Abstract
Objectives: This study examined whether social capital (SC) mediated the association between internalized homophobia (IH) and condomless sex among men who have sex with men (MSM), with the interaction of SC and IH considered.
Methods: A cross-sectional study was conducted between November 2018 and April 2019 in Sichuan Province, China. A total of 540 participants were recruited to investigate their IH, SC, and condomless sex. A four-way decomposition of causal mediation analysis was used to test SC’s roles in the association between IH and condomless sex.
Results: Condomless sex was prevalent (46.7%) among the participants, which was significantly associated with IH [odds ratio (OR) = 1.70] and SC (OR = 0.55). A direct effect [excess risk ratio (RR = 0.32)] and an indirect effect (excess RR = 0.16) of SC were found to be significant in the association between IH and condomless sex. Heterogeneities in effects were observed when taking the SC’s domains (e.g., individual and family-based SC) as mediators. SC’s effects were significant only in the homosexual subgroup.
Conclusion: IH-based intervention with consideration of SC can be tailored to MSM to decrease condomless sex and curb the spread of HIV, especially for the homosexual subgroup.
Introduction
Globally, HIV has become a major public health issue among men who have sex with men (MSM) [1]. It has been reported that, compared to the general male population, MSM are 28 times more likely to be affected by HIV globally [2], and this difference is about 100 times in China [3]. The overall prevalence of HIV among Chinese MSM during 2001–2018 has been estimated to be 5.7% [4]. Besides, some other sexually transmitted infections (STIs), such as the syphilis epidemic [5], also have a higher prevalence in Chinese MSM. The higher risk for STIs among MSM is mainly due to sexual risk behaviors, such as condomless sex [6]. A meta-analysis has suggested that the rate of condomless sex in Chinese MSM was 55.2% in the past 6 months [7].
Internalized homophobia (IH) is the assemblage of negative attitudes toward homosexuality in general or homosexual features and behavior among sexual minorities [8,9]. According to Meyer’s conceptualization of the Minority Stress Theory, there are distal and proximal stressors unique and chronic for minority populations. IH is a form of stigma-related proximal stressor, attributed to distal stressors (e.g., acts of antigay discrimination and victimization) [10]. Moreover, IH is in the most proximal position along the continuum from environment to self [10]. In countries with heterosexism-dominated culture, discrimination and prejudice for MSM may be pervasive [11]. Even if one’s homosexuality is concealed, MSM may be harmed by social values toward self, especially in countries where collectivist culture is highly accepted [12]. From a different perspective, symbolic interaction theorists also contend that interactions with others are important for the development of a sense of self, and negative regard from others (e.g., stigma) leads to negative self-regard (e.g., IH) [13]. Persistent IH negatively impacts health, including low self-esteem, defenses that can lead to isolation [14], anxiety, depression, and suicidal ideation [15]. Importantly, IH has further effects on risky behavior such as condomless sex [16,17] due to a low level of self-validation, coping with psychological distress resulting from the perceived stigma, and temporarily escaping from shame and depression [18,19]. Besides, a higher level of IH might be related to more substance and alcohol use that may impair decision-making processes [20]. However, the results regarding the association between IH and condomless sex remain inconsistent [21], reflecting a need for more nuanced studies, such as examining the mediator or moderator [22].
In the past 20 years, there has been a pronounced increase in studies testing potential roles of social capital in health [23]. Social capital (SC), which was described as a source of support and benefits embodied in interpersonal and social networks [24], may play an essential mediation role between mental health and risky behaviors [25–27]. The social capital theory contends that the accumulation of human capital is determined by resources of social relationships [28]. However, whether individuals can access group-level resources (e.g., medical and health services) depends on many factors, including personality and mental health [10]. For those with high IH, some group-level resources (e.g., support from family, safer sex information from MSM community) may be difficult to access. For example, due to a high level of IH, some old MSM have been cut off from their family of origin [29]. Besides, MSM indicating greater IH are more isolated from the MSM community and are less likely to discuss HIV prevention with sexual partners [30]. Therefore, IH might show a direct effect on SC, and further affect health through SC. In addition, SC has been suggested to mitigate poor mental status (e.g., stigma, and depression) and condomless sex. For example, a study conducted among 98 male sex workers in the northeast of the US has found that SC acts as a buffer in the relationship between stigma and sexual risk behaviors [16]. This has suggested that when estimating mediation effects of SC, the potential interaction effect between SC and exposure should also be considered. A qualitative study has suggested that reducing IH and fostering SC are vital elements to improve the effectiveness of HIV risk prevention in this population [31]. Although this finding is encouraging, it is unclear whether and how SC may mediate the effect of IH on condomless sex.
Moreover, individuals of stigmatized groups generally evaluate themselves by comparing with others who look similar to them [10], and MSM who are non-homosexual men have a risk of double stigma cast by gays besides heterosexuals [32]. The previous study has also suggested that MSM who are non-homosexual subgroups may be exposed to more stressors and have more mental health problems than homosexual subgroups [33]. Therefore, the association of IH, SC and condomless sex should be considered separately in these two subgroups. Besides, different SC dimensions are worth concerning due to their different roles on health outcomes [34,35].
Prior work on examining mediation effects may be limited in considering the interaction between the mediator and exposure variables. This study aimed to examine the potential mediation effect of SC on the association between IH and condomless sex in Chinese MSM, with consideration of the interaction between SC and IH. We therefore incorporated a novel causal mediation analysis with a four-way decomposition approach, which is suitable in the presence of a mediator with which the exposure may interact [36] and can help understand how much of a total effect may be attributed to mediation, interaction, both mediation and interaction, or neither. These analyses could help design targeted intervention strategies to reduce risky sexual behaviors among MSM.
Methods
Subjects and Recruitment
The study was conducted from November 2018 to April 2019 in the Sichuan Province of China, where the estimated HIV prevalence was the highest in China [37]. Referring to the previous report [38], we selected the participants from cities that vary in the number of MSM to reduce the potential bias in cultural diversity and social interaction in the MSM community. Based on the information provided by the Sichuan Center for Disease Control and Prevention (CDC) and the estimates of the proportion of MSM people in 2018 by the Chengdu CDC [39], we estimated the numbers of MSM people in 35 cities of Sichuan Province, which were grouped into three layers by tertiles of the number of MSM people. One city in each layer was randomly selected as a study site.
Participants were recruited through snowball sampling, and the inclusion criteria were: 1) 16 years of age or older, 2) having engaged in anal sex with males for the past 6 months, and 3) having lived in Sichuan province for the past 3 months. We trained 15 investigators from two MSM communities and six colleges, and those trained investigators then recruited potential participants online (e.g., gay dating apps such as blued, and online chat platforms) and offline (e.g., bars, teahouses, bathhouses, groves and HIV testing clinics). Specifically, for online recruitment, investigators posted the flyer on chat platforms where potential participants could chat privately with the investigators. For offline recruitment, in addition to daily testing services, investigators visited gay bars at weekends and other gay sites (e.g., teahouse) three times a week for potential participants. Those who showed interest and accepted to participate in the investigation were assured of anonymity. An electronic questionnaire was sent to online participants, and a one-on-one interview was provided by investigators to offline participants. Details of the investigation process were described in a previous study [40]. All participants recruited offline were given 30 Chinese RMB (about US $4) as compensation for their time (about 20 min for a one-on-one interview). In addition, participants recruited offline were also provided free condoms and lubricants by the investigator.
Eligible participants were screened and provided written informed consent by electronic or pen signature. A total of 817 potential participants were contacted, of whom 540 met the inclusion criteria and were analyzed. This study was approved by the ethic committee of the West China School of Public Health and the West China Fourth Hospital and was conducted in accordance with the Declaration of Helsinki (1964).
Measurement
Outcome Variables
Participants reported whether they used condoms every time they had sex with a male partner for the past 6 months. The answer of “no” was considered as having condomless sex, which was used as the dependent variable.
Exposure Variables
The IH scale was designed according to the items of Nungesser’s inventory improved by Mayfield [8], and the IH scale of the Chinese version [41]. We modified and refined the IH scale into a 7-item scale due to the cultural differences, sensitive issues and potential response burden consideration [42]. Specifically, a panel consisting of two epidemiologists, one health psychologist, one sociologist, and four staff from gay health and culture communities participated in determining the original IH scale items. Some questions that may lead to misunderstandings due to cultural differences and some sensitive questions were screened out to obtain a 7-item scale. The scale was translated by the panel and modified in idiomatic expressions based on the feedback of the ten qualified MSM after a pre-test and panel discussion [40]. The IH scale included three dimensions: self-affirmation (one item), personal homonegativity (four items), and morality of homosexuality (two items) (Supplementary Table S1). Five-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree) was used for all items, of which three were reverse-scored items. The IH score was measured by summing up the scores of all items, and the total score ranged from 7 to 35, with a higher score indicating a higher level of IH. The Cronbach’s α value of the IH scale was 0.699.
Mediator
The SC scale in the study was drawn from the item pool of the Chinese version of Health-related Social Capital Measurement [43,44]. The 9-item SC scale included two dimensions: individual and family (IF)-based SC (5 items) and community and society (CS)- based SC (4 items) (Supplementary Table S2). Five-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree) was used for all items. The SC score was measured by summing up the scores of all items. The total score ranged from 9 to 45, with a higher total score indicating a higher level of SC. The Cronbach’s α value of the SC scale was 0.713.
Covariates
Demographic characteristics included age, sexual orientation, educational level, personal income, and employment status, which were considered covariates based on the knowledge of common causal precedents of both the exposure and outcome [45,46]. Besides, two HIV-related characteristics (i.e., HIV status and the number of sexual partners in the past 6 months) were also considered covariates due to their potential effects on condomless sex [47].
Statistical Analyses
Descriptive statistics for categorical data (frequencies and percentages) and continuous data [median and interquartile range (IQR)] were used. Univariate and adjusted analyses were used to examine the association between IH, SC, the interaction item (IH*SC), and condomless sex. Univariate odds ratio (ORu), adjusted odds ratio (AOR), and the respective 95% confidence interval (CI) were obtained. Furthermore, the causal mediation analysis was performed using the four-way decomposition method developed by Vander Weele [36,48], which provided detailed insight into the mediation roles of SC in the association of IH and condomless sex, with total effect decomposed into four components: controlled direct effect (CDE), reference interaction effect (INTref), mediated interaction effect (INTmed), and pure indirect effect (PIE). The specific paths and definition of four-way decomposition were presented in Figure 1 and Supplementary Table S3.
FIGURE 1
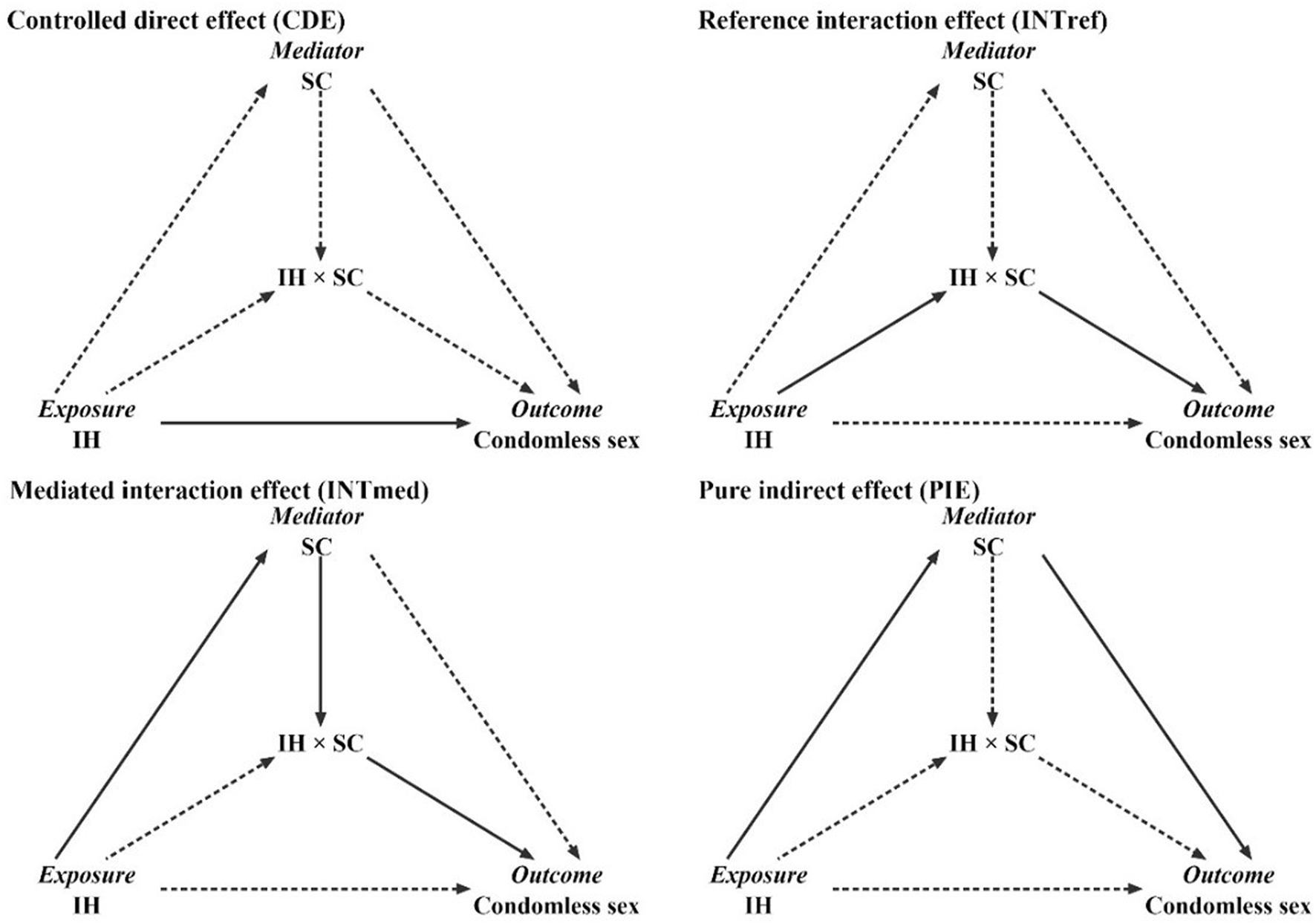
Conceptual framework of the data analysis in the current study (Chengdu, China, 2018–2019). A solid line represents a practical path, while a dashed line indicates that the path is blocked.
The four-way decomposition method is based on a counterfactual view that fixes the exposure of all participants at a low or high level and estimates whether and how the changes in the level of mediator could affect the relationship between the exposure and outcome [36]. In this study, with SC (i.e., total SC, IF-based SC, and CS-based SC) for each participant fixed at a high level (upper half of 50th percentile for the SC score), we compared the risks for condomless sex between those with a high IH (upper half of 50th percentile for the IH score) and a low IH (lower half of 50th percentile for the IH score). Besides, we plotted the IH estimates on condomless sex due to the four components, with SC fixed across the range from the minimum to the maximum observed scores. The estimates of the total effect and four components were presented as excess risk ratio (RR), i.e., RR minus 1. Finally, subgroup analysis regarding sexual orientation (i.e., homosexual, and non-homosexual subgroups) was conducted due to the difference in condom use and IH profiles [49,50].
We used Cronbach’s α calculation and factor analysis (with a prerequisite of KMO > 0.6) to test the validity and reliability of the IH and SC scales used in the study. Cronbach’s α showed acceptable reliability for criteria of 0.6 or higher [51]. Based on Patil’s method and selection criteria [41], screen tests and parallel analysis were used to suggest components in the SC and IH scales.
Data from the offline investigation were input and derived by Epidata 3.1. Data from the online investigation were derived from the questionnaire system (https://www.wjx.cn/). R software version 4.1.2 was used for data analysis; the statistical significance was defined as p < 0.05.
Results
Descriptive Statistics
A total of 540 MSM were included in our analysis. Their median age was 31 (21, 52) years. Most of them had a college degree or above (52.4%) and a personal income of less than 2,000 Chinese yuan (41.7%). Most of them were homosexual (65.2%), and employed/students (82.6%). The percentage of condomless sex in the past 6 months was 46.7%. The median total scores of IH and SC were 17 (13, 20) and 25 (22, 29), respectively (Table 1).
TABLE 1
| Variables | Median (IQR) or n (%) |
|---|---|
| Condomless sex in the past 6 months | |
| Yes | 252 (46.7) |
| No | 288 (53.3) |
| IH | 17 (13, 20) |
| SC | 25 (22, 29) |
| Age (years) | 31 (21, 52) |
| Homosexual | 352 (65.2) |
| Educational level | |
| Middle school or below | 172 (31.9) |
| High school/technical school | 85 (15.7) |
| College or above | 283 (52.4) |
| Personal income (in RMB) | |
| <2,000 | 225 (41.7) |
| 2,000–3,999 | 170 (31.5) |
| ≥4,000 | 145 (26.9) |
| Employed/student | 446 (82.6) |
| Number of sexual partners in the past 6 months | |
| 1 | 65 (12.0) |
| 2 | 212 (39.3) |
| 3 | 123 (22.8) |
| ≥4 | 140 (25.9) |
| HIV-positive | 37 (6.9) |
Characteristics of participants (n = 540) (Chengdu, China, 2018–2019).
Notes: IH, internalized homophobia; SC, social capital; IQR, interquartile range; RMB, “renminbi”, 1 USD = 6.99 RMB at the time of survey; STIs, sexually transmitted infections.
Association Between IH and Condomless Sex
IH (AOR = 1.700, 95% CI [1.154, 2.504]) showed a significantly positive association with condomless sex; SC (AOR = 0.554, 95% CI [0.380, 0.807]) suggested a significantly negative association with condomless sex. The interaction of IH and SC showed a significant and positive association with condomless sex (AOR = 1.303, 95% CI [1.115, 1.522]) (Supplementary Table S4).
Causal Mediation Analysis
In overall participants, with SC as a mediator and fixed at a high level (upper half of 50th percentile for the SC score), the total effect of IH on condomless sex was significant [excess risk ratio (RR) = 0.559], and can be decomposed into four parts (Table 2). The CDE (excess RR = 0.315, p < 0.05), i.e., the direct effect due to neither mediation nor interaction, was significant, and there was PIE (excess RR = 0.162, p < 0.05), i.e., mediation effect only without interaction, in the association between IH and condomless sex. The percentages attributable of the direct effect and mediation effect only were 56.4% and 29.0%, respectively. However, the effects due to INTref (i.e., interaction effect only without mediation), and the effects due to INTmed, i.e., both mediation and interaction effect, were not significant (p > 0.05). When the total SC was fixed at a value from 22 to 30, the excess RRs due to direct effect significantly declined; when the total SC was fixed at a value from 29 to 34, the excess RRs due to interaction effect only significantly increased (Figure 2).
TABLE 2
| Total SC | % | IF-based SC | % | CS-based SC | % | |
|---|---|---|---|---|---|---|
| Excess RR (95% CI) | Excess RR (95% CI) | Excess RR (95% CI) | ||||
| CDE | 0.315 (0.030, 0.730)** | 56.361 | 0.365 (0.093, 0.728)*** | 63.468 | 0.183 (−0.111, 0.473) | 30.541 |
| INTref | 0.144 (−0.031, 0.630) | 25.792 | 0.201 (−0.032, 0.690) | 34.916 | 0.321 (0.044, 0.715)** | 53.69 |
| INTmed | −0.062 (−0.415, 0.167) | −11.152 | −0.080 (−0.429, 0.073) | −13.972 | 0.069 (−0.042, 0.291) | 11.595 |
| PIE | 0.162 (0.034, 0.430)** | 28.998 | 0.090 (−0.002, 0.366) | 15.587 | 0.025 (−0.044, 0.133) | 4.175 |
| Total effect | 0.559 (0.169, 0.334)*** | 0.575 (0.121, 1.246)*** | 0.598 (0.109, 1.195)*** |
Effects of internalized homophobia on condomless sex due to mediation and interaction with social capital in overall participants (n = 540) (Chengdu, China, 2018–2019).
*p < 0.1, **p < 0.05, ***p < 0.01.
Analyses were adjusted by age, sexual orientation, educational level, personal income, employment status, number of sexual partners in the past 6 months, and HIV status.
%, proportion attributable; IH, internalized homophobia; SC, social capital; IF, individual and family; CS, community and society; CDE, controlled direct effect; INTref, reference interaction effect; INTmed, mediated interaction effect; PIE, pure indirect effect; RR, risk ratio.
FIGURE 2
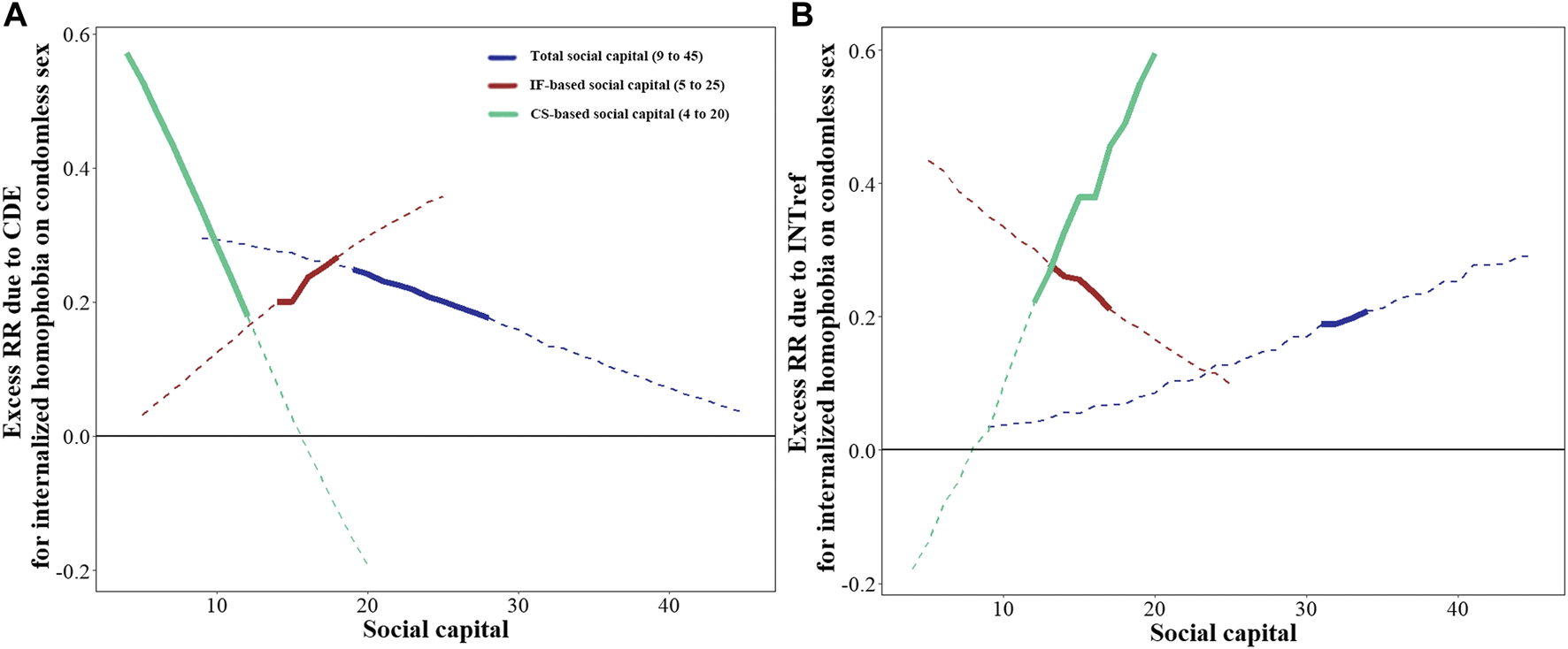
Excess risk ratio of internalized homophobia on condomless sex when social capital is fixed at a given value ranging from the minimum to the maximum observed scores in overall participants (Chengdu, China, 2018–2019). (A) Excess RR due to CDE when SC is fixed at a given value ranging from the minimum to the maximum observed scores. (B) Excess RR due to INTref when SC is fixed at a given value ranging from the minimum to the maximum observed scores. Values that range from the minimum to the maximum observed scores are listed in brackets. The solid line indicates that the excess RR is statistically significant, while the dotted line indicates that the excess RR is not statistically significant. Excess RR due to INTmed and PIE were relatively stable and therefore were not plotted (INTmed for total SC, around 0.150; for IF-based SC, around 0.003; for CS-based SC, around 0.166. PIE for total SC, around 0.156; for IF-based SC, around 0.169, for CS-based SC, around 0.039). Analyses were adjusted by age, sexual orientation, educational level, personal income, employment status, number of sexual partners in the past 6 months, and HIV status. IH, internalized homophobia; SC, social capital; IF, individual and family; CS, community and society; CDE, controlled direct effect; INTref, reference interaction effect; INTmed, mediated interaction effect; PIE, pure indirect effect; RR, risk ratio.
With IF-based SC as a mediator and fixed at a high level, the excess RRs due to total effect and directed effect were 0.575 and 0.365 (all p < 0.01) (Table 2). With the score of IF-based SC increased, the excess RRs due to direct effect increased while due to interaction effect only showed an adverse trend (Figure 2).
With CS-based SC as a mediator and fixed at a high level, excess RRs due to total effect (excess RR = 0.598, p < 0.01) and interaction effect only (excess RR = 0.321, p < 0.05) were observed (Table 2). With the score of CS-based SC increased, the excess RRs due to interaction effect only increased while due to direct effect decreased (Figure 2).
Subgroup Analysis
The proportion of participants with condomless sex and high IH in the homosexual subgroup was lower than that in the non-homosexual subgroup. In comparison, the proportion of participants with high SC was higher in the homosexual subgroup (Supplementary Figure S1).
In the homosexual subgroup, when taking SC as a mediator and fixed at a high level, we observed significant excess RR due to total effect (excess RR = 0.854, p < 0.05) and mediation effect only (excess RR = 0.332, p < 0.05). Taking the IF-based SC or CS-based SC as mediators respectively and fixed at a high level, we found excess RR due to the total effect was significant, while heterogeneity of significant effect was observed in the directed effect and interaction effect only (Table 3). With the score of IF-based SC increased, excess RRs due to directed effect increased while excess RRs due to interaction effect only decreased; with the score of CS-based SC increased, we observed a decreased excess RR due to directed effect while an increased excess RR due to interaction effects only (Figure 3). However, in the non-homosexual subgroup, with SC or its two domains as mediators, excess RR due to four parts were all not significant at any score of SC (p > 0.05) (Figure 3; Table 3).
TABLE 3
| Total SC | % | IF-based SC | % | CS-based SC | % | |
|---|---|---|---|---|---|---|
| Excess RR (95% CI) | Excess RR (95% CI) | Excess RR (95% CI) | ||||
| Homosexual (n = 352) | ||||||
| CDE | 0.329 (−0.124, 0.745) | 38.48 | 0.615 (0.222, 1.140)*** | 79.186 | 0.224 (−0.127, 0.785) | 27.921 |
| INTref | 0.192 (−0.028, 0.975) | 22.487 | 0.325 (−0.042, 1.082) | 41.934 | 0.437 (0.082, 1.042)** | 54.575 |
| INTmed | 0.002 (−0.386, 0.481) | 0.14 | −0.305 (−0.890, 0.013) | −39.302 | 0.125 (−0.149, 0.425) | 15.584 |
| PIE | 0.332 (0.073, 0.696)** | 38.891 | 0.141 (−0.023, 0.384) | 18.182 | 0.015 (−0.071, 0.164) | 1.92 |
| Total effect | 0.854 (0.119, 1.763)** | 0.776 (0.181, 1.821)** | 0.801 (0.135, 1.743)** | |||
| Non-homosexual (n = 188) | ||||||
| CDE | 0.200 (−0.106, 0.975) | 73.436 | 0.059 (−0.234, 0.737) | 23.035 | 0.059 (−0.234, 0.737) | 23.035 |
| INTref | 0.058 (−0.293, 1.292) | 21.492 | 0.133 (−0.165, 1.194) | 52.14 | 0.133 (−0.166, 1.194) | 52.14 |
| INTmed | −0.075 (−1.056, 0.073) | −27.814 | 0.027 (−0.226, 0.503) | 10.431 | 0.027 (−0.226, 0.503) | 10.431 |
| PIE | 0.089 (−0.020,1.135) | 32.886 | 0.037 (−0.084, 0.674) | 14.395 | 0.037 (−0.084, 0.674) | 14.395 |
| Total effect | 0.272 (−0.341, 1.451) | 0.256 (−0.255, 1.926) | 0.256 (−0.255, 1.926) |
Effects of internalized homophobia on condomless sex due to mediation and interaction with social capital in different sexual orientation groups (Chengdu, China, 2018–2019).
*p < 0.1, **p < 0.05, ***p < 0.01.
Analyses were adjusted by age, sexual orientation, educational level, personal income, employment status, number of sexual partners in the past 6 months, and HIV status.
%, proportion attributable; IH, internalized homophobia; SC, social capital; IF, individual and family; CS, community and society; CDE, controlled direct effect; INTref, reference interaction effect; INTmed, mediated interaction effect; PIE, pure indirect effect; RR, risk ratio.
FIGURE 3
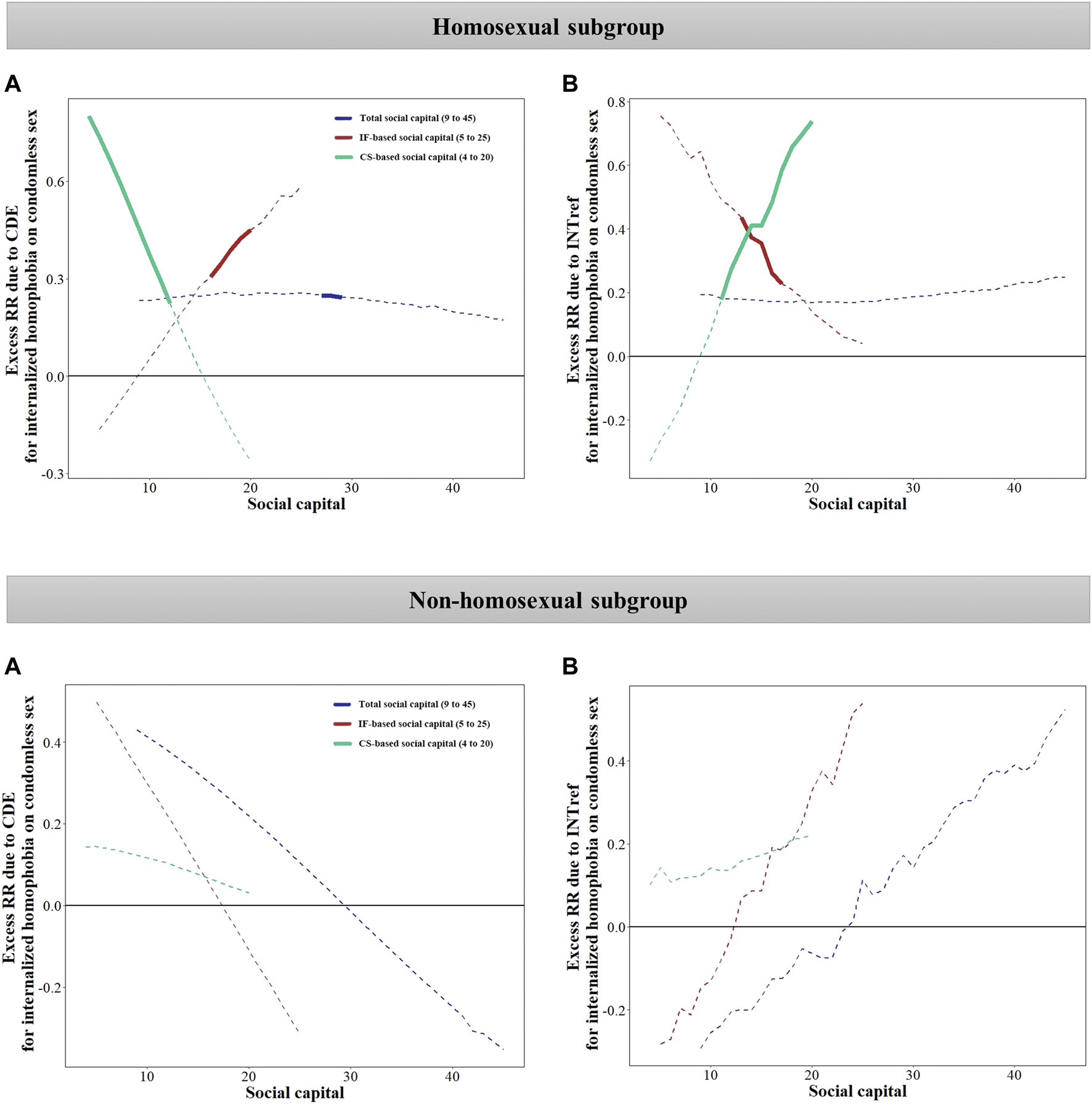
Excess risk ratio of internalized homophobia on condomless sex when social capital is fixed at a given value ranging from the minimum to the maximum observed scores in subgroups (Chengdu, China, 2018–2019). (A) Excess RR due to CDE when SC is fixed at a given value ranging from the minimum to the maximum observed scores. (B) Excess RR due to INTref when SC is fixed at a given value ranging from the minimum to the maximum observed scores. Values that range from the minimum to the maximum observed scores are listed in brackets. The solid line indicates that the excess RR is statistically significant, while the dotted line indicates that the excess RR is not statistically significant. Excess RR due to INTmed and PIE was stable and not plotted. Analyses were adjusted by age, sexual orientation, educational level, personal income, employment status, number of sexual partners in the past 6 months, and HIV status. IH, internalized homophobia; SC, social capital; IF, individual and family; CS, community and society; CDE, controlled direct effect; INTref, reference interaction effect; INTmed, mediated interaction effect; PIE, pure indirect effect; RR, risk ratio.
Discussion
This study on Chinese MSM suggested that IH and SC were closely associated with condomless sex. Using a novel four-way composition method, we found that for those with a high level of SC, IH is still a risk factor for condomless sex. Improving SC could reduce and/or mitigate the negative effect of IH on condomless sex, with heterogeneity observed in different domains of SC. Such a mechanism was only found in the homosexual subgroup.
Social connections may have “mixed” effects and paradoxically exacerbate the effect of IH, especially if such connections entail role strain associated with obligations to provide social support to others (e.g., a man was supported and expected to carry on the family line) [52]. The heterogeneity of results in the IF-based SC and CS-based SC might be attributed to the “mixed” effects. Specifically, for CS-based SC, our study reinforced the evidence that reduction of IH could decrease condomless sex by encouraging community participation and improving government support [26,31]. In contrast to the CS-based SC, however, we observed an adverse trend for IF-based SC, i.e., the risk of condomless sex due to the direct effect of IH increased when IF-based SC was fixed at a higher level. The higher IF-based SC may be explained by the support from family members and MSM peers, which might result in more social interaction among MSM. However, for those with a high level of IH, family obligations based on strong IF-based SC become a possible stressor [52], and access to social support from other sexual minorities might be restricted [53]. They also suffer more adverse mental status (e.g., anxiety, low condom use self-efficacy) [15,54] and behavior (e.g., substance use) [20], increasing their condomless sex behavior. Besides, subgroup analysis suggested that the risk of condomless sex due to IH and the mediation and interaction effect of SC were only significant in the homosexual subgroups. However, similar to a recent study in Kazakhstan [55], our findings suggested that the non-homosexual population reported a higher level of IH, more condomless sex, and a lower level of SC than their counterpart.
We provided new findings that deserve discussion using the causal mediation analysis with the four-way method. First, with total SC fixed at a high level, mediation effects of total SC contributed significantly to the total effect, highlighting the dominant role of SC as a mediator between IH and condomless sex in MSM. Second, we found that even attained a high level of SC, MSM with a high level of IH still had a higher risk of condomless sex than those with a low level of IH. For those with a high level of SC, structural stigma may still shape the fear of being stigmatized and crisis sense of support loss from social contacts (e.g., family members, colleagues) [56,57]. External prejudice events (i.e., distal stressors) and IH might further increase the risk of condomless sex. This finding suggested that joint intervention of reducing IH and fostering SC should be designed to improve the effectiveness of HIV risk prevention [31]. Third, we found that a higher IF-based SC may not mediate or mitigate the effect of IH on condomless sex; however, risk attributable to interactions gradually increased with the improvement of CS-based SC. Those with enough community support can obtain more available health services, and self-efficacy in safe sex also mitigates the effect of IH [58].
The findings on the relationship between IH and risky sexual behavior seem mixed since the first definition of IH was proposed [59]. Williamson’s review revealed some inconsistent evidence about IH and risky sexual behavior [17]. Our study on Chinese MSM suggested a significant association of IH with condomless sex, which is in line with the findings in the US [20,30], Israel [60], and Ugandan [61]. However, inconsistencies also exist [21,62], which might be explained by one or more potential moderators [21]. Since the previous study proposed the need for more nuanced studies, such as examining the mediator or moderator [22], we, therefore, extended our previous study, which focused on the relationship between IH and sexual risk behavior [63], considering the potential role of SC in the association between IH and condomless sex. More evidence is still needed to better understand the effect of IH on condomless sex through other factors.
Our findings have strong policy implications. Although homosexuality and same-sex sexual behavior were no longer considered a disease since 2001, homosexuality is still not widely accepted [9], with structural stigma and prejudice leading to a high level of IH among Chinese MSM [64]. A previous report showed that nearly 85% of Chinese MSM kept their homosexuality secret [65]. In recent years, the Chinese government has issued some policies to enhance health service delivery for MSM [66], while mental health services for this population are still lacking [15]. As our findings suggested, those with both high SC and IH still had a high risk of condomless sex. These findings provided information on the professions or service providers of the indispensable reduction of psychological problems and minority stress like IH and to improve the family, community, and social support towards MSM to mitigate the impact of IH on condomless sex [15,26,31,67]. Further efforts are needed at civil and political levels to address structural discrimination, establish a supportive environment and strengthen peer support [68,69].
Several limitations should be mentioned in our study. First, we used a health-related SC scale for the general population and could not differentiate the SC from MSM and non-MSM peers. The estimates due to mediations and moderation of peer-related SC may differ, which requires future research. Second, the reporting bias might exist, especially for some information such as sexual orientation. However, we used anonymous questionnaires to reduce this bias as much as possible. Third, findings from the participants in Sichuan may not be generalized without caution to the overall MSM in China. Fourth, we adopted a non-probability sampling and cannot guarantee the representativeness of the total sample. Fifth, some potential covariates (e.g., pre-exposure prophylaxis use) were not included in our study, which may lead to an overestimation of the contribution of IH to the risk for condomless sex.
Conclusions
Our study identified the mediating role of SC in the association between IH and condomless sex among Chinese MSM, and SC interacts with IH. IH is still a risk factor for condomless sex for those with a high level of SC, especially for MSM identified as homosexual. IH-based intervention with consideration of SC can be tailored to this group to decrease condomless sex and curb the spread of HIV.
Statements
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics committee of the West China School of Public Health and the West China Fourth Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
BY and SY had taken a principal role in the study conception, design and methodologies, and drafting the manuscript. SY, XY, ZW, HZ, and PJ contributed to the writing of the study protocol and made revisions to the manuscript. BY, SY, and CF contributed to the material preparation and data analysis. All authors read and approved the final manuscript.
Funding
This study was funded by the National Natural Science Foundation of China (81703279), Liangshan Key R&D Projects of Science and Technology (2021DYF0045), Sichuan Provincial Foundation for AIDS Prevention and Control (2022ZC02, 2021ZC01, 2020zc05, 2020zc04, 2019sc01, 2018-WJW-03), Wuhan University Specific Fund for Major School-level Internationalization Initiatives (WHU-GJZDZX-PT07), and the International Institute of Spatial Lifecourse Health (ISLE).
Acknowledgments
The authors would like to thank the Center for AIDS/STD Control and Prevention, Sichuan Center for Disease Control and Prevention, the devoted investigators of gay communities for their contributions.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2023.1605202/full#supplementary-material
References
1
Xu JJ Tang WM Zou HC Mahapatra T Hu QH Fu GF et al High HIV Incidence Epidemic Among Men Who Have Sex with Men in china: Results from a Multi-Site Cross-Sectional Study. Infect Dis Poverty (2016) 5:82. 10.1186/s40249-016-0178-x
2
Liu ZSO Yan Q Fang Q Zuo J Chen Y Chen X et al Changing Epidemiological Patterns of HIV and AIDS in China in the post-SARS Era Identified by the Nationwide Surveillance System. BMC Infect Dis (2018) 18:700. 10.1186/s12879-018-3551-5
3
Wang HY Xu JJ Zou HC Reilly KH Zhang CM Yun K et al Sexual Risk Behaviors and HIV Infection Among Men Who Have Sex with Men and Women in China: Evidence from a Systematic Review and Meta-Analysis. Res Int (2015) 2015:850132. 10.1155/2015/850132
4
Dong MJ Peng B Liu ZF Ye QN Liu H Lu XL et al The Prevalence of HIV Among MSM in China: a Large-Scale Systematic Analysis. BMC Infect Dis (2019) 19:1000. 10.1186/s12879-019-4559-1
5
Wu ZY Xu J Liu E Mao Y Xiao Y Sun X et al HIV and Syphilis Prevalence Among Men Who Have Sex with Men: A Cross-Sectional Survey of 61 Cities in China. Clin Infect Dis (2013) 57:298–309. 10.1093/cid/cit210
6
Blashill AJ Wilson JM O'Cleirigh CM Mayer KH Safren SA . Examining the Correspondence between Relationship Identity and Actual Sexual Risk Behavior Among HIV-Positive Men Who Have Sex with Men. Arch Sex Behav (2014) 43:129–37. 10.1007/s10508-013-0209-7
7
Huang Q Li Q Li Y Zeng G Cui X Yan P et al [Prevalence of HIV Infection and Syphilis, Sexual Behaviors and Awareness of HIV/AIDS Related Knowledge Among Men Who Have Sex with Men in China: a Meta-Analysis of Data Collected from 2010 to 2013. Zhonghua Liu Xing Bing Xue Za Zhi (2015) 36:1297–304.
8
Mayfield W . The Development of an Internalized Homonegativity Inventory for Gay Men. J Homosex (2001) 41:53–76. 10.1300/J082v41n02_04
9
Neilands TB Steward WT Choi KH . Assessment of Stigma towards Homosexuality in China: a Study of Men Who Have Sex with Men. Arch Sex Behav (2008) 37:838–44. 10.1007/s10508-007-9305-x
10
Meyer IH . Prejudice, Social Stress, and Mental Health in Lesbian, Gay, and Bisexual Populations: Conceptual Issues and Research Evidence. Psychol Bull (2003) 129:674–97. 10.1037/0033-2909.129.5.674
11
Zhou YR Homosexuality, Seropositivity, and Family Obligations: Perspectives of HIV-Infected Men Who Have Sex with Men in China Cult Health Sex, 8 (2006). p. 487–500. 10.1080/13691050600847455
12
Zang C Guida J Sun Y Liu H . Collectivism Culture, HIV Stigma and Social Network Support in Anhui, China: a Path Analytic Model. AIDS Patient Care STDS (2014) 28:452–8. 10.1089/apc.2014.0015
13
Aksan N Kısac B Aydın M Demirbuken S . Symbolic Interaction Theory. Symbolic interaction Theor Proced - Soc Behav Sci (2009) 1:902–4. 10.1016/j.sbspro.2009.01.160
14
Cuca YP Asher A Okonsky J Kaihura A Dawson-Rose C Webel A . HIV Stigma and Social Capital in Women Living with HIV. J Assoc Nurses AIDS Care (2017) 28:45–54. 10.1016/j.jana.2016.09.001
15
Sun S Pachankis JE Li X Operario D . Addressing Minority Stress and Mental Health Among Men Who Have Sex with Men (MSM) in China. Curr Hiv/aids Rep (2020) 17:35–62. 10.1007/s11904-019-00479-w
16
Valente PK Mimiaga MJ Mayer KH Safren SA Biello KB Social Capital Moderates the Relationship between Stigma and Sexual Risk Among Male Sex Workers in the US Northeast AIDS Behav, 24 (2020). p. 29–38. 10.1007/s10461-019-02692-5
17
Williamson IR . Internalized Homophobia and Health Issues Affecting Lesbians and Gay Men. Educ Res (2000) 15:97–107. 10.1093/her/15.1.97
18
Earnshaw VA Bogart LM Dovidio JF Williams DR . Stigma and Racial/ethnic HIV Disparities: Moving toward Resilience. Am Psychol (2013) 68:225–36. 10.1037/a0032705
19
Valdiserri RO . HIV/AIDS Stigma: an Impediment to Public Health. Am J Public Health (2002) 92:341–2. 10.2105/ajph.92.3.341
20
Puckett JA Newcomb ME Garofalo R Mustanski B . Examining the Conditions under Which Internalized Homophobia Is Associated with Substance Use and Condomless Sex in Young MSM: the Moderating Role of Impulsivity. Ann Behav Med (2017) 51:567–77. 10.1007/s12160-017-9878-0
21
Newcomb ME Mustanski B . Moderators of the Relationship between Internalized Homophobia and Risky Sexual Behavior in Men Who Have Sex with Men: a Meta-Analysis. Arch Sex Behav (2011) 40:189–99. 10.1007/s10508-009-9573-8
22
Ross MW Rosser BR Smolenski D . The Importance of Measuring Internalized Homophobia/homonegativity. Arch Sex Behav (2010) 39:1207–8. 10.1007/s10508-010-9634-z
23
Moore S Kawachi I . Twenty Years of Social Capital and Health Research: a Glossary. J Epidemiol Community Health (2017) 71:513–7. 10.1136/jech-2016-208313
24
Portes A Social Capital: Its Origins and Applications in Modern Sociology Annual Review of Sociology, 24 (1998). p. 1–24. 10.1146/annurev.soc.24.1.1
25
Chan SA-OX Chung GKK Chan YH Woo J Yeoh EK Chung RYN et al The Mediating Role of Individual-Level Social Capital Among Worries, Mental Health and Subjective Well-Being Among Adults in Hong Kong during the COVID-19 Pandemic. Curr Psychol (2021) 1–11. 10.1007/s12144-021-02316-z
26
Restar A Ogunbajo A Adia A Nazareno J Hernandez L Sandfort T et al Using Structural Equation Modelling to Characterise Multilevel Socioecological Predictors and Mediators of Condom Use Among Transgender Women and Cisgender Men Who Have Sex with Men in the Philippines. Glob Health (2020) 5:e002463. 10.1136/bmjgh-2020-002463
27
Sun Q Lu N . Social Capital and Mental Health Among Older Adults Living in Urban China in the Context of COVID-19 Pandemic. Int J Environ Res Public Health (2020) 17:7947. 10.3390/ijerph17217947
28
Machalek R Martin MW . Sociobiology and Sociology: A New Synthesis. In: WrightJD, editor. International Encyclopedia of the Social & Behavioral Sciences. 2nd ed. Oxford: Elsevier (2015). p. 892–8. 10.1016/B978-0-08-097086-8.32010-4
29
Goldhammer H Krinsky L Keuroghlian AS . Meeting the Behavioral Health Needs of LGBT Older Adults. J Am Geriatr Soc (2019) 67:1565–70. 10.1111/jgs.15974
30
Crosby RA Salazar LF Mena L Geter A . Associations between Internalized Homophobia and Sexual Risk Behaviors Among Young Black Men Who Have Sex with Men. Transm Dis (2016) 43:656–60. 10.1097/OLQ.0000000000000505
31
Garcia J Parker C Parker RG Wilson PA Philbin M Hirsch JS . Psychosocial Implications of Homophobia and HIV Stigma in Social Support Networks: Insights for High-Impact HIV Prevention Among Black Men Who Have Sex with Men. Educ Behav (2016) 43:217–25. 10.1177/1090198115599398
32
Ryan WS Blascovich J . Chapter 25 - Measures of Attitudes towards Sexual Orientation: Heterosexism, Homophobia, and Internalized Stigma. In: BoyleGJSaklofskeDHMatthewsG, editors. Measures of Personality and Social Psychological Constructs. San Diego: Academic Press (2015). p. 719–51. 10.1016/B978-0-12-386915-9.00025-5
33
Jorm AF Korten AE Rodgers B Jacomb PA . Sexual Orientation and Mental Health: Results from a Community Survey of Young and Middle-Aged Adults. Br J Psychiatry (2002) 180:423–7. 10.1192/bjp.180.5.423
34
Alvarez EC Kawachi I Romani JR . Family Social Capital and Health - a Systematic Review and Redirection. Sociol Health Illn (2017) 39:5–29. 10.1111/1467-9566.12506
35
He L Yu B Yu J Xiong J Huang Y Xie T et al The Impact of Social Capital and Mental Health on Medication Adherence Among Older People Living with HIV (PLWH). BMC Public Health (2021) 21:2252. 10.1186/s12889-021-12251-0
36
VanderWeele TJ A Unification of Mediation and Interaction: A 4-way Decomposition Epidemiology, 25 (2014). p. 749–61. 10.1097/EDE.0000000000000121
37
Huang W Wang L Guodong M Zahn RJ Taussig J Peterson SR et al HIV Incidence Among Men Who Have Sex with Men in mainland China: a Systematic Review Protocol. Syst Rev (2021) 10:277. 10.1186/s13643-021-01828-w
38
Stueve A O'Donnell LN Duran R San Doval AJB . Time-space Sampling in Minority Communities: Results with Young Latino Men Who Have Sex with Men. Am J Public Health (2001) 91:922–6. 10.2105/ajph.91.6.922
39
Dai Z Wang XD Liu F Duan ZH Shi YY Zhang S et al Applying Multiplier Method to Estimate the Population Size of Active MSM in Chengdu Based on Social App Data. Mod Prev Med (2019) 46:4421–3.
40
Huang Y Yu B Jia P Wang Z Yang S Tian C et al Association between Psychological Factors and Condom Use with Regular and Nonregular Male Sexual Partners Among Chinese MSM: A Quantitative Study Based on the Health Belief Model. Res Int (2020) 2020:5807162. 10.1155/2020/5807162
41
Ren Z Hood RW Jr . Internalized Homophobia Scale for Gay Chinese Men: Conceptualization, Factor Structure, Reliability, and Associations with Hypothesized Correlates. Am J Mens Health (2018) 12:1297–306. 10.1177/1557988318768603
42
Rolstad S Adler J Ryden A . Response burden and Questionnaire Length: Is Shorter Better?A Rev meta-analysis Value Health (2011) 14:1101–8. 10.1016/j.jval.2011.06.003
43
Chen RHX Gao B . [Establishment of an index System for Evaluation on Health-Related Social Capital for New Urban Immigrants in China] Chinese. J Public Health (2019) 36:1055–7. 10.11847/zgggws1121292
44
Han J Jia P Huang Y Gao B Yu B Yang S et al Association between Social Capital and Mental Health Among Older People Living with HIV: The Sichuan Older HIV-Infected Cohort Study (SOHICS). BMC Public Health (2020) 20:581. 10.1186/s12889-020-08705-6
45
Chuang DM Newman PA Fang L Lai MC . Syndemic Conditions, Sexual Risk Behavior, and HIV Infection Among Men Who Have Sex with Men in Taiwan. AIDS Behav (2021) 25:3503–18. 10.1007/s10461-021-03269-x
46
VanderWeele TJ Shpitser I . A New Criterion for Confounder Selection. Biometrics (2011) 67:1406–13. 10.1111/j.1541-0420.2011.01619.x
47
Ofreneo MAP Gamalinda TB Canoy NA . Culture-embedded Drivers and Barriers to (Non) Condom Use Among Filipino MSM: a Critical Realist Inquiry. AIDS Care (2021) 33:1430–5. 10.1080/09540121.2020.1801979
48
Discacciati A Bellavia A Lee JJ Mazumdar M Valeri L . Med4way: a Stata Command to Investigate Mediating and Interactive Mechanisms Using the Four-Way Effect Decomposition. Int J Epidemiol (2018) 48:15–20. 10.1093/ije/dyy236
49
Kim JS Kim K Kwak Y . Differences in Risky Sexual Behavior According to Sexual Orientation in Korean Adolescents. J Homosex (2019) 66:17–30. 10.1080/00918369.2017.1392134
50
Tskhay KO Rule NO . Internalized Homophobia Influences Perceptions of Men's Sexual Orientation from Photos of Their Faces. Arch Sex Behav (2017) 46:755–61. 10.1007/s10508-015-0628-8
51
Taber KS . The Use of Cronbach’s Alpha when Developing and Reporting Research Instruments in Science Education. Sci Educ Res Sci Educ (2018) 48:1273–96. 10.1007/s11165-016-9602-2
52
Kawachi I Berkman LF . Social Ties and Mental Health. J Urban Health (2001) 78:458–67. 10.1093/jurban/78.3.458
53
Friedman MR Bukowski L Eaton LA Matthews DD Dyer TV Siconolfi D et al Psychosocial Health Disparities Among Black Bisexual Men in the U.S.: Effects of Sexuality Nondisclosure and Gay Community Support. Arch Sex Behav (2019) 48:213–24. 10.1007/s10508-018-1162-2
54
Dawson EL Mendoza MCB Gaul Z Jeffries Iv WL Sutton MY Wilson PA . Resilience, Condom Use Self-Efficacy, Internalized Homophobia, and Condomless Anal Sex Among Black Men Who Have Sex with Men, New York City. New York City PLoS One (2019) 14:e0215455. 10.1371/journal.pone.0215455
55
Paine EA Lee YG Vinogradov V Zhakupova G Hunt T Primbetova S et al HIV Stigma, Homophobia, Sexual and Gender Minority Community Connectedness and HIV Testing Among Gay, Bisexual, and Other Men and Transgender People Who Have Sex with Men in Kazakhstan. Kazakhstan AIDS Behav (2021) 25:2568–77. 10.1007/s10461-021-03217-9
56
Stojanovski KA-O King EJ Amico KR Eisenberg MC Geronimus AT Baros S Schmidt AJ Stigmatizing Policies Interact with Mental Health and Sexual Behaviours to Structurally Induce HIV Diagnoses Among European Men Who Have Sex with Men AIDS Behav, 26 (2022). p. 3400–10. 10.1007/s10461-022-03683-9
57
Feng Y Wu Z Detels R . Evolution of Men Who Have Sex with Men Community and Experienced Stigma Among Men Who Have Sex with Men in Chengdu, China. J Acquir Immune Defic Syndr (2011) 53:S98–103. 10.1097/QAI.0b013e3181c7df71
58
Calvo V Cusinato M Meneghet N Miscioscia M . Perceived Social Support Mediates the Negative Impact of Insecure Attachment Orientations on Internalized Homophobia in Gay Men. J Homosex (2021) 68:2266–84. 10.1080/00918369.2020.1734378
59
Sprecher S McKinney K . Sexuality. Thousand Oaks, California: SAGE Publications, Inc (1993). 10.4135/9781483326252
60
Michael S . Internalized Homophobia and Sexual Risk Behavior Among HIV-Infected Men Who Have Sex with Men in Israel. Soc Work Health Care (2020) 59:709–24. 10.1080/00981389.2020.1859045
61
Ross MW Kajubi P Mandel JS McFarland W Raymond HF . Internalized Homonegativity Homophobia Is Associated with HIV-Risk Behaviours Among Ugandan Gay and Bisexual Men. Int J STD&AIDS (2013) 24:409–13. 10.1177/0956462412472793
62
Dudley MG Rostosky SS Korfhage BA . Correlates of High-Risk Sexual Behavior Among Young Men Who Have Sex with Men. Educ Prev (2004) 16:328–40. 10.1521/aeap.16.4.328.40397
63
Yu B Yang S Huang Y Han J Dong P Liu M et al Correlation between Self-Identity and Multiple Sexual Partners of MSM Among Young Students. Chin J AIDS&STD (2020) 26:729–32.
64
Xu W Zheng L Xu Y Zheng Y . Internalized Homophobia, Mental Health, Sexual Behaviors, and Outness of Gay/bisexual Men from Southwest China. Int J Equity Health (2017) 16:36. 10.1186/s12939-017-0530-1
65
Mu H Li Y Liu L Na J Yu L Bi X et al Prevalence and Risk Factors for Lifetime Suicide Ideation, Plan and Attempt in Chinese Men Who Have Sex with Men. BMC Psychiatry (2016) 16:117. 10.1186/s12888-016-0830-9
66
Tang S Tang W Meyers K Chan P Chen Z Tucker JD . HIV Epidemiology and Responses Among Men Who Have Sex with Men and Transgender Individuals in China: a Scoping Review. BMC Infect Dis (2016) 16:588. 10.1186/s12879-016-1904-5
67
Stahlman S Grosso A Ketende S Sweitzer S Mothopeng T Taruberekera N et al Depression and Social Stigma Among MSM in Lesotho: Implications for HIV and Sexually Transmitted Infection Prevention AIDS Behav, 19 (2015). p. 1460–9. 10.1007/s10461-015-1094-y
68
Stahlman S Bechtold K Sweitzer S Mothopeng T Taruberekera N Nkonyana J et al Sexual Identity Stigma and Social Support Among Men Who Have Sex with Men in Lesotho: a Qualitative Analysis. Matters (2015) 23:127–35. 10.1016/j.rhm.2015.11.017
69
Wang Y Hu Z Peng K Xin Y Yang Y Drescher J . Discrimination against LGBT Populations in China. Lancet Public Health (2019) 4:e440–1. 10.1016/S2468-2667(19)30153-7
Summary
Keywords
social capital, men who have sex with men, internalized homophobia, condomless sex, mediation effect
Citation
Yu B, Feng C, Yang X, Wang Z, Zou H, Jia P and Yang S (2023) Roles of Social Capital in the Association Between Internalized Homophobia and Condomless Sex Among Men Who Have Sex With Men in Southwest China: A Four-Way Decomposition. Int J Public Health 68:1605202. doi: 10.3389/ijph.2023.1605202
Received
09 July 2022
Accepted
10 January 2023
Published
20 January 2023
Volume
68 - 2023
Edited by
Sonja Merten, Swiss Tropical and Public Health Institute (Swiss TPH), Switzerland
Reviewed by
Yu-Te Huang, The University of Hong Kong, Hong Kong SAR, China
Updates
Copyright
© 2023 Yu, Feng, Yang, Wang, Zou, Jia and Yang.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shujuan Yang, rekiny@126.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.