- 1School of Public Health The Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, Zhejiang, China
- 2School of Public Health, Capital Medicine University, Beijing, China
Objectives: This study aimed to examine the association of solid fuel use for cooking and heating with the progression of multimorbidity.
Methods: A total of 5,437 participants from the China Health and Retirement Longitudinal Study were included. Multivariate logistic regression models were used to estimate the odds ratios (ORs) and 95% confidence intervals (CIs) for the associations of the independent and joint effects of solid fuel use for cooking and heating with the progression of multimorbidity.
Results: The proportion of participants reporting solid fuel use for both cooking and heating was 59.0% at baseline. Solid fuel use for both cooking and heating was associated with the progression of multimorbidity (adjusted OR: 1.42, 95% CI: 1.19–1.70), compared with clean fuel use for both.
Conclusion: Solid fuel use for cooking and heating play an important role in the progression of multimorbidity. Therefore, solid fuel reduction should be considered in developing multimorbidity control and prevention programmes.
Introduction
Using solid fuels (e.g., coal, wood, charcoal, dung, and crop residues [1]) for cooking or heating could lead to household air pollution, which is one of the most important risk factors for the rising number of chronic diseases. This is because solid fuels can produce an array of pollutants (like PM2.5, black carbon, and carbon monoxide), particularly in inadequately ventilated homes [2]. According to China’s National Energy Administration, China has provided full electricity access to all residents in December 2015 [3]. However, approximately 361 million people in China continued to use solid fuel for cooking and heating, leading to 8.74 million disability-adjusted life-years (DALYs) and .36 million deaths in 2019 [2]. Solid fuel for cooking has been a major public health problem in China and other developing countries [4, 5], and burning solid fuel for heating in winter or rainy seasons is also common in China. For example, burning solid fuels in heating stoves or “kangs” in the winter is still the most common home-heating practice [6, 7]. Previous studies have explored the health impacts of solid fuel use, but most of them did not distinguish between the effect of using solid fuel for cooking and for heating [8–11]. The independent and joint effects of solid fuel use for cooking and heating on health remain largely unknown.
Evidence has emerged that solid fuel use was associated with single chronic conditions, such as hypertension, diabetes, lung disease, liver disease, heart disease, arthritis, and asthma [12–15]. With the aging of the population, the co-existence of two or more chronic conditions in the elderly, defined as multimorbidity, has become more common worldwide, with the prevalence of multimorbidity in China ranging from 57% to 81% [16, 17]. Several studies showed that multimorbidity led to reduced quality of life such as poor functional status, increasing cost of health services such as longer hospital stays, and higher levels of primary care than single conditions [16, 18–20]. This challenged the current public health system, which paid more attention to single conditions than multimorbidity.
This study aimed to examine the independent and joint effects of solid fuel use for cooking and heating on the progression of multimorbidity using the China Health and Retirement Longitudinal Study (CHARLS), a nationally representative prospective study in China.
Methods
Study Population
This longitudinal cohort study was conducted based on the harmonized data (2011–2018) from CHARLS developed by the Gateway to Global Aging Data. Detailed information on CHARLS has been described elsewhere [21]. Briefly, the CHARLS enrolled participants from 450 urban communities and rural areas in 28 provinces of China. Information on health status, socio-demographic characteristics, and lifestyle factors were collected. The baseline survey with 17,708 individuals was conducted between June 2011 to March 2012 and the follow-up surveys were carried out every 2 years (2013, 2015, and 2018).
A total of 11,442 participants aged 45 years and above who responded to the four surveys were included in our study. The exclusion criteria were: 1) individuals with missing values on solid fuel use; 2) individuals with missing values on covariates; 3) individuals with missing values on information about chronic conditions. Finally, a total of 5,437 participants were included in the analysis (Figure 1).
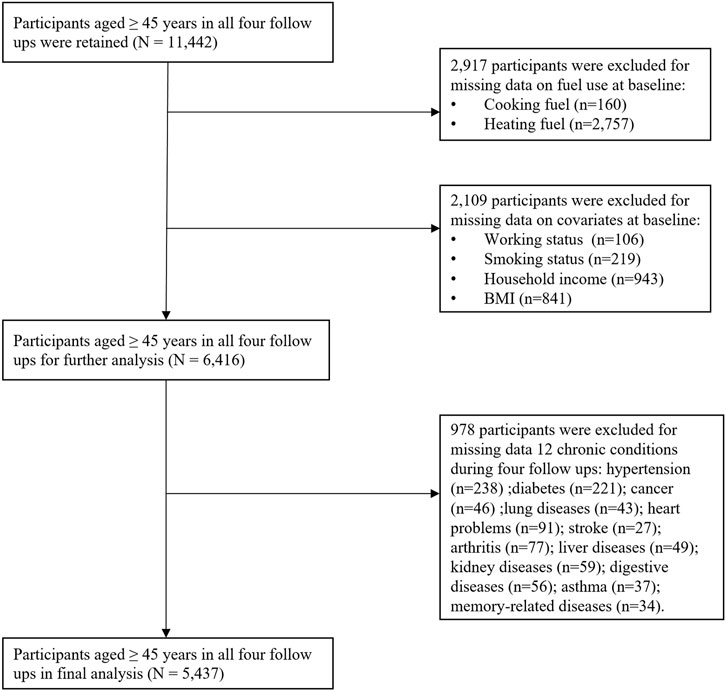
FIGURE 1. Flowchart of the participants included in the present study (China Health and Retirement Longitudinal Study, China, 2011–2018).
Assessment of Solid Fuel Use
Information on solid fuel use was collected through a questionnaire assessment of CHARLS, in which the fuel for cooking was collected across four waves (2011, 2013, 2015, and 2018), and fuel for heating was collected in 2011 and 2015. Using the following questions: “what is the main source of cooking fuel?” and “what is the main heating energy source?”. Based on previous studies [11, 22], we categorized cooking fuel as either solid fuel (crop residue/wood; or coal) or clean fuel (natural gas; marsh gas [CH4]; liquefied petroleum gas; or electric); heating fuel was also categorized as either solid fuel (crop residue/wood; or coal) or clean fuel (solar; natural gas; liquefied petroleum gas; or electric) [23]. The joint effect of solid fuel use for cooking and heating was categorized as both clean fuel use, either solid fuel use and both solid fuel use. In the current study, the baseline survey of fuel use was used for the main analysis.
Assessment of Multimorbidity Progression
Based on previous studies about the association of household air pollution with chronic conditions and the disease burden of household air pollution [12, 24, 25], 12 chronic conditions were selected to define multimorbidity in this study, including hypertension, diabetes or high blood sugar, cancer or malignancies, chronic lung diseases (e.g., chronic bronchitis and emphysema), heart problems (e.g., heart attack, coronary heart disease, angina, congestive heart failure, or other heart problems), stroke, arthritis or rheumatism, liver diseases, kidney diseases, digestive diseases (e.g., stomach or other digestive diseases), asthma, and memory-related disease (e.g., Alzheimer’s disease, Brain atrophy, and Parkinson’s disease). In each wave (2011, 2013, 2015, and 2018) participants were asked whether they were diagnosed with a list of the above 12 chronic conditions. Stable condition progression was defined as not developing any new conditions during follow-up. Single condition progression was defined as developing one condition for participants with no condition at baseline. Multimorbidity progression was defined as developing two or more chronic conditions for participants with no conditions or developing the new condition(s) for participants with one or more conditions at baseline.
Covariates
Covariates were collected at baseline. According to previous studies [22, 26], covariates include socio-demographic variables (age, sex, education level, marital status, working status, household income, and residence) and lifestyle factors (smoking status, drinking status, and body mass index [BMI]). Sex was reported as male and female. Education level was categorized as less than lower secondary, upper secondary & vocational, and tertiary. Working status was categorized as unemployed/retired/never worked and employed. Household income was categorized by the quartile. Marital status was categorized as married/partnered and others (separated, divorced, widowed, and never married). The residence was categorized as living in urban or rural. Smoking status was categorized as ever/never smoking and current smoking. Drinking status was categorized as never drinking and ever drinking. BMI was classified according to the criteria for Chinese adults [27]: underweight: <18.5 kg/m2; normal weight: 18.5–23.9 kg/m2; overweight: 24–27.9 kg/m2; obese: ≥28 kg/m2.
Statistical Analysis
Baseline characteristics were described as mean with standard deviation (SD) or numbers (percentages) according to solid fuel use for cooking and heating at baseline (2011), multimorbidity progression during follow-up (2011–2018), and four waves (2011, 2013, 2015, and 2018), respectively. Furthermore, the baseline characteristics were also presented according to the sample excluding or not excluding missing data. Differences among the groups were compared using the Student’s t-test or Analysis of Variance for continuous variables and the Chi-squared test for categorical variables.
Multivariate logistic regression models were used to calculate odds ratios (ORs) with 95% confidence intervals (CIs) for the association of the independent and joint solid fuel use for cooking and heating with the progression of multimorbidity, compared with clean fuel use. Model 1 was unadjusted. Model 2 was adjusted for age, sex, education levels, marital status, working status, household income, and residence. Model 3 was further adjusted for smoking status, drinking status, and BMI. Solid fuels for cooking and heating were mutually adjusted in all models.
To test the robustness of our results, this study further conducted several additional analyses with the fully adjusted model: 1) analyzing the joint effect of solid fuel use for cooking and heating on the incidence of 12 single chronic conditions; 2) analyzing the independent effect of each specific type of fuel for cooking and heating on multimorbidity progression; 3) subgroup analyses by age, sex, education levels, marital status, working status, household income, and residence, smoking status, drinking status, and BMI among the joint effect of solid fuel use for cooking and heating on multimorbidity progression; 4) two sensitivity analyses of the joint effect of solid fuel for cooking and heating on multimorbidity progression, one repeated the analysis in participants without the selected conditions at baseline and the other one conducted by defining electric or solar as clean fuel. Additionally, we also explored the association between the duration of solid fuel use for cooking from 2011 to 2018 and multimorbidity progression. The duration of solid fuel use for cooking was categorized as 0, 1-6, and 7 years or more. It was calculated based on the fuel types used for cooking in four waves [28]. For example, if individuals used clean fuel for cooking in all four waves, then the duration of solid fuel use for cooking was 0 years. Likewise, the duration of solid fuel use for cooking was >7 years if individuals used solid fuel for cooking in all four waves.
Statistical analyses were performed using SAS (version 9.4, SAS Institute Inc.). A two-sided result with p < .05 in all statistical tests were considered statistically significant.
Results
Baseline Characteristics of Study Populations
The baseline characteristics of participants were compared according to the solid fuel use for cooking and heating at baseline (Table 1) and the progression of multimorbidity during follow-up (Table 2), respectively. At baseline, 64.1% of participants reported using solid fuel for cooking, 78.5% reported using solid fuel for heating, and 59.0% reported using solid fuel for both cooking and heating. A total of 3,011 (55.4%) participants experienced multimorbidity progression during follow-up. In general, participants who used solid fuel were more likely to have lower levels of education, live in rural areas, be employed, and have lower household income (Table 1). Participants who experienced multimorbidity progression were more likely to be employed and non-drinkers (Table 2). Additionally, the baseline characteristics of participants were also presented according to the sample, excluding or not excluding missing data (Supplementary Table S1) and four waves (2011, 2013, 2015, and 2018) (Supplementary Table S2).
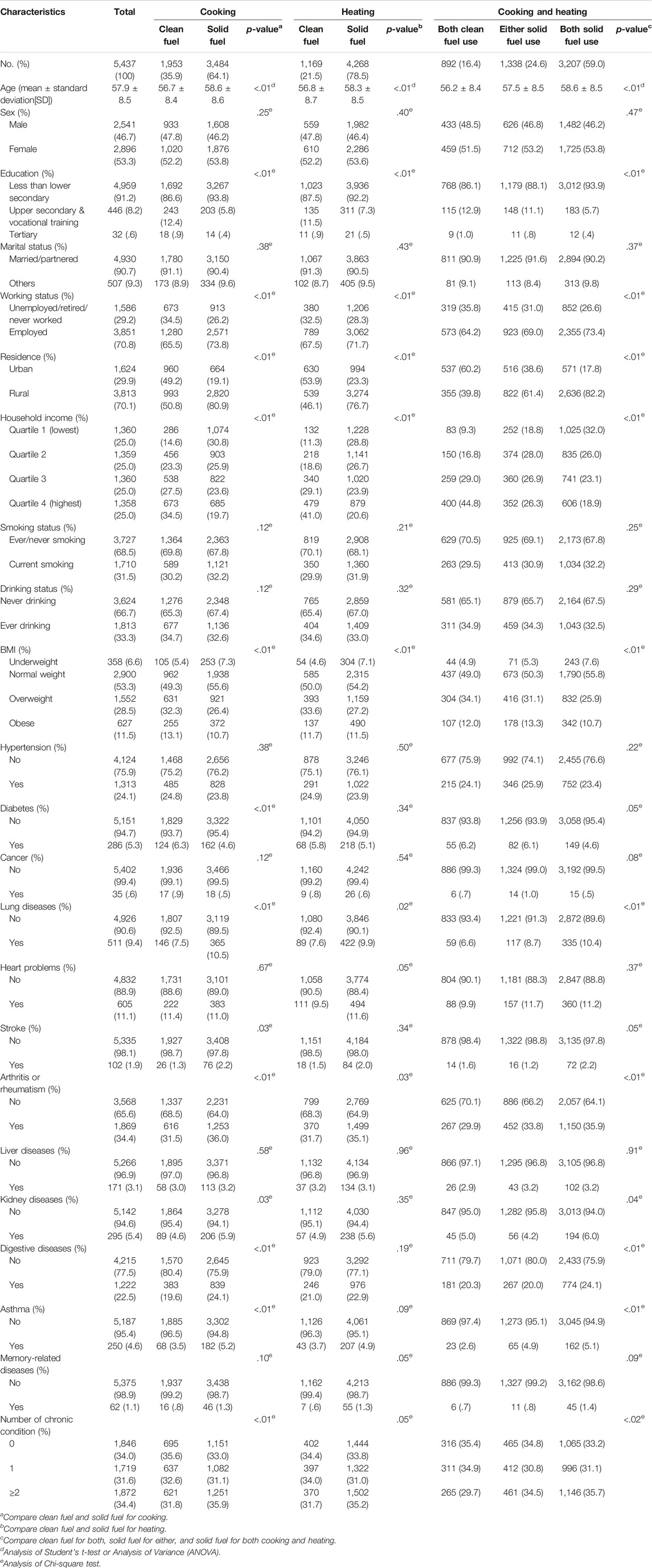
TABLE 1. Baseline characteristics of participants according to solid fuel use for cooking and heating at baseline (China Health and Retirement Longitudinal Study, China, 2011).
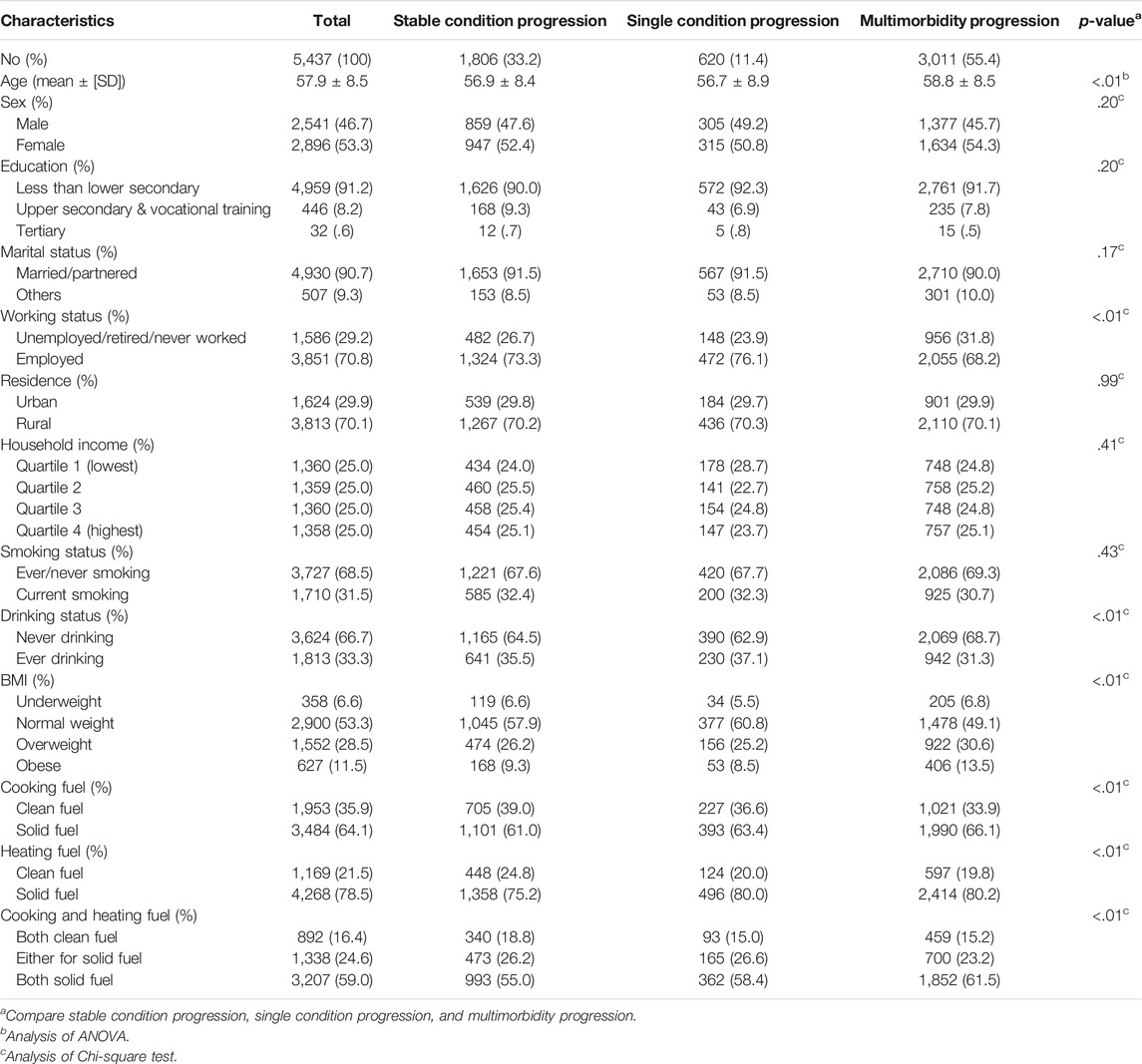
TABLE 2. Baseline characteristics of participants according to the progression of multimorbidity during follow-up (China Health and Retirement Longitudinal Study, China, 2011–2018).
Solid Fuel Use and Multimorbidity
Solid fuel use was associated with the progression of multimorbidity (Table 3). Solid fuel use for cooking or heating was associated with multimorbidity progression with adjusted odds of 1.16 (95% CI: 1.01–1.34) or 1.28 (95% CI: 1.09–1.50), respectively, compared with clean fuel use. Both solid fuel use for cooking and heating was also associated with multimorbidity progression with adjusted odds of 1.42 (95% CI: 1.19–1.70), compared with both clean fuel use for cooking and heating.
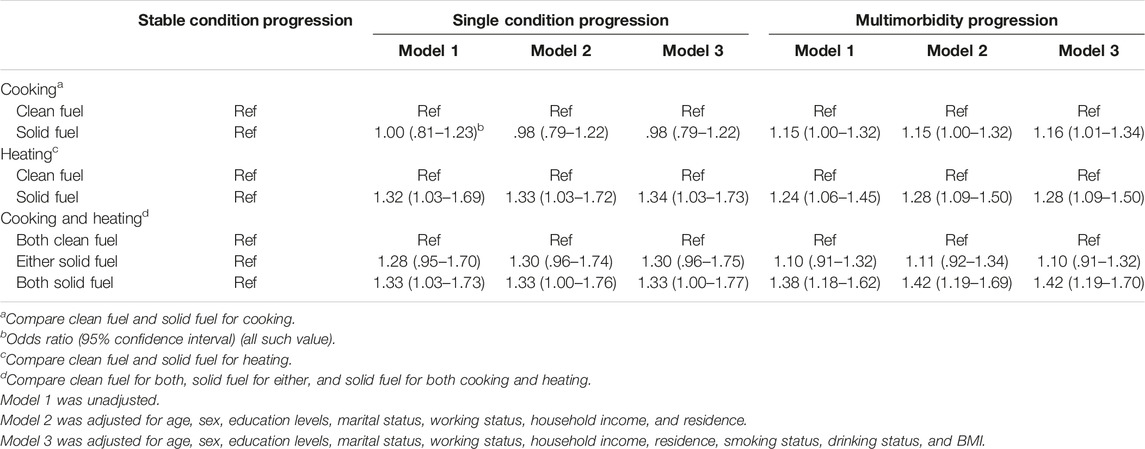
TABLE 3. Associations of solid fuel use with the progression of multimorbidity during follow-up (China Health and Retirement Longitudinal Study, China, 2011–2018).
Additional Analyses
Use of solid fuel for both cooking and heating was associated with most of the 12 single chronic conditions such as chronic lung diseases (adjusted OR: 1.38, 95% CI: 1.06–1.79), arthritis (adjusted OR: 1.42, 95% CI: 1.14–1.78), and memory-related diseases (adjusted OR: 2.30, 95% CI: 1.44–3.68), compared with clean fuel use for both (Supplementary Table S3). In the subgroup analyses (Supplementary Table S5), solid fuel use for both cooking and heating was associated with multimorbidity progression in urban (adjusted OR: 1.47, 95% CI: 1.12–1.93) and rural (adjusted OR: 1.38, 95% CI: 1.08–1.75), participants without multimorbidity at baseline (adjusted OR: 1.42, 95% CI: 1.05–1.91), and participants with multimorbidity at baseline (adjusted OR: 1.53, 95% CI: 1.13–2.08), compared with clean fuel use for both. The results from sensitivity analyses were similar to the main analysis (Supplementary Tables S6–S8). For example, solid fuel use for both cooking and heating was also associated with the progression of multimorbidity in participants without the selected conditions at baseline (adjusted OR: 1.28, 95% CI: .90–1.81) and defining electric or solar as clean fuel (adjusted OR: 1.41, 95% CI: 1.09–1.82), compared with clean fuel use for both. The participant who used 7 years or more of solid fuel for cooking was associated with multimorbidity progression (adjusted OR: 1.36, 95% CI: 1.13–1.62), compared with 0 years of solid fuel use for cooking.
Discussion
Based on the nationally representative cohort study of CHARLS, this study found that using solid fuels was significantly associated with the progression of multimorbidity, compared with clean fuel use. This highlights the role of household air pollution in controlling and preventing multimorbidity.
First, this study found that solid fuel use for cooking, heating, and for both cooking and heating were associated with multimorbidity progression, compared with clean fuel use, respectively. Our findings were consistent with a study that reported that solid fuel use was associated with the incidence of cardiometabolic multimorbidity (CMM) (hazard ratio [HR]: 1.71,95% CI: 1.28, 2.28) [29]. Our study added evidence on the disease burden of household air pollution, where previous studies had only estimated the disease-specific relative risk (RR) of single conditions like asthma (RR:1.23, 95% CI: 1.11–1.36) [12], and our study also highlighted the importance of reducing solid fuel use to prevent multimorbidity. However, only one previous study reported the association between solid fuel use and multimorbidity. Considering that people were more likely to develop multimorbidity as the population aged, 49.64% of the elderly in China were estimated to have multimorbidity in 2015 [16, 30]. Most previous studies also reported that people with multimorbidity were at higher risk of death, had a longer hospital stay, had a poorer quality of life, and had poorer physical function than those with a single chronic condition [31–33]. Therefore, more longitudinal and representative cohort studies were needed to explore risk factors of multimorbidity, providing more evidence about multimorbidity prevention for policymakers.
Second, this study identified that the association of solid fuel use for heating with the progression of multimorbidity was stronger than solid fuel use for cooking. One explanation for this result was that the utilization rate of solid fuels for heating was higher than that for cooking in this study (78.5% vs. 64.1%). Another potential reason was the different exposure patterns from cooking and heating that burning solid fuel for heating might be kept going all day in the winter months, often with poor ventilation, whereas cooking is kept going several times per day. Moreover, according to previous research [34, 35], burning solid fuel for heating creates more pollutants and a longer length of exposure than cooking, which may explain the higher association with the progression of multimorbidity. The burden of household air pollution remained high in the world’s regions contributing to 2.31 million deaths and 91.5 million DALYs in 2019 [36]. Considering solid fuel use for cooking and heating were two exposure patterns, leading to different health impacts on people, separate interventions for solid fuel use for cooking and heating were needed to reduce the adverse health impacts and burden of household air pollution effectively.
Third, this study also found that the joint effect of solid fuel use for both cooking and heating was stronger in urban than rural areas. The first explanation for this result was that in this study, the prevalence of multimorbidity at baseline was higher in urban than rural areas (34.5% vs. 34.4%) and participants with multimorbidity at baseline demonstrated a higher association between solid fuel use and multimorbidity progression than those without multimorbidity at baseline. It was consistent with previous studies which reported that people had a higher cumulative incidence of multimorbidity among those with the presence of ≥2 chronic conditions at baseline [37, 38]. The second explanation was that the prevalence of obesity in urban areas was higher than in rural areas (15.6% vs. 9.8%) in this study, many previous studies also reported that obesity was the risk factor for multimorbidity [39–41]. Another potential reason was that people living in urban areas were more likely to be exposed to outdoor air pollution such as urban traffic. Luo and his colleagues have reported that outdoor air pollution was associated with the development of CMM [42]. However, the information on outdoor air pollution was not collected in this study. Future research should consider this factor, which could explain the different relationships of solid fuel use and multimorbidity progression between urban and rural areas specifically.
Limitations and Strengths
The present study had some strengths. First, we provided prospective evidence on the association between solid fuel use and multimorbidity based on a relatively large sample size in a nationally representative cohort study in China. Second, the separate roles of solid fuel use for cooking and heating on multimorbidity were examined. Third, the sensitivity and subgroup analyses have confirmed the robustness of our results. Our study has some limitations that should be noted. First, as in other studies [29], information on solid fuel use at baseline was used to explore the association with multimorbidity progression without considering the changes in solid fuel use during follow-up. But we did the sensitivity analysis of estimating the association between the duration of solid fuel use for cooking from 2011 to 2018 and multimorbidity progression, which was consistent with our result. Second, as in other studies [43–45], the self-report use of solid fuel may be affected by reporting bias and using self-reported fuel use as a proxy for household air pollution without the levels of exposure separated by frequency of use of the solid fuel may not fully capture the extent of one’s exposure. Third, missing data on solid fuel use, chronic conditions, and covariates were excluded from this study and may be affected by select bias. Fourth, the information on seasonal, altitude, and temperature variations in the areas of the study, ventilation status when using solid fuel, and solid fuel use in the past which may relate to the exposure to household air pollution were not collected in this cohort study. We could not identify the influence of these factors on the association between solid fuel use and multimorbidity progression. Fifth, despite adjusting several covariates in our analyses, residual confounding remains a possibility.
Conclusion
This study showed that solid fuel use was associated with the progression of multimorbidity. Our findings indicate that reducing solid fuel use and promoting clean fuel use should be integrated into household air pollution for the control and the prevention of multimorbidity.
Author Contributions
TW: Conceptualization, methodology, software, visualization, writing-original draft preparation; YZ, ZZ, and XL: Writing-reviewing and editing; YZ: Software, validation; XX: Conceptualization, methodology, writing-reviewing and editing, supervision. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by Zhejiang University.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Acknowledgments
We sincerely thank those who were participants in the data collection and management of the China Health and Retirement Longitudinal Study.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2022.1605206/full#supplementary-material
References
1.WHO. WHO Guidelines for Indoor Air Quality: Household Fuel Combustion (2014). Avaialable from: https://www.who.int/publications/i/item/9789241548885 (Accessed June 06, 2022).
2.SGA. STATE OF GLOBAL AIR (2020). Avaialable from: https://www.stateofglobalair.org/ (Accessed June 06, 2022).
3.NEA. National Energy Administration. The Task of Solve the Electricityuse Problems of People without Access to Electricity Was Successfully Completed 2015 (2015). Avaialable from: https://english.www.gov.cn/state_council/2014/10/01/content_281474991089761.htm (Accessed June 06, 2022).
4. Mestl, HE, Aunan, K, Seip, HM, Wang, S, Zhao, Y, and Zhang, D. Urban and Rural Exposure to Indoor Air Pollution from Domestic Biomass and Coal Burning across China. Sci Total Environ (2007) 377(1):12–26. doi:10.1016/j.scitotenv.2007.01.087
5. Duan, X, Jiang, Y, Wang, B, Zhao, X, Shen, G, Cao, S, et al. Household Fuel Use for Cooking and Heating in China: Results from the First Chinese Environmental Exposure-Related Human Activity Patterns Survey (CEERHAPS). Appl Energ (2014) 136:692–703. doi:10.1016/j.apenergy.2014.09.066
6. Chen, B, Zhuang, Z, and Chen Xj, X. Field Survey on Indoor thermal Environment of Rural Residences with Coupled Chinese Kang and Passive Solar Collecting wall Heating in Northeast China. Solar Energy (2007) 81:781–90. doi:10.1016/j.solener.2006.09.004
7. Chen, Y, Shen, H, Smith, KR, Guan, D, Chen, Y, Shen, G, et al. Estimating Household Air Pollution Exposures and Health Impacts from Space Heating in Rural China. Environ Int (2018) 119:117–24. doi:10.1016/j.envint.2018.04.054
8. Liang, W, Wang, B, Shen, G, Cao, S, McSwain, B, Qin, N, et al. Association of Solid Fuel Use with Risk of Stunting in Children Living in China. Indoor Air (2020) 30(2):264–74. doi:10.1111/ina.12627
9. Luo, Y, Zhong, Y, Pang, L, Zhao, Y, Liang, R, and Zheng, X. The Effects of Indoor Air Pollution from Solid Fuel Use on Cognitive Function Among Middle-Aged and Older Population in China. Sci Total Environ (2021) 754:142460. doi:10.1016/j.scitotenv.2020.142460
10. Chan, KH, Yan, M, Bennett, DA, Guo, Y, Chen, Y, Yang, L, et al. Long-term Solid Fuel Use and Risks of Major Eye Diseases in China: A Population-Based Cohort Study of 486, 532 Adults. Plos Med (2021) 18(7):e1003716. doi:10.1371/journal.pmed.1003716
11. Lin, L, Wang, HH, Liu, Y, Lu, C, Chen, W, and Guo, VY. Indoor Solid Fuel Use for Heating and Cooking with Blood Pressure and Hypertension: A Cross-Sectional Study Among Middle-Aged and Older Adults in China. Indoor Air (2021) 31(6):2158–66. doi:10.1111/ina.12872
12. Lee, KK, Bing, R, Kiang, J, Bashir, S, Spath, N, Stelzle, D, et al. Adverse Health Effects Associated with Household Air Pollution: a Systematic Review, Meta-Analysis, and burden Estimation Study. Lancet Glob Health (2020) 8(11):e1427–34. doi:10.1016/S2214-109X(20)30343-0
13. Li, L, Yang, A, He, X, Liu, J, Ma, Y, Niu, J, et al. Indoor Air Pollution from Solid Fuels and Hypertension: A Systematic Review and Meta-Analysis. Environ Pollut (2020) 259:113914. doi:10.1016/j.envpol.2020.113914
14. Wang, F, Wang, J, Li, Y, Han, X, Hu, H, Yu, C, et al. Associations between Daily Cooking Duration and the Prevalence of Diabetes and Prediabetes in a Middle-Aged and Elderly Chinese Population: A Cross-Sectional Study. Indoor Air (2018) 28(2):238–46. doi:10.1111/ina.12434
15. Siddharthan, T, Grigsby, MR, Goodman, D, Chowdhury, M, Rubinstein, A, Irazola, V, et al. Association between Household Air Pollution Exposure and Chronic Obstructive Pulmonary Disease Outcomes in 13 Low- and Middle-Income Country Settings. Am J Respir Crit Care Med (2018) 197(5):611–20. doi:10.1164/rccm.201709-1861OC
16. Guo, X, Zhao, B, Chen, T, Hao, B, Yang, T, and Xu, H. Multimorbidity in the Elderly in China Based on the China Health and Retirement Longitudinal Study. PLoS One (2021) 16(8):e0255908. doi:10.1371/journal.pone.0255908
17. Xu, X, Mishra, GD, and Jones, M. Evidence on Multimorbidity from Definition to Intervention: An Overview of Systematic Reviews. Ageing Res Rev (2017) 37:53–68. doi:10.1016/j.arr.2017.05.003
18. Alkhatib, A, Nnyanzi, LA, Mujuni, B, Amanya, G, and Ibingira, C. Preventing Multimorbidity with Lifestyle Interventions in Sub-saharan Africa: A New Challenge for Public Health in Low and Middle-Income Countries. Int J Environ Res Public Health (2021) 18(23):12449. doi:10.3390/ijerph182312449
19. Zhao, Y, Zhao, S, Zhang, L, Haregu, TN, and Wang, H. Impacts of Multimorbidity on Medication Treatment, Primary Healthcare and Hospitalization Among Middle-Aged and Older Adults in China: Evidence from a Nationwide Longitudinal Study. BMC Public Health (2021) 21(1):1380. doi:10.1186/s12889-021-11456-7
20. Barnett, K, Mercer, SW, Norbury, M, Watt, G, Wyke, S, and Guthrie, B. Epidemiology of Multimorbidity and Implications for Health Care, Research, and Medical Education: a Cross-Sectional Study. The Lancet (2012) 380(9836):37–43. doi:10.1016/S0140-6736(12)60240-2
21. Zhao, Y, Hu, Y, Smith, JP, Strauss, J, and Yang, G. Cohort Profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol (2014) 43(1):61–8. doi:10.1093/ije/dys203
22. Liu, Y, Ning, N, Sun, T, Guan, H, Liu, Z, Yang, W, et al. Association between Solid Fuel Use and Nonfatal Cardiovascular Disease Among Middle-Aged and Older Adults: Findings from the China Health and Retirement Longitudinal Study (CHARLS). Sci Total Environ (2022) 856(2):159035. doi:10.1016/j.scitotenv.2022.159035
23. Yu, K, Qiu, G, Chan, KH, Lam, KH, Kurmi, OP, Bennett, DA, et al. Association of Solid Fuel Use with Risk of Cardiovascular and All-Cause Mortality in Rural China. JAMA (2018) 319(13):1351–61. doi:10.1001/jama.2018.2151
24. Balmes, JR. Household Air Pollution from Domestic Combustion of Solid Fuels and Health. J Allergy Clin Immunol (2019) 143(6):1979–87. doi:10.1016/j.jaci.2019.04.016
25. Yamamoto, SS, Yacyshyn, E, Jhangri, GS, Chopra, A, Parmar, D, and Jones, CA. Household Air Pollution and Arthritis in Low-And Middle-Income Countries: Cross-Sectional Evidence from the World Health Organization's Study on Global Ageing and Adult Health. PLoS One (2019) 14(12):e0226738. doi:10.1371/journal.pone.0226738
26. Cao, L, Zhao, Z, Ji, C, and Xia, Y. Association between Solid Fuel Use and Cognitive Impairment: A Cross-Sectional and Follow-Up Study in a Middle-Aged and Older Chinese Population. Environ Int (2021) 146:106251. doi:10.1016/j.envint.2020.106251
27. Wang, L, Zhou, B, Zhao, Z, Yang, L, Zhang, M, Jiang, Y, et al. Body-mass index and Obesity in Urban and Rural China: Findings from Consecutive Nationally Representative Surveys during 2004–18. The Lancet (2021) 398(10294):53–63. doi:10.1016/s0140-6736(21)00798-4
28. Li, C, Zhou, Y, and Ding, L. Effects of Long-Term Household Air Pollution Exposure from Solid Fuel Use on Depression: Evidence from National Longitudinal Surveys from 2011 to 2018. Environ Pollut (2021) 283:117350. doi:10.1016/j.envpol.2021.117350
29. Chen, W, Wang, X, Chen, J, You, C, Ma, L, Zhang, W, et al. Household Air Pollution, Adherence to a Healthy Lifestyle, and Risk of Cardiometabolic Multimorbidity: Results from the China Health and Retirement Longitudinal Study. Sci Total Environ (2022) 855:158896. doi:10.1016/j.scitotenv.2022.158896
30. Violan, C, Foguet-Boreu, Q, Flores-Mateo, G, Salisbury, C, Blom, J, Freitag, M, et al. Prevalence, Determinants and Patterns of Multimorbidity in Primary Care: a Systematic Review of Observational Studies. PLoS One (2014) 9(7):e102149. doi:10.1371/journal.pone.0102149
31. Yao, SS, Meng, X, Cao, GY, Huang, ZT, Chen, ZS, Han, L, et al. Associations between Multimorbidity and Physical Performance in Older Chinese Adults. Int J Environ Res Public Health (2020) 17(12):4546. doi:10.3390/ijerph17124546
32. Boult, C, and Wieland, GD. Comprehensive Primary Care for Older Patients with Multiple Chronic Conditions“Nobody Rushes You through”. JAMA (2010) 304(17):1936–43. doi:10.1001/jama.2010.1623
33. Lozano-Herna´ndezID, CM, Lo´pez-Rodrı´guez, JA, Leiva-Ferna´ndez, F, Calderon-Larranaga, A, Barrio-Cortes, J, Gimeno-Feliu, LA, et al. Social Support, Social Context and Nonadherence to Treatment in Young Senior Patients with Multimorbidity and Polypharmacy Followed-Up in Primary Care. MULTIPAP Study. MULTIPAP Study PLOSONE (2020) 15(6):e0235148. doi:10.1371/journal.pone.0235148
34. Li, J, Qin, C, Lv, J, Guo, Y, Bian, Z, Zhou, W, et al. Solid Fuel Use and Incident COPD in Chinese Adults: Findings from the China Kadoorie Biobank. Environ Health Perspect (2019) 127(5):57008. doi:10.1289/EHP2856
35. Xu, H, Li, Y, Guinot, B, Wang, J, He, K, Ho, KF, et al. Personal Exposure of PM2.5 Emitted from Solid Fuels Combustion for Household Heating and Cooking in Rural Guanzhong Plain, Northwestern China. Atmos Environ (2018) 185:196–206. doi:10.1016/j.atmosenv.2018.05.018
36. Murray, CJL, Aravkin, AY, Zheng, P, Abbafati, C, Abbas, KM, Abbasi-Kangevari, M, et al. Global burden of 87 Risk Factors in 204 Countries and Territories, 1990–2019: a Systematic Analysis for the Global Burden of Disease Study 2019. The Lancet (2020) 396(10258):1223–49. doi:10.1016/S0140-6736(20)30752-2
37. Ungprasert, P, Matteson, EL, and Crowson, CS. Increased Risk of Multimorbidity in Patients with Sarcoidosis: A Population-Based Cohort Study 1976 to 2013. Mayo Clin Proc (2017) 92(12):1791–9. doi:10.1016/j.mayocp.2017.09.015
38. Kudesia, P, Salimarouny, B, Stanley, M, Fortin, M, Stewart, M, Terry, A, et al. The Incidence of Multimorbidity and Patterns in Accumulation of Chronic Conditions: A Systematic Review. J Multimorb Comorb (2021) 11:26335565211032880. doi:10.1177/26335565211032880
39. Romano, E, Ma, R, Vancampfort, D, Firth, J, Felez-Nobrega, M, Haro, JM, et al. Multimorbidity and Obesity in Older Adults from Six Low- and Middle-Income Countries. Prev Med (2021) 153:106816. doi:10.1016/j.ypmed.2021.106816
40. Kivimäki, M, Kuosma, E, Ferrie, JE, Luukkonen, R, Nyberg, ST, Alfredsson, L, et al. Overweight, Obesity, and Risk of Cardiometabolic Multimorbidity: Pooled Analysis of Individual-Level Data for 120 813 Adults from 16 Cohort Studies from the USA and Europe. Lancet Public Health (2017) 2:e277–85. doi:10.1016/S2468-2667(17)30074-9
41. Kivimäki, M, Strandberg, T, Pentti, J, Nyberg, ST, Frank, P, Jokela, M, et al. Body-mass index and Risk of Obesity-Related Complex Multimorbidity: an Observational Multicohort Study. Lancet Diabetes Endocrinol (2022) 10:253–63. doi:10.1016/S2213-8587(22)00033-X
42. Luo, H, Zhang, Q, Yu, K, Meng, X, Kan, H, and Chen, R. Long-term Exposure to Ambient Air Pollution Is a Risk Factor for Trajectory of Cardiometabolic Multimorbidity: A Prospective Study in the UK Biobank. EBioMedicine (2022) 84:104282. doi:10.1016/j.ebiom.2022.104282
43. Qiu, S, Chen, X, Chen, X, Luo, G, Guo, Y, Bian, Z, et al. Solid Fuel Use, Socioeconomic Indicators and Risk of Cardiovascular Diseases and All-Cause Mortality: a Prospective Cohort Study in a Rural Area of Sichuan, China. Int J Epidemiol (2021).
44. Shao, J, Ge, T, Liu, Y, Zhao, Z, and Xia, Y. Longitudinal Associations between Household Solid Fuel Use and Depression in Middle-Aged and Older Chinese Population: A Cohort Study. Ecotoxicol Environ Saf (2021) 209:111833. doi:10.1016/j.ecoenv.2020.111833
Keywords: multimorbidity, cohort study, Chinese, household air pollution, solid fuel use
Citation: Wu T, Zhang Y, Zhou Y, Zhang Z, Cheng Y, Liu X and Xu X (2023) Solid Fuel Use and the Progression of Multimorbidity in Middle-Aged Chinese Participants: A Prospective Cohort Study. Int J Public Health 67:1605206. doi: 10.3389/ijph.2022.1605206
Received: 11 July 2022; Accepted: 13 December 2022;
Published: 09 January 2023.
Edited by:
Nino Kuenzli, Swiss Tropical and Public Health Institute (Swiss TPH), SwitzerlandReviewed by:
Bing Han, China Medical University, ChinaCopyright © 2023 Wu, Zhang, Zhou, Zhang, Cheng, Liu and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaolin Xu, xiaolin.xu@zju.edu.cn
 Tingting Wu1
Tingting Wu1 Xiaolin Xu
Xiaolin Xu