Abstract
Objectives: The main objective of this research was to investigate the Work-life balance (WLB), mental health, and quality of life and their associated factors among Healthcare Professionals (HCPs) in Sudan during the peak of the COVID-19 pandemic during 2021.
Methods: An observational cross-sectional web-based survey was conducted during August-December 2021 among a sample of 430 HCPs working in the hospitals of four Sudanese states. The study used the WHOQoLBREF scale, Work-Life Balance Scale, and General Anxiety Disorder (GAD-7).
Results: HCPs reporting a poor quality of life made up 33.5% (95% CI 29.1–38.0), while those reporting worse WLB made up 52.6% (95% CI 47.8–57.2). HCPs reporting moderate to severe anxiety symptoms accounted for 35.8% (95% CI 31.4–40.5). The Multiple Regression model indicated that an increase in the anxiety scores is associated with a decrease in Health-related Quality of Life (HRQoL) (β= 0.831, p < 0.05). Female HCPs exhibited 4.53-fold lower HRQoL scores than their male colleagues (p < 0.05).
Conclusion: Approximately one-third of the HCPs in Sudan reported low HRQoL and suffered from moderate to severe anxiety, while a large portion of them had an unequal work-life balance during COVID-19. Health policies addressing these factors are needed to improve the quality of health of HCPs.
Introduction
The timeline of COVID-19 indicated that the first case was identified in China in December 2019 before spreading to every corner of the Globe, causing the most unprecedented public health crisis in recent decades [1]. In Sudan, the first case was reported on the 13th of March 2020, and by May 2021 the infection curve showed approximately 33,104 confirmed cases, 2,349 deaths, and 26,795 recovered cases [2].
The COVID-19 pandemic has a significant burden on all aspects of life, not limited to population health. Its impact extended to economic slowdown, Gross Domestic Product (GDP) growth and people’s jobs and livelihoods. As a developing country, Sudan’s healthcare system is already flooded by structural problems and this situation has been aggravated by COVID-19 [3]. Sudan’s healthcare system is characterized by limited resources, and the available information showed that the overall government health expenditure is very low and the health sector is under-funded [4].
Healthcare Professions (HCPs) were at the heart of the storm of the COVID-19 pandemic, facing multiple challenges in treating patients with COVID-19: reducing the spread of infection and developing prevention strategies. Healthcare workers were more likely to contract SARS-CoV-2 compared to the general population. In addition, during the COVID-19 pandemic, in some countries, female healthcare workers reported higher rates of mental health problems and burnout compared to male healthcare workers [5]. Furthermore, female health workers have double the rate of COVID-19 infections compared to their male colleagues [6].
Work-life balance (WLB) is defined as a high level of role engagement in professional activities and personal commitments with minimal conflict between social roles in work and non-work-life. Normally, the term encompasses three dimensions: time balance, involvement balance, and satisfaction balance [7]. The concept also includes burnout prevention and stress management as the level of productivity is increasingly associated with time to relax and recharge [8]. Stress at work is the psychological and physical state that results when a person’s resources cannot adapt or cope with the pressures of the situation [9]. Poor work settings can be accompanied by unhealthy consequences, including marital conflicts, shortened life expectancy, and immune system impairment [10, 11]. Quality of life (QoL) is the person’s perception of his/her position in life in the context of the culture and value systems [12].
According to the World Health Organization (WHO), the perceived QoL is not only the absence of physical disease but extends to the evaluation of an individual’s psychological, social, and environmental conditions [13]. QoL is measured using eleven indicators: education, wealth, the environment, employment, physical and mental health, safety, recreation and rest time, social belonging, religious beliefs, security, and freedom [13]. Improving QoL reflects in the employees, organization, and consumers and leads to improving the quality of care, strengthening organizational commitment, and increasing productivity [13].
Recent studies on QoL documented the strong association between QoL and the mental health of HCPs during the COVID-19 pandemic [14–17]. HCPs are dealing with a large number of confirmed or suspected cases under massive psychological and physical stress [18–20]. Increasingly published reports postulated that mental health among HCPs was affected and the prevalence of depression and anxiety among HCPs during the COVID-19 pandemic was (37%) and (40%), respectively [21]. A study conducted in 34 Chinese hospitals measured the psychological reactions of healthcare workers and found high rates of sadness (50%), anxiety (42%), insomnia (34%), and distress (72%) [22]. Similarly, rates of depression, anxiety, and post-traumatic stress disorder (PTSD) in healthcare workers ranged from (8.90% to (50.45) %, (10.4%) to (44.6%), and (32%) to (71.5%), respectively, in a recent systematic review [23]. On the other hand, work-life balance is closely correlated with burnout and mental health [19, 20, 24]. Burnout of HCPs and reduction in quality of life is related to an increased number of medical errors [25]. Some studies have found that work-life balance is linked to negative outcomes such as anxiety, depression, and mental health issues [26, 27].
There is a significant amount of literature available on COVID-19 and its impact on Quality of Life, Mental Health, and Work-Life Balance. However, there are still some gaps in the research regarding the relationship between these three factors during COVID-19 among HCPs. Further, there is a scarcity of published reports on work-life balance, stress, and quality of life among healthcare workers in Sudan during the COVID-19 pandemic. Hence, the main objective of this research was to investigate the work-life balance, mental health, and quality of life and their associated factors among HCPs in Sudan.
Methods
Study Design, Population, and Place
An observational cross-sectional survey targeted the HCPs in Sudan hospitals. The target population includes all HCPs of different specialties and departments in the four selected States. Work settings included intensive care units, inpatient units, outpatient clinics, pharmacies, clinical labs, radiology, and nursing Departments. The main inclusion criteria were HCPs who were actively working in hospitals with COVID-19 wards, and working for at least three months in the study setting.
The Republic of Sudan comprises 18 states, is populated by 45.70 million people as of the 2022 population estimate, and occupies 1,886,068 square kilometers. In our study, we selected four states representing the whole country, namely, North Kordofan, Al-Qadarif, El Gazira, and Khartoum, for this research. These four states are situated in western, eastern, and central Sudan, with Khartoum serving as the capital. These states are geographically diverse and provide a fairly accurate representation of the country as a whole.
Sampling Procedures
For the purpose of this study, a sample of 440 HCPs were estimated. This number was determined using the standard formula for cross-sectional surveys (Lwanga, and Lemeshow, 1991) [28], which is the initial sample size n = [(z2 *p * 1-p)]/d2. The terms of the equation are as follows: n is the required sample size; p is the attribute studied; Z is the standardized variable that corresponds to a 95% level of confidence and d is the desired marginal error.
Since we are interested in three domains (Work life balance, mental health, and QoL) a value of (0.5) for p is reasonable because it gives the maximum possible sample size. Assigning 0.05 for the marginal error and z = 1.96, the initial sample size was 400 participants and accounting for 20% non-repose rate the final size was 480 HCPs.
The sampling design was three-stage cluster random sampling; each Sudanese state was regarded as an independent cluster. Stage one involved a random selection of four states out of 16 of the whole of Sudan. In stage two, we selected one governmental hospital and another private one. We used probability proportional to size sampling (PPS) to determine the number of participants in the selected health institution. In the last step, we used a snowball technique to select healthcare professionals (HCPs) from each institution. The questionnaire link was then distributed to these HCPs through social networks like Facebook, Instagram, LinkedIn, and WhatsApp in their respective hospitals.
Data Collection and Study Instruments
A web-based questionnaire was used for data collection. The data collection tool consists of four parts. The first is sociodemographic information (age, gender, marital status, occupation, job period, chronic disease, and Tobacco use). The second part is the Work-life Balance scale (eight items) for measuring work-life climate. The work-life climate scale asks, “During the past week, how often did this occur?” followed by phrases such as: skipped a meal, arrived home late from work, or had difficulty sleeping. The response scale for the work-life climate items ranges from: rarely or none of the time (less than 1 day); some or a little of the time (1–2 days); occasionally or a moderate amount of time (3–4 days); all of the time (5–7 days); and not applicable. Work settings with less frequent work-life climate difficulties (lower scores) have HCPs with healthier work-life-balance [20].
The third section is measured by the General Anxiety Disorder (GAD-7) questionnaire, a validated seven-item assessment (Spitzer, et al, 2006) [29]. The tool is designed to assess the patient’s health status during the previous 14 days. The items require four responses: not difficult at all, somewhat difficult, very difficult and extremely difficult. The total scale scores for the seven items range from 0 to 21 and are categorized as follows; 0–4: minimal anxiety; 5–9: mild anxiety; 10–14: moderate anxiety and 15–21: severe anxiety.
The final part of the instrument is the World Health Organization Quality of Life-BREF (WHQoL-BREF). It is a self-administered 26-item instrument categorized into four domains (physical, psychological, social, and environmental). Each instrument item is scored from 1 to 5 on a response scale. Higher total scores indicate higher QoL [13]. The instruments are available for scientific purposes without commercial use. A pilot study was conducted among 30 HCPs working in Khartoum Hospitals to test the questionnaire applicability and understanding before starting the actual research. The data from the pilot study were not included in the main study. The internal consistency was calculated and evaluated for the different measures and produced a satisfactory result. The final results of the internal consistency based on Cronbach’s alpha are presented in the results section.
Data Management and Statistical Analysis
The IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp software program was used for data analysis. Descriptive statistics based on simple tabulations, frequencies, and percentages were used. The normality of continuous variables was assessed using the Shapiro-Wilk test. Means with their standard deviation were calculated and used to describe the total scores of the four domains of QoL, the scores of WLB and GAD-7. Categorical variables were described as frequency and percentage. To assess the differences in the demographic, workplace, QoL, and Anxiety characteristics, we compared the means of continuous variables using the Student’s t-test and One Way ANOVA respectively. The differences in percentages of categorical variables between the two groups was assessed using the Chi-squared test/Fisher exact test. A Multiple Linear regression model was used to assess predictors of the overall score of quality of life among the healthcare Professions. The regression model analyzed the relationship between HRQoL (the dependent variable) and several independent variables including total Anxiety scores, WLB scores, tobacco use, history of workplace violence, and demographics such as age, gender, marital status, and profession. The regression model was assessed for Multicollinearity and other assumptions underlying OLS technique. The model was also assessed for Goodness of fit using an F test and the coefficient of multiple determination (R2.). A p. value of less than 0.05 was considered significant.
Ethical Consideration
This study was conducted according to the ethical standards of Sudan and the Helsinki declaration. The IRB committee of Al-Gadarif University approved the study protocol ref GU/FM/REC/Q3.7.12.4 dated July 2021. All the participants read, understood, and signed the study consent. The data was stored under a high confidentiality level without names to protect participants’ privacy.
Results
Of the 480 anticipated responses, a total of 430 HCPs were included in the analysis providing a response rate of 89.6%. The background characteristics of the HCPs are presented in Table1. Most participants were female (N = 276, 64.2%), single HCPs (N = 365, 84.9%), in the age group (25–34) years (N = 285, 66.3%) The majority of healthcare professionals were Physicians (N = 293, 68.1%). Most of them had less than 4 years of experience (N = 330, 76.7%) and were working Morning shifts (N = 249, 57.9%). One-fifth of HCPs reported verbal violence during the COVID-19 pandemic (N = 98, 22.8%) and only (N = 47, 10.9%) were Tobacco users.
TABLE 1
| Characteristic (N = 430) | Count | % | |
|---|---|---|---|
| Gender | Male | 154 | 35.8 |
| Female | 276 | 64.2 | |
| Marital status | Single | 365 | 84.9 |
| Married | 65 | 15.1 | |
| Age groups (years) | 18–24 | 123 | 28.6 |
| 25–34 | 285 | 66.3 | |
| 35–50 | 22 | 5.1 | |
| Profession | Physician | 293 | 68.1 |
| Nurse | 37 | 8.6 | |
| Pharmacist | 28 | 6.5 | |
| Technician | 22 | 5.1 | |
| Other profession | 50 | 11.6 | |
| Years of Experience | Less than 4 | 330 | 76.7 |
| 4–9 | 84 | 19.5 | |
| 10–20 | 16 | 3.7 | |
| Working Shifts | Morning | 249 | 57.9 |
| Evening | 84 | 19.5 | |
| Both | 97 | 22.6 | |
| Type of violence during COVID-19 | Verbal | 98 | 22.8 |
| Physical | 6 | 1.4 | |
| Intimidation | 16 | 3.7 | |
| None | 310 | 72.1 | |
| Tobacco use | Yes | 47 | 10.9 |
| No | 383 | 89.1 | |
Participants’ demographic and professional characteristics, (Sudan, 2021).
Table 2 summarizes the mean scores for the four domains of WHOQoL, WLB, and GAD-7 according to HCPs’ background characteristics. The WLB mean for the HCPs was [17 ± 5.3, 95% CI = 16.6–17.6], compared with [8 ± 5.2, 95% CI = 7.1–8.2] for the GAD-7 total score. The same Table showed a significant difference (p < 0.05) in mean scores for social relationship QoL domain according to the variable years of experiences. Moreover, there was a significant difference (p < 0.05) in mean scores according to age groups in the environment domain, GAD-7, and WLB. The type of violence mean scores also differ significantly (p < 0.05) across the four WHOQol domains, WLB and GAD-7. The mean scores according to Tobacco use were also significantly different for WLB and Physical QoL domain (p < 0.05).
TABLE 2
| Characteristic | WHOQoL Domainsa | WLBb | GADb | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Physical | Psychological | Social relationships | Environment | ||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| Gender | Male | 56 | (19.3) | 58 | (20.2) | 49 | (24.3) | 42 | (18.1) | 17 | (5.4) | 8 | (6.0) |
| Female | 52 | (19.6) | 55 | (18.8) | 47 | (22.5) | 41 | (16.6) | 17 | (5.2) | 8 | (5.4) | |
| Marital status | Single | 54 | (19.0) | 56 | (19.5) | 44c | (21.7) | 41 | (16.7) | 17c | (5.2) | 8 | (5.7) |
| Married | 51 | (22.4) | 56 | (19.1) | 66 | (22.5) | 42 | (19.4) | 19 | (5.7) | 8 | (5.6) | |
| Age groups (years) | 18–24 | 57 | (19.4) | 59 | (19.9) | 48 | (23.0) | 44d | (16.7) | 19d | (5.4) | 7d | (5.4) |
| 25–34 | 52 | (19.5) | 55 | (19.0) | 47 | (23.3) | 40 | (17.1) | 17 | (5.2) | 8 | (5.7) | |
| 35–50 | 52 | (20.1) | 56 | (20.3) | 51 | (22.8) | 41 | (18.4) | 16 | (4.6) | 8 | (5.2) | |
| Profession | Physician | 52d | (19.2) | 55d | (19.6) | 47 | (23.0) | 40 | (17.8) | 16d | (5.1) | 8 | (5.7) |
| Nurse | 63 | (18.6) | 68 | (18.9) | 53 | (22.2) | 46 | (18.7) | 19 | (5.9) | 6 | (4.4) | |
| Pharmacist | 51 | (18.3) | 57 | (18.3) | 52 | (25.5) | 40 | (14.2) | 20 | (4.8) | 7 | (3.7) | |
| Technician | 57 | (19.9) | 58 | (13.8) | 49 | (23.8) | 43 | (12.2) | 19 | (4.6) | 7 | (5.8) | |
| Other profession | 52 | (21.3) | 55 | (18.9) | 45 | (22.8) | 44 | (14.8) | 19 | (5.2) | 8 | (6.7) | |
| Years of Experience | Less than 4 | 54 | (18.9) | 57 | (18.6) | 47d | (22.3) | 41 | (16.3) | 17 | (5.4) | 8 | (5.6) |
| 4–9 | 51 | (21.4) | 55 | (22.1) | 52 | (27.0) | 43 | (19.8) | 17 | (5.2) | 8 | (5.9) | |
| 10–20 | 51 | (22.4) | 53 | (20.6) | 42 | (16.1) | 39 | (18.4) | 16 | (4.6) | 9 | (6.0) | |
| Working Shifts | Morning | 54 | (19.4) | 57 | (18.9) | 49 | (23.4) | 43 | (17.2) | 18d | (5.2) | 8 | (5.6) |
| Evening | 52 | (20.1) | 55 | (19.1) | 46 | (23.9) | 40 | (15.5) | 18 | (5.0) | 7 | (6.0) | |
| Both | 53 | (19.6) | 56 | (20.8) | 44 | (21.4) | 38 | (17.9) | 14 | (5.0) | 8 | (5.4) | |
| No | 56 | (19.6) | 58 | (18.8) | 50 | (22.9) | 44 | (16.8) | 18 | (5.3) | 7 | (5.5) | |
| Type of violence during COVID-19 | Verbal | 48d | (19.2) | 51d | (19.8) | 41d | (23.0) | 35d | (17.5) | 15d | (4.7) | 9d | (5.9) |
| Physical | 59 | (8.7) | 57 | (9.7) | 43 | (20.7) | 40 | (12.4) | 15 | (4.5) | 7 | (2.2) | |
| Intimidation | 44 | (14.3) | 47 | (21.2) | 41 | (21.7) | 35 | (12.3) | 14 | (3.9) | 12 | (5.8) | |
| None | 56 | (19.6) | 58 | (18.9) | 50 | (22.9) | 44 | (16.8) | 18 | (5.3) | 7 | (5.5) | |
| Tobacco use | Yes | 47c | (19.2) | 53 | (20.1) | 46 | (24.1) | 37 | (20.0) | 15c | (5.0) | 7 | (6.0) |
| No | 54 | (19.5) | 57 | (19.3) | 48 | (23.0) | 42 | (16.7) | 17 | (5.3) | 8 | (5.6) | |
| Healthcare professionals | 53 | 19.6 | 56 | (19.4) | 48 | (23.1) | 41 | (17.1) | 17 | (5.3) | 8 | (5.2) | |
| 95% CI | 51.5–55.2 | 54.4–58.0 | 45.4–49.7 | 39.5–42.8 | 16.6–17.6 | 7.1–8.2 | |||||||
| Cronbach’s alpha | 0.812 | 0.739 | 0.400 | 0.744 | 0.826 | 0.899 | |||||||
The Mean and SD scores of the health-related Quality of Life Domains, Work-life balance, and General Anxiety Disorder according to healthcare professionals background characteristics, (Sudan, 2021).
Abbreviations: HCP, Healthcare professionals; GAD, General Anxiety Disorder; WLB, work Life Balance; SD, Standard Deviation.
The max value for HRQoL Domains, WLB and GAD, were 100, 32 and 16 respectively.
Higher score is favorable.
Lower score is favorable.
Significant at the 0.05 level, based on the independent sample t-test.
Significant at the 0.05 level, based on One-way ANOVA test.
Marital status, profession, or occupation, working shifts, workplace violence, type of violence and Tobacco use, were positively associated worse WLB (p < 0.05 for all). Further, experiencing workplace Violence, and certain types of violence were also positively associated with moderate to severe anxiety among the study participants (p < 0.05 for all). There were more female than male respondents with poor quality of life as well as more pharmacists than other occupations reporting workplace violence, but without documenting a statistically significant association (p > 0.05 for all) (Table 3). As shown in the same Table, the proportion of HCPs with poor HRQoL was 33.5% (95% CI 29.1–38.0), while the percentage of those reporting worse WLB was 52.6% (95% CI 47.8–57.2). HCPs reporting symptoms of moderate to severe anxiety accounted for 35.8% (95% CI 31.4–40.5) of the study participants.
TABLE 3
| Characteristic | Poor QoL | p-value | Worse WLB | p-value | Moderate to severe anxiety | p-value | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| No | % | No | % | No | % | |||||
| Gender | Male | 48 | (31.2) | 0.580 | 76 | (49.4) | 0.990 | 54 | (35.1) | 0.059 |
| Female | 96 | (34.8) | 150 | (54.3) | 100 | (36.2) | ||||
| Marital status | Single | 123 | (33.7) | 0.827 | 181 | (49.6) | 0.003 | 126 | (34.5) | 0.185 |
| Married | 21 | (32.3) | 45 | (69.2) | 28 | (43.1) | ||||
| Age groups (years) | 18–24 | 33 | (26.8) | 0.160 | 73 | (59.3) | 0.186 | 34 | (27.6) | 0.081 |
| 25–34 | 102 | (35.8) | 143 | (50.2) | 111 | (38.9) | ||||
| 35–50 | 9 | (40.9) | 10 | (45.5) | 9 | (40.9) | ||||
| Profession | Physician | 100 | (34.1) | 0.477 | 134 | (45.7) | 0.001 | 112 | (38.2) | 0.251 |
| Nurse | 10 | (27.0) | 22 | (59.5) | 9 | (24.3) | ||||
| Pharmacist | 13 | (46.4) | 20 | (71.4) | 7 | (25.0) | ||||
| Technician | 6 | (27.3) | 15 | (68.2) | 6 | (27.3) | ||||
| Other profession | 15 | (30.0) | 35 | (70.0) | 20 | (40.0) | ||||
| Years of Experience | Less than 4 | 111 | (33.6) | 0.911 | 173 | (52.4) | 0.718 | 109 | (33.0) | 0.082 |
| 4–9 | 27 | (32.1) | 46 | (54.8) | 37 | (44.0) | ||||
| 10–20 | 6 | (37.5) | 7 | (43.8) | 8 | (50.0) | ||||
| Working Shifts | Morning | 82 | (32.9) | 0.654 | 151 | (60.6) | <0.001 | 93 | (37.3) | 0.928 |
| Evening | 26 | (31.0) | 48 | (57.1) | 28 | (33.3) | ||||
| Both | 36 | (37.1) | 27 | (27.8) | 33 | (34.0) | ||||
| Work place violence | Yes | 48 | (40.0) | 0.075 | 42 | (35.0) | <0.001 | 55 | (45.8) | 0.007 |
| No | 96 | (31.0) | 184 | (59.4) | 99 | (31.9) | ||||
| Type of violence during COVID-19* | Verbal | 40 | (40.8) | 0.271 | 33 | (33.7) | <0.001 | 42 | (42.9) | 0.006 |
| Physical | 1 | (16.7) | 2 | (33.3) | 1 | (16.7) | ||||
| Intimidation | 6 | (37.5) | 6 | (37.5) | 11 | (68.8) | ||||
| None | 97 | (31.3) | 185 | (59.7) | 100 | (32.3) | ||||
| Tobacco use | Yes | 21 | (44.7) | 0.085 | 14 | (29.8) | 0.001 | 14 | (29.8) | 0.361 |
| No | 123 | (32.1) | 212 | (55.4) | 140 | (36.6) | ||||
| All HCPs | 144 | (33.5) | 226 | (52.6) | 154 | (35.8) | ||||
| 95% CI | 29.1–38.0 | 47.8–57.2 | 31.4–40.5 | |||||||
Factors associated with poor Quality of life, worse Work-life balance, and moderate to severe Anxiety among healthcare professionals, (Sudan, 2021).
Abbreviations: HCPs, Healthcare professionals; WLB, work Life Balance.
The cutoff for Moderate to severe anxiety symptoms was >8, poor QoL <50 and worse WLB >16.
p-value was based on Chi squared test; *p-value is based on Fisher Exact test.
Figure 1 presents the work-life balance dimensions among the healthcare Professions. Most of the study participants (80%) reported a poorly balanced diet, while three quarters suffered sleep difficulty. Two-thirds (66%) of HCPs arrived home late from work, and 57% skipped a meal during COVID-19. HCPs who worked through a shift without any breaks accounted for over half (56%) of the respondents. Regarding the work-life environment, it was reported that 41% of HCPs felt frustrated by technology.
FIGURE 1
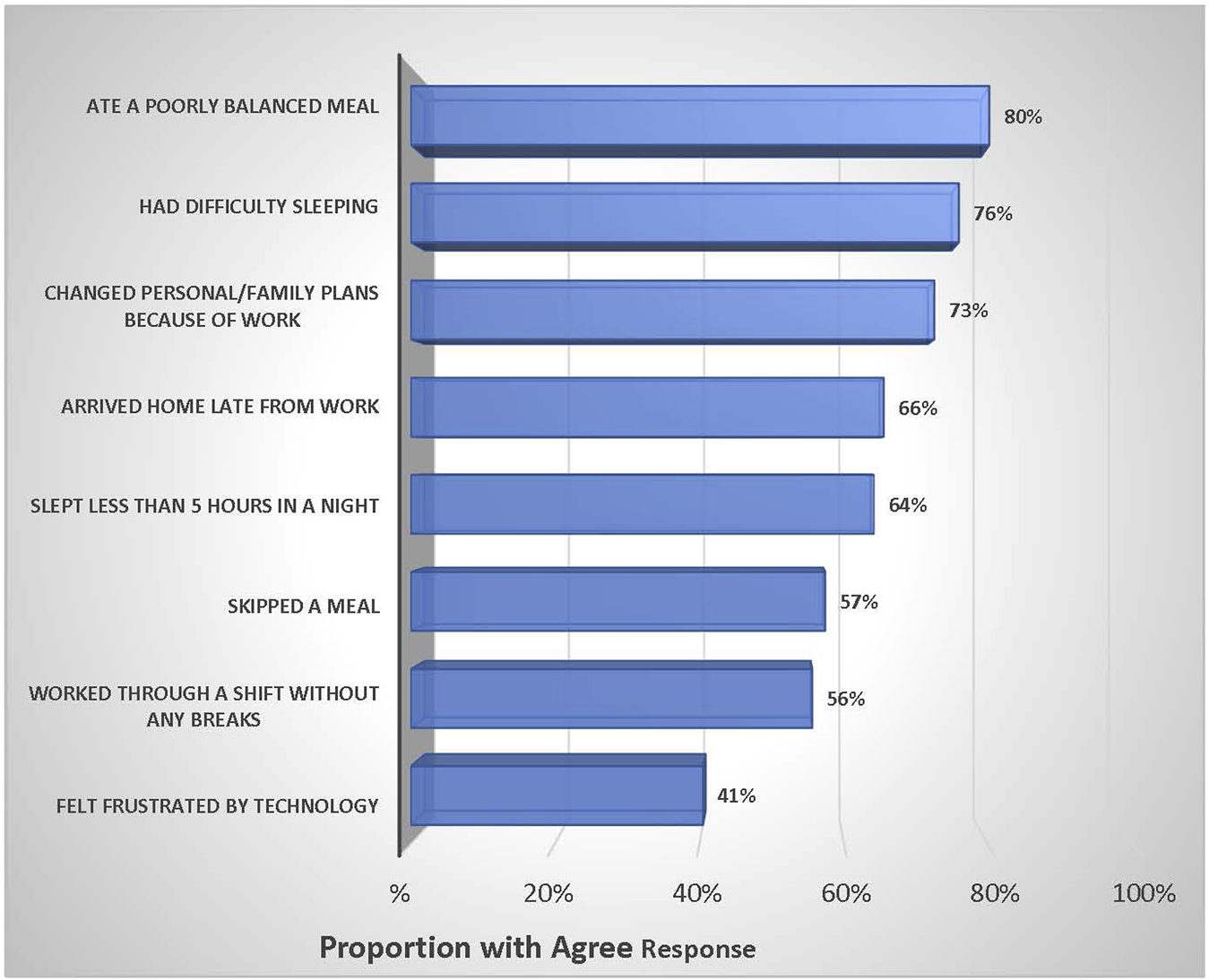
Work–life Balance dimensions among the healthcare professions, (Sudan, 2021).
Table 4 provides The Multiple Linear Regression model for the factors that predict the overall HRQoL scores among the HCPs. The model shows that WLB and (GAD-7) scores significantly predict the level of HRQoL (p < 0.001). The results indicate that an increase in the Anxiety scores (GAD-7) by one unit is associated with a decreased HRQoL (β= 0.831, p < 0.05). The table further indicated that other healthcare professionals exhibited lower HRQoL scores than the physicians (p < 0.05). Moreover, female HCPs also exhibited lower HRQoL scores than the males (p < 0.05). Married HCPs were associated with higher levels of HRQoL (β = 4.91, p < 0.05) compared with single HCPs. Non-smokers were associated with a higher level of HRQoL (β = 4.91, p < 0.05) than smokers.
TABLE 4
| Term | Coef | SE Coef | T-Value | p-value | VIF | Model summary |
|---|---|---|---|---|---|---|
| Constant | 54.70 | 9.02 | 6.07 | <0.001 | F = 13.8 p-value= <0.001 | |
| Total Anxiety Scores | −0.831 | 0.131 | −6.36 | <0.001 | 1.09 | |
| WLB Scores | −0.969 | 0.148 | 6.57 | <0.001 | 1.22 | |
| Age (years) | −0.627 | 0.337 | −1.86 | 0.063 | 3.46 | |
| Years of Experience | 0.525 | 0.411 | 1.28 | 0.202 | 3.19 | |
| Gender | ||||||
| Male | REF | |||||
| Female | −5.43 | 1.61 | −3.37 | 0.001 | 1.19 | |
| Marital Status | ||||||
| Single | REF | |||||
| Married | 4.53 | 2.19 | 2.07 | 0.039 | 1.23 | |
| Tobacco Use | ||||||
| Smokers | REF | R2 = 0.27 | ||||
| Non-Smokers | 4.91 | 2.44 | 2.02 | 0.045 | 1.16 | |
| Profession | ||||||
| Physician | REF | |||||
| Nurse | 4.28 | 2.72 | 1.57 | 0.117 | 1.16 | |
| Pharmacist | −5.02 | 3.04 | −1.65 | 0.099 | 1.13 | |
| Technician | −1.05 | 3.34 | −0.31 | 0.754 | 1.08 | |
| Other profession | −5.32 | 2.36 | −2.26 | 0.025 | 1.14 | |
| Work place violence | ||||||
| Yes | REF | |||||
| NO | 2.98 | 1.68 | 1.77 | 0.078 | 1.14 |
Multiple linear regression model for the factors that are associated with the health-related Quality of Life overall scores as a dependent variable, (Sudan, 2021).
Abbreviation: Coef, regression coefficient; SE Coef, standard error of the coefficient; ref, reference category; REF, reference category.
Discussion
This study tried to investigate the QoL, mental health, and work-life balance among Sudanese healthcare professionals during the COVID-19 Pandemic. To the best of our knowledge, this is the first national study to assess the experiences of HCPs in Sudan. The COVID-19 Pandemic was unprecedented and affected the healthcare systems in all countries. Healthcare workers were at the frontline of the storm and sacrificed their lives and welfare.
The results revealed moderate to severe anxiety among 35.8% of the study participants. This high level of anxiety among HCPs is consistent with some existing literature [30]. A recent study conducted in Khartoum state in Sudan revealed moderate to severe anxiety in 34.9% of respondents [31]. A wealth of research suggests that excessive work pressure is linked to mental disorders, anxiety, insomnia, distress, and fear of infection [32–34]. A systematic review and meta-analyses revealed that the overall prevalence of stress among HCPs reaches 45% [35]. The mean score of the psychological domain was almost 56, which indicates worse psychological health quality of life. These results indicated that a considerable percentage of HCPs suffered from mental health disorders. This finding is consistent with many published studies during COVID-19 [36–38]. Many factors contribute to the psychological health quality of life, including great pressure at work, life-saving decisions given limited knowledge about the new epidemic, limited resources, and fear of harming family and friends with COVID-19 infection.
The analysis revealed a poor work-life integration in more than half (60.2%) of the HCPs, who expressed dissatisfaction with work-life integration (WLI). This result is consistent with the Khartoum state study [31] and international research [39]. The epidemic created a negative social environment for HCPs including fear, anxiety, and concern for both patients and their loved ones [40]. Some suffered from low social acceptance and high workload that affected their work-family integration [33].
Healthcare professionals experience traumatic events during the COVID-19 pandemic, which make them prone to stress and anxiety. In contrast to many studies [41–43], this research did not document a significant difference in anxiety according to gender, as severe anxiety was documented among 35.1% of males and 36.2% of females. A similar study conducted in Brazil showed that anxiety was more prevalent among females, who were also more likely to develop depression, anxiety, and insomnia than male workers [41].
A large proportion of the study participants reported poor quality of life (33.5%). It is well documented that the healthcare environment is a major public health concern that affected the health of HCPs during COVID-19. A recent review conducted by Kandula and Wake, 2021 concluded that there is a greater impact on the QoL of health professions which is attributed to many issues such as disturbances in physical and mental health [14].
In this study, age and gender were found to be an important factor associated with HRQoL. We found that female HCPs exhibited lower HRQoL scores than their male counterparts. This finding is in line as a study in frontline Brazilian healthcare workers [41] which showed that anxiety was more prevalent among females. The explanation for that according to many systematic reviews reported a higher risk of female HCWs in developing depression, anxiety, and insomnia compared to male workers [5, 14].
One interesting finding was that other healthcare professionals exhibited lower HRQoL scores than the physicians. This finding disagrees with Chalhub, et al (2021), who found that physicians had lower HRQoL. Moreover, the HCPs who experience any type of violence have low HRQoL compared to those who do not [41]. Workplace violence is always associated with dissatisfaction and increased stress [3]. Like most literature, our research revealed the negative association between mental health and HRQoL. Health-related quality of life was worse among HCPs who experienced high stress [17].
Although this research is the first to deal with HCPs quality of life, mental health, and work-life-balance using a relatively representative sample from four states of Sudan, it has some limitations. First, we used a cross-sectional design, so the associations in this research should be interpreted carefully. Second, the self-reported data may affect the accuracy of the study outcomes; however, the level of education in our population and the high response rate may mitigate potential sampling bias. The study did not include important variables, such as direct contact with patients, previous infection of COVID-19, and extra work hours. Further studies are recommended on these issues. Finally, during the final stage of the sampling procedures, the research relied on non-random sampling, which ultimately had an impact on the reliability of the research outcomes.
In conclusion, one-third of the healthcare Professionals in Sudan reported poor Health-related Quality of life-based on the WHO scale during the COVID-19 pandemic. It is also documented that large segments of HCPs have an unequal life-work balance. At the same time, there is a strong association between mental health and HRQol. Health institutions must implement health intervention programs to address mental health concerns among HCPs and promote better-coping strategies in the workplace during pandemics. Further, at a macro level, there is an urgent need for a health policy to address these factors to improve the quality of health of the HCPs and hence improve the standard of patient care in Sudan.
Statements
Ethics statement
The studies involving human participants were reviewed and approved by Algadarif University—Ethical Committee approved this research- SUDAN. The patients/participants provided their written informed consent to participate in this study.
Author contributions
MM, SO, BM, ES, MI, RE, and MO contributed in the study conception and design, data collection, analysis and interpretation of results, draft manuscript preparation, reviewed the results and approved the final version of the manuscript.
Acknowledgments
We thank all the study participants who gave their valuable time, actively participated, and completed the questionnaire.
Conflict of interest
The authors declare that they do not have any conflicts of interest.
Abbreviations
HCPs, Healthcare professionals; WLI, work-life integration; WLB, Work-life balance; GAD, General Anxiety Disorder; WHQoL-BREF, Health Organization Quality of Life-BREF; QoL, Quality of Life; HRQoL, Health related Quality of Life.
References
1.
Wang C Horby PW Hayden FG Gao GF . A Novel Coronavirus Outbreak of Global Health Concern. The Lancet (2020) 395(10223):470–3. 10.1016/S0140-6736(20)30185-9
2.
COVID-19—Sudan. WHO Coronavirus (COVID-19) Dashboard (2022). Available from: https://covid19.who.int/region/emro/country/sd (Accessed May 19;16:2022).
3.
El-Sadig SM Fahal LA Abdelrahim ZB Ahmed ES Mohamed NS Siddig EE . Impact of COVID-19 on Doctors and Healthcare Providers During the Pandemic in Sudan. Trans R Soc Trop Med Hyg (2021) 115:577–8. 10.1093/trstmh/trab016
4.
Ebrahim EM Ghebrehiwot L Abdalgfar T Juni MH . Health Care System in Sudan: Review and Analysis of Strength, Weakness, Opportunity, and Threats (SWOT Analysis). Sudan J Med Sci (2017) 12(3):133–50. 10.18502/sjms.v12i3.924
5.
Shaukat N Ali DM Razzak J . Physical and Mental Health Impacts of COVID-19 on Healthcare Workers: A Scoping Review. Int J Emerg Med (2020) 13(1):40. 10.1186/s12245-020-00299-5
6.
COVID-19: Emerging gender data and why it matters. UN Women Data Hub (2022). Available from: https://data.unwomen.org/resources/covid-19-emerging-gender-data-and-why-it-matters (Accessed June 12, 2022).
7.
Sirgy MJ Lee DJ . Work-Life Balance: An Integrative Review. Appl Res Qual Life (2018) 13(1):229–54. 10.1007/s11482-017-9509-8
8.
Meenakshi SP The Importance of Work-Life-Balance. IOSR J Bus Manag (2013) 14(3):31–5. 10.9790/487x-1433135
9.
Michie S . Causes and Management of Stress at Work. Occup Environ Med (2002) 59(1):67–72. 10.1136/oem.59.1.67
10.
Schwartz SP Adair KC Bae J Rehder KJ Shanafelt TD Profit J et al Work-Life Balance Behaviours Cluster in Work Settings and Relate to Burnout and Safety Culture: A Cross-Sectional Survey Analysis. BMJ Qual Saf (2019) 28(2):142–50. 10.1136/bmjqs-2018-007933
11.
Shanafelt TD Boone SL Dyrbye LN Oreskovich MR Tan L West CP et al The Medical Marriage: A National Survey of the Spouses/partners of US Physicians. Mayo Clin Proc [Internet] (2013) 88(3):216–25. 10.1016/j.mayocp.2012.11.021
12.
WHOQOL. Measuring Quality of Life, the World Health Organization (2023). Available from: https://www.who.int/toolkits/whoqol (Accessed January 10, 2023).
13.
World Health Organization. WHOQOL-BREFF Introduction, Adminstration, Scoring and Generic Version of the Assessement Feild Trail Version December 1996. Programme on Mental Health. Geneva, Switzerland: World Health Organization (1996).
14.
Kandula UR Wake AD . Assessment of Quality of Life Among Health Professionals During COVID-19: Review. J multidisciplinary Healthc (2021) 14:3571–85. 10.2147/JMDH.S344055
15.
Iqbal MS . Predictors of Health-Related Quality of Life Among Healthcare Professionals. Med Sci (2020) 24(4445):e52.
16.
Tran TV Nguyen HC Pham LV Nguyen MH Nguyen HC Ha TH et al Impacts and Interactions of COVID-19 Response Involvement, Health-Related Behaviours, Health Literacy on Anxiety, Depression and Health-Related Quality of Life Among Healthcare Workers: A Cross-Sectional Study. BMJ Open (2020) 10(12):e041394. 10.1136/bmjopen-2020-041394
17.
Korkmaz S Kazgan A Çekiç S Tartar AS Balcı HN Atmaca M . The Anxiety Levels, Quality of Sleep and Life and Problem-Solving Skills in Healthcare Workers Employed in COVID-19 Services. J Clin Neurosci (2020) 80:131–6. 10.1016/j.jocn.2020.07.073
18.
Gupta N Dhamija S Patil J Chaudhari B . Impact of COVID-19 Pandemic on Healthcare Workers. Ind Psychiatry J (2021) 30(1):S282–S284. 10.4103/0972-6748.328830
19.
Fiorillo A Gorwood P . The Consequences of the COVID-19 Pandemic on Mental Health and Implications for Clinical Practice. Eur Psychiatry (2020) 63(1):e32. 10.1192/j.eurpsy.2020.35
20.
Ornell F Halpern SC Kessler FH Narvaez JC . The Impact of the COVID-19 Pandemic on the Mental Health of Healthcare Professionals. Cadernos de saude publica (2020) 36:e00063520. 10.1590/0102-311x00063520
21.
Saragih ID Tonapa SI Saragih IS Advani S Batubara SO Suarilah I et al Global Prevalence of Mental Health Problems Among Healthcare Workers During the Covid-19 Pandemic: A Systematic Review and Meta-Analysis. Int J Nurs Stud (2021) 121:104002. 10.1016/j.ijnurstu.2021.104002
22.
Lai J Ma S Wang Y Cai Z Hu J Wei N et al Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open (2020) 3(3):e203976. 10.1001/jamanetworkopen.2020.3976
23.
Robertson LJ Maposa I Somaroo H Johnson O . Mental Health of Healthcare Workers During the COVID-19 Outbreak: A Rapid Scoping Review to Inform Provincial Guidelines in South Africa. S Afr Med J (2020) 110(10):1010–9. 10.7196/samj.2020.v110i10.15022
24.
Shanafelt TD West CP Sinsky C Trockel M Tutty M Satele DV et al Changes in Burnout and Satisfaction With Work-Life Integration in Physicians and the General US Working Population Between 2011 and 2017. Mayo Clin Proc (2019) 94(9):1681–94. 10.1016/j.mayocp.2018.10.023
25.
Shanafelt TD Balch CM Bechamps G Russell T Dyrbye L Satele D et al Burnout and Medical Errors Among American Surgeons. Ann Surg (2010) 251(6):995–1000. 10.1097/SLA.0b013e3181bfdab3
26.
Kotera Y Green P Sheffield D . Work-Life Balance of UK Construction Workers: Relationship With Mental Health. Constr Manag Econ (2020) 38(3):291–303. 10.1080/01446193.2019.1625417
27.
Borowiec AA Drygas W . Work-Life Balance and Mental and Physical Health Among Warsaw Specialists, Managers and Entrepreneurs. Int J Environ Res Public Health (2022) 20(1):492. 10.3390/ijerph20010492
28.
Lwanga SK Lemeshow S . Sample Size Determination in Health Studies a Practical Manual. Geneva, Switzerland: World Health Organization (2022).
29.
Spitzer RL Kroenke K Williams JB Löwe B A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch Intern Med (2006) 166(10):1092–7. 10.1001/archinte.166.10.1092
30.
Kang L Ma S Chen M Yang J Wang Y Li R et al Impact on Mental Health and Perceptions of Psychological Care Among Medical and Nursing Staff in Wuhan During the 2019 Novel Coronavirus Disease Outbreak: A Cross-Sectional Study. Brain Behav Immun (2020) 87:11–7. 10.1016/j.bbi.2020.03.028
31.
Mahgoub IM Abdelrahman A Abdallah TA Mohamed Ahmed KA Omer ME Abdelrahman E et al Psychological Effects of the COVID‐19 Pandemic: Perceived Stress, Anxiety, Work–Family Imbalance, and Coping Strategies Among Healthcare Professionals in Khartoum State Hospitals, Sudan, 2021. Brain Behav (2021) 11(8):e2318. 10.1002/brb3.2318
32.
Razu SR Yasmin T Arif TB Islam M Islam SM Gesesew HA et al Challenges Faced by Healthcare Professionals During the COVID-19 Pandemic: A Qualitative Inquiry From Bangladesh. Front Public Health (2021) 9:647315. 10.3389/fpubh.2021.647315
33.
Paiano M Jaques AE Nacamura PA Salci MA Radovanovic CA Carreira L . Mental Health of Healthcare Professionals in China During the New Coronavirus Pandemic: An Integrative Review. Revista Brasileira de Enfermagem (2020) 18:73. 10.1590/0034-7167-2020-0338
34.
Perlis RH . Exercising Heart and Head in Managing Coronavirus Disease 2019 in Wuhan. JAMA Netw Open (2020) 3(3):e204006. 10.1001/jamanetworkopen.2020.4006
35.
Salari N Khazaie H Hosseinian-Far A Khaledi-Paveh B Kazeminia M Mohammadi M et al The Prevalence of Stress, Anxiety and Depression Within Front-Line Healthcare Workers Caring for COVID-19 Patients: A Systematic Review and Meta-Regression. Hum Resour Health (2020) 18(1):100–4. 10.1186/s12960-020-00544-1
36.
Young KP Kolcz DL O’Sullivan DM Ferrand J Fried J Robinson K . Health Care Workers’ Mental Health and Quality of Life During COVID-19: Results From a Mid-Pandemic, National Survey. Psychiatr Serv (2021) 72(2):122–8. 10.1176/appi.ps.202000424
37.
Stojanov J Malobabic M Stanojevic G Stevic M Milosevic V Stojanov A . Quality of Sleep and Health-Related Quality of Life Among Health Care Professionals Treating Patients With Coronavirus Disease-19. Int J Soc Psychiatry (2021) 67(2):175–81. 10.1177/0020764020942800
38.
Tomar BS Suman S Singh P Raj P Nathiya D . Mental Health Outcome and Professional Quality of Life Among Healthcare Workers During COVID-19 Pandemic: A Frontline-COVID Survey. Hamdan Med J (2020) 13(4):196. 10.4103/HMJ.HMJ_53_20
39.
Sharma T . Work Life Balance in COVID Time. J Perioper Crit Intensive Care Nurs S (2020) 1:1–3.
40.
Sun N Wei L Shi S Jiao D Song R Ma L et al A Qualitative Study on the Psychological Experience of Caregivers of COVID-19 Patients. Am J Infect Control (2020) 48(6):592–8. 10.1016/j.ajic.2020.03.018
41.
Chalhub RÁ Menezes MS Aguiar CV Santos-Lins LS Martins Netto E Brites C et al Anxiety, Health-Related Quality of Life, and Symptoms of Burnout in Frontline Physicians During the COVID-19 Pandemic. Braz J Infect Dis (2021) 25:101618. 10.1016/j.bjid.2021.101618
42.
Van Wert MJ Gandhi S Gupta I Singh A Eid SM Haroon Burhanullah M et al Healthcare Worker Mental Health After the Initial Peak of the COVID-19 Pandemic: A US Medical Center Cross-Sectional Survey. J Gen Intern Med (2022) 37:1169–76. 10.1007/s11606-021-07251-0
43.
Syamlan AT Salamah S Alkaff FF Prayudi YE Kamil M Irzaldy A et al Mental Health and Health-Related Quality of Life Among Healthcare Workers in Indonesia During the COVID-19 Pandemic: A Cross-Sectional Study. BMJ open (2022) 12(4):e057963. 10.1136/bmjopen-2021-057963
Summary
Keywords
HRQOL, general anxiety disorder, healthcare professions, work life balance, Sudan
Citation
Mahfouz MS, Osman SA, Mohamed BA, Saeed EAM, Ismaeil MIH, Elkhider RAA and Orsud MA (2023) Healthcare Professionals’ Experiences During the COVID-19 Pandemic in Sudan: A Cross-Sectional Survey Assessing Quality of Life, Mental Health, and Work-Life-Balance. Int J Public Health 68:1605991. doi: 10.3389/ijph.2023.1605991
Received
17 March 2023
Accepted
26 June 2023
Published
30 August 2023
Volume
68 - 2023
Edited by
Gabriel Gulis, University of Southern Denmark, Denmark
Reviewed by
Juan Gómez-Salgado, University of Huelva, Spain
Updates
Copyright
© 2023 Mahfouz, Osman, Mohamed, Saeed, Ismaeil, Elkhider and Orsud.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohamed Salih Mahfouz, mm.mahfouz@gmail.com, orcid.org/0000-0002-3155-6381
This Original Article is part of the IJPH Special Issue “Public Health and Primary Care, is 1 + 1 = 1?”
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.