54 |
Results of multiple linear regression of the independent variables against Total Covid Deaths per million (An Assessment of Systemic Factors and COVID-19 Mortality in Africa, Africa, 2021).
Standard errors are in parentheses.
The dependent variable used here is the log10 of TCDPerMill, and Age65older is the covariate.
aIndicates statistical significance.
Discussion
This study provides insight into factors affecting recorded deaths attributed COVID-19 across Africa and helps to further our understanding of how governance and health indices are associated with the recorded mortalities from the COVID-19 pandemic. Statistically significant associations were not found between the GHSI, IIAG, and deaths from COVID-19 which is similar to results obtained from a study conducted by Hooper that showed that the GHSI had no effects on COVID-19 deaths [21]. However, there was a positive association between deaths from COVID-19, SI and HDI. The GHSI is known as a tool that shows promise in giving insights into levels of biosafety and levels of systems preparedness for countries, but they are encouraged to look beyond it for mitigating factors for impact of pandemics, as this study and another conducted by Hooper have shown how it has no effect on the death outcomes for COVID-19 [21, 30]. The GHSI has been criticized for not incorporating the social and political features that have significant effect on public health outcomes across different countries, hence this is why it has not performed well in aligning with performance of different countries in managing COVID-19 [31].
Some of these results can be explained by the fact that we used total deaths as opposed to weekly averages for this study and the possibility that countries that had higher mortalities implemented stricter or more stringent measures to control the pandemic. The positive association seen between HDI and COVID-19 deaths is underlined by the percentage of the population aged above 65 being higher in countries with higher levels of HDI, because these countries have higher life expectancy because of better healthcare and living conditions [32]. Also, since these countries have higher indices of SI and IIAG too, and COVID-19 is more fatal in individuals above the age of 65, the positive association can be explained by the fact that there will be more deaths in these countries because of their higher population of persons above 65, and older people also constitute a significant percentage of those with co-morbidities [33, 34]. This is consistent with results from a study conducted by Liu et al which revealed a positive association between COVID-19 deaths and HDI in Italy, and in another study by Imtyaz et al. that revealed that European countries were recording higher COVID-19 deaths due to higher percentage of elderly people compared to other countries [26, 27].
However, the impact of HDI disappeared when we controlled for variables in a multiple regression with just Stringency Index and percentage of population aged 65 and above showing significance. This disappearance of effect could be explained by the fact that countries with higher HDIs have larger percentages of the population above 65 and controlling for this variable removes that effect. As shown earlier that there is a linear relationship between HDI and COVID-19 deaths, this effect can then be explained by the percentage of population aged above 65 in each country. This also shows that the strongest factors related to outcomes of death in Africa are SI and percentage of the population aged above 65.
Limitations
Our findings should be considered in the context of several limitations. Our study is subject to inherent ecological fallacies that stem from the data used which are country-level data such as total deaths which is highly affected by the variability in COVID-19 reporting, between countries in Africa. Also, a more appropriate way to ascertain the effect of SI will be to assess its relationships with weekly moving averages over time as this will show how recorded deaths have changed and if stringency measures have been effective. We were furthermore unable to account for the time to implementation of the social distancing measures, and death outcomes which will differ based on how soon each country implemented their measures. It is also important to note that our results are only showing associations and not inferring causality. This is important context for interpreting and applying the lessons from this study.
Conclusion
COVID-19 deaths on the African continent have largely been less compared to other countries and places in the world. Countries in Africa with poorer governance, inadequate pandemic preparedness and lower levels of development have unexpectedly fared better with respect to COVID-19 deaths mainly because of having a younger population than the countries with better indices. This study helps with insight on one of the most significant reasons that is associated with higher COVID-19 deaths per population across African countries which is population demographics.
Statements
Author Contributions
AO conceptualized the study and wrote the initial draft with the initial statistical analyses. TB worked on improving the statistical analysis and the multiple regression aspect. JO, TN, OF, AA, and IA contributed to all other aspects of the article, edited and reviewed the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1
Makoni M . COVID-19 in Africa: Half a Year Later. Lancet Infect Dis (2020) 20(10):1127. 10.1016/S1473-3099(20)30708-8
2
Africa CDC. Africa CDC - COVID-19 Daily Updates [Internet] (2020). Available from: https://africacdc.org/covid-19/.
3
Nicola M O’Neill N Sohrabi C Khan M Agha M Agha R . Evidence Based Management Guideline for the COVID-19 Pandemic - Review Article. Int J Surg (2020) 77:206–16. 10.1016/j.ijsu.2020.04.001
4
Ferguson N Laydon D Nedjati Gilani G Imai N Ainslie K Baguelin M et al Report 9: Impact of Non-pharmaceutical Interventions (NPIs) to Reduce COVID19 Mortality and Healthcare Demand. London, England: Imperial College London (2020).
5
Banholzer N van Weenen E Kratzwald B Seeliger A Bottrighi P Cenedese A et al The Estimated Impact of Non-pharmaceutical Interventions on Documented Cases of COVID-19: A Cross-Country Analysis. medRxiv (2020).
6
Deb P Furceri D Ostry J Tawk N . The Effect of Containment Measures on the COVID-19 Pandemic. IMF Working Pap (2020) 20:42. 10.5089/9781513550268.001
7
World Health Organization. World Health Statistics 2020: Monitoring Health for the SDGs, Sustainable Development Goals. Geneva, Switzerland: World Health Organization (2020).
8
Sachs J Schmidt-Traub G Kroll C Lafortune G Fuller G . Sustainable Development Report 2019. New York: Bertelsmann Stiftung and Sustainable Development Solutions Network (2019).
9
Amaechi UA Sodipo BO Nnaji CA Owoyemi A Omitiran K Okedo-Alex IN et al Social Approaches to COVID-19 Pandemic Response: Effectiveness and Practicality in Sub-saharan Africa. Pan Afr Med J (2020) 37:2. 10.11604/pamj.supp.2020.37.2.25183
10
Our World in Data. Coronavirus Pandemic (COVID-19) – the data [Internet] (2020). Available from: https://ourworldindata.org/coronavirus-data.
11
Our World in Data. Cumulative confirmed COVID-19 deaths by world region [Internet] (2022). Available from: https://ourworldindata.org/grapher/cumulative-covid-deaths-region.
12
Flaxman S Mishra S Gandy A Unwin HJT Mellan TA Coupland H et al Estimating the Effects of Non-pharmaceutical Interventions on COVID-19 in Europe. Nature (2020) 584(7820):257–61. 10.1038/s41586-020-2405-7
13
Fuller JA Hakim A Victory KR Date K Lynch M Dahl B et al Mitigation Policies and COVID-19–Associated Mortality — 37 European Countries, January 23–June 30, 2020. MMWR Morb Mortal Wkly Rep (2021) 70(2):58–62. 10.15585/mmwr.mm7002e4
14
Hadjidemetriou GM Sasidharan M Kouyialis G Parlikad AK . The Impact of Government Measures and Human Mobility Trend on COVID-19 Related Deaths in the UK. Transp Res Interdiscip Perspect (2020) 6:100167. 10.1016/j.trip.2020.100167
15
Abrams EM Szefler SJ . COVID-19 and the Impact of Social Determinants of Health. Lancet Respir Med (2020) 8(7):659–61. 10.1016/S2213-2600(20)30234-4
16
Nawaz A Su X Barkat MQ Asghar S Asad A Basit F et al Epidemic Spread and its Management through Governance and Leadership Response Influencing the Arising Challenges Around COVID-19 in Pakistan—A Lesson Learnt for Low Income Countries with Limited Resource. Front Public Health (2020) 8:573431. 10.3389/fpubh.2020.573431
17
Martínez-Córdoba PJ Benito B García-Sánchez IM . Efficiency in the Governance of the Covid-19 Pandemic: Political and Territorial Factors. Glob Health (2021) 17(1):113. 10.1186/s12992-021-00759-4
18
Soheylizad M Khazaei S Jenabi E Delpisheh A Veisani Y . The Relationship between Human Development Index and its Components with Thyroid Cancer Incidence and Mortality: Using the Decomposition Approach. Int J Endocrinol Metab (2018) 16(4):e65078. 10.5812/ijem.65078
19
Hu QD Zhang Q Chen W Bai XL Liang TB . Human Development index Is Associated with Mortality-To-Incidence Ratios of Gastrointestinal Cancers. World J Gastroenterol (2013) 19(32):5261–70. 10.3748/wjg.v19.i32.5261
20
Hale T Angrist N Goldszmidt R Kira B Petherick A Phillips T et al A Global Panel Database of Pandemic Policies (Oxford COVID-19 Government Response Tracker). Nat Hum Behav (2021) 5(4):529–38. 10.1038/s41562-021-01079-8
21
Hooper VJ . Global Determinants of Covid-19 Deaths: Lockdown Dates and Social Distancing Measures Mattered. medRxiv (2020).
22
Hale T Noam A Cameron-Blake E Hallas L Kira B Majumdar S et al Variation in Government Responses to COVID-19 [Internet]. Report No.: Version 8.0 (2020). Available from: https://www.bsg.ox.ac.uk/sites/default/files/2020-10/BSG-WP-2020-032-v8.pdf.
23
GHS Index. About the GHS Index [Internet] (2019). Available from: https://www.ghsindex.org/about/.
24
Abbey EJ Khalifa BAA Oduwole MO Ayeh SK Nudotor RD Salia EL et al The Global Health Security Index Is Not Predictive of Coronavirus Pandemic Responses Among Organization for Economic Cooperation and Development Countries. PLOS ONE (2020) 15(10):e0239398. 10.1371/journal.pone.0239398
25
Human Development Reports. Human Development Index (HDI) [Internet] (2022). Available from: http://hdr.undp.org/en/content/human-development-index-hdi.
26
Liu K He M Zhuang Z He D Li H . Unexpected Positive Correlation between Human Development index and Risk of Infections and Deaths of COVID-19 in Italy. One Health (2020) 10:100174. 10.1016/j.onehlt.2020.100174
27
Imtyaz A Haleem A Javaid M . Analysing Governmental Response to the COVID-19 Pandemic. J Oral Biol Craniofac Res (2020) 10(4):504–13. 10.1016/j.jobcr.2020.08.005
28
Mo Ibrahim Foundation. Ibrahim Index of African Governance (IIAG) Report [Internet] (2020). Available from: https://mo.ibrahim.foundation/sites/default/files/2020-11/2020-index-report.pdf.
29
Mo Ibrahim Foundation. COVID-19 in Africa: A Call for Coordinated Governance, Improved Health Structures and Better Data [Internet] (2020). Available from: https://reliefweb.int/sites/reliefweb.int/files/resources/2020%20COVID-19%20in%20Africa.pdf.
30
Boyd MJ Wilson N Nelson C . Validation Analysis of Global Health Security Index (GHSI) Scores 2019. BMJ Glob Health (2020) 5(10):e003276. 10.1136/bmjgh-2020-003276
31
Mahajan M . Casualties of Preparedness: the Global Health Security Index and COVID-19. Int J L Context (2021) 17(2):204–14. 10.1017/s1744552321000288
32
Human Development Reports. Wide Inequalities in People’s Well-Being Cast a Shadow on Sustained Human Development Progress (2018). Available from: http://hdr.undp.org/en/content/wide-inequalities-peoples-well-being-cast-shadow-sustained-human-development-progress.
33
Mueller AL McNamara MS Sinclair DA . Why Does COVID-19 Disproportionately Affect Older People?Aging (Albany NY) (2020) 12(10):9959–81. 10.18632/aging.103344
34
Vos T Lim SS Abbafati C Abbas KM Abbasi M Abbasifard M et al Global burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990–2019: a Systematic Analysis for the Global Burden of Disease Study 2019. Lancet (2020) 396(10258):1204–22. 10.1016/S0140-6736(20)30925-9
Summary
Keywords
mortality, COVID, lockdown, governance, Africa, stringency index
Citation
Owoyemi A, Balogun T, Okoro J, Ndoro T, Fasominu O, Atanda A and Abioye I (2022) An Assessment of Systemic Factors and COVID-19 Mortality in Africa. Int J Public Health 67:1604915. doi: 10.3389/ijph.2022.1604915
Received
13 March 2022
Accepted
31 August 2022
Published
13 September 2022
Volume
67 - 2022
Edited by
Nino Kuenzli, Swiss Tropical and Public Health Institute (Swiss TPH), Switzerland
Reviewed by
Katarzyna Czech, Warsaw University of Life Sciences, Poland
Updates
Copyright
© 2022 Owoyemi, Balogun, Okoro, Ndoro, Fasominu, Atanda and Abioye.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ayomide Owoyemi, blacbard@gmail.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.