Abstract
Objectives: Analyze the presence of acute stress response after adverse events in human talent in Colombian health institutions from 2017 to 2021.
Methods: Cross-sectional study of prevalence, carried out on 838 members of the human talent in health (professionals, technicians, technologists, and auxiliaries) of Colombian health institutions in the study period with the application of the EASE instrument. Univariate analysis using descriptive statistical techniques, chi-square and Student’s t-test, and bivariate analysis with a Poisson regression model using the institucional SPSS v. 26.
Results: The prevalence of adverse events in the last 5 years was 33.8%, presenting levels of acute stress qualifying as Medium-high emotional overload at 21.91%, while extreme acute stress was at 3.53%. The prevalence of risk for presenting acute stress after being involved in an adverse event was PR: 1.30 (CI: 1.24–1.36).
Conclusion: Acute stress in human talent after adverse events is limiting health and care capacity and must be efficiently addressed by health institutions. Psychosocial risk is linked within the framework of the patient safety program and the institutional occupational health and safety management systems.
Introduction
Patient safety is understood as the process by which the probability of harm to the patient during healthcare is sought to be reduced to a minimum acceptable level [1]; in this sense, in the Study of Prevalence of Adverse Effects in Latin American Hospitals (IBEAS) found a prevalence of 10% [2], and Ambulatory Care (AC) Services Across Latin America (LA) and the Caribbean (LAC) (AMBEAS/OPS) reported an adverse event prevalence of 5.2% [3, 4].
This is how the presentation of safety events related to healthcare unfolds: a patient suffers unpredictable and involuntary harm and requires support both physical and psychological; members of the human talent in health involved in the genesis of the event suffer negative impacts at a psychosocial, emotional, legal and professional level [5–9], and are designated second victims in a reputational crisis in the institution where the event occurred [10].
Therefore, among the negative impacts experienced by the second victim acute stress is one of the predominant symptoms that interferes with the proper performance of the professional and threatens the safety of patients [6, 11–13]. It is understood as a disorder related to a traumatic event such as patient safety events, which are related to direct contact with the event, which causes physical, psychological, and emotional effects [14]. Accordingly, psychosocial factors are understood as all those interactions that occur daily through work dynamics and in the work environment, and are present in all work environments regardless of the sector. In the health sector, the prevalence of acute stress due to exposure to psychosocial risk factors, after an adverse event, manifests itself as one of the conditions that produce the greatest impact on the health of health personnel, requiring effective intervention [6, 15–20].
However, health personnel worldwide during the period of this study also had to experience the effects on their mental health during the COVID-19 pandemic in the period from 2020 to 2021, where they were exposed to increased psychosocial strain and even greater probability of presentation of adverse events given the increase in patients and absenteeism of health personnel due to illness, among other causes, which materialized in disorders such as anxiety, depression, and acute stress as a consequence of work overload, repetitive exposure to traumatic events, and increased risk of contagion to them and/or their support network; this added to the stress resulting from the generation of adverse events, which is an aspect that must be taken into account in the study [21–24].
Due to the above, the present study aimed to analyze the presence of acute stress and presentation of the adverse event in human talent in Colombian health institutions in the period from 2017 to 2021.
Methods
A cross-sectional study of healthcare providers in Colombia from 2017 to 2021 in 838 human talent in health (auxiliaries, technicians, technologists, and professionals) in health institutions in three Colombian regions (Caribbean, Andean, and Pacific) [25]. The study had the signing of informed consent and the approval of the Ethics Committee of the Fundación Universitaria del Área Andina, Fundación Universitaria Sanitas, and the Red Salud Colsubsidio. Participation was voluntary, and participants could stop participating at any time. The confidentiality of personal data was guaranteed.
Instruments
The Acute Stress Scale (EASE) instrument was used and validated previously with a sample of health workers in Spain in primary care and hospitals [26, 27]. It was also employed in a study of four Latin American countries [20] (Table 1).
TABLE 1
| Scale questions |
|---|
| Factor 1- affective responses |
| I keep my distance, resent dealing with people, and am irascible even at home |
| I have completely lost the taste for things that used to bring me peace of mind or wellbeing |
| I feel that I am neglecting many people who need my help |
| I cannot help but think of recent critical situations. I cannot get out of work |
| I have difficulty thinking and making decisions, have doubts, and have entered a kind of emotional blockage |
| Factor 2- fear and anxiety responses |
| I have difficulty empathizing with patients ‘suffering or connecting with their situation (emotional distancing and emotional anesthesia) |
| Worrying about not getting sick causes me a strain that is hard to bear |
| I am afraid I am going to infect my family |
| I feel on permanent alert. I believe my reactions now put other patients, colleagues, or myself at risk |
| I feel intense physiological reactions (shock, sweating, dizziness, shortness of breath, insomnia, etc.) related to the current crisis |
| Total (score ranges from 3 to 30) | Individual scores range from 0 to 3 (0 = it did not happen to me; 1 = It occurs to me on specific occasions; 2 = I happen often; 3 = I was like this continuously |
Stress scale used among professionals caring Colombia 2017–2021.
Notes: Interpretability on the following categories based on score ranges were established: 0–9 points, good emotional adjustment; 10–14 points, emotional distress; 15–24 points, medium-high emotional overload; and ≥25 points, extreme acute stress.
The EASE scale was created to assess the possible acute stress from COVID-19 experienced during the COVID-19 pandemic in health sector personnel. The scale is self-applied through an application and has ten elements with four alternative responses each (Table 1).
The score scale ranges from 0 to 30 points and is structured into two factors; factor 1 refers to the emotional response, and factor 2 relates to the fears and anxiety experienced during the COVID-19 pandemic. The interpretability of the score is prioritized into four categories, good emotional adjustment (0–9 points), emotional distress (10–14 points), high emotional distress (15–24 points), and acute stress (>25 points).
In addition to the application of the instrument, a series of sociodemographic and work questions were included, in which the question “if he has been involved in an adverse event in the last 5 years” [sic] was included.
The sampling used was non-probabilistic sampling at convenience and was sent to the participants from different health institutions in the Andean, Pacific, and Caribbean regions through a Google form that contained the informed consent, a sociodemographic section, and variables of the work and the EASE instrument that was completed anonymously by the participants. The sample corresponds to health workers in health institutions of any level of complexity in the Andean, Caribbean, and Pacific regions. According to data from the National Policy of Human Talent in Health, in 2018 there were 599,890 health professionals; Casal’s [28] formula for infinite samples was employed, with a confidence level = 95%, a margin of error of 5%, meaning n = 384 to have a representative sample, and with the calculation of the non-response rate of 20%, the n = 461 participants, however, the answers received massively exceeded the calculated sample, with 834 health workers completing the questionnaire across three regions.
Reliability
The scale was minimally adapted, with only a few words being changed to better encompass the Colombian study population. The metric attributes of the scale were evaluated using Cronbach’s and McDonald’s Omega Alpha coefficients; a value greater than .85 was considered acceptable for this analysis.
Internal consistency values were tested and considered as adequate >7 (Cronbach α = .874 and McDonald ω = .877); when all items of the EASE scale were considered.
Statistical Analysis
A univariate analysis was fit considering the variables of interest—sex, marital status, educational level, working in more than one place, type of institution, and level of care indicate their percentage and size in the sample (Table 2).
TABLE 2
| Variable | Adverse event (2017–2021) | p-value | |||
|---|---|---|---|---|---|
| No (n = 555) | Yes (n = 283) | ||||
| n | % | n | % | ||
| Sex | 0.844 | ||||
| Man | 115 | 20.7 | 57 | 20.1 | |
| Women | 440 | 79.3 | 226 | 79.9 | |
| Civil Status | 0.690 | ||||
| Married | 174 | 31.4 | 103 | 36.4 | |
| Divorced | 23 | 4.1 | 12 | 4.2 | |
| Single | 225 | 40.5 | 109 | 38.5 | |
| Free union | 128 | 23.1 | 59 | 20.8 | |
| Widow (er) | 5 | 0.9 | 0.0 | ||
| Education level | 0.064 | ||||
| Baccalaureate | 5 | 0.9 | 1 | 0.4 | |
| Postgraduate | 159 | 28.6 | 97 | 34.3 | |
| Undergraduate | 156 | 28.1 | 90 | 31.8 | |
| Technological or Technical | 235 | 42.3 | 95 | 33.6 | |
| Age in years | 555 | 37.6* | 283 | 37.8* | 0.680 |
| Seniority in the position | 555 | 10.7* | 283 | 7.3* | 0.067 |
| Years of experience in the health sector | 555 | 13.1* | 283 | 13.3* | 0.068 |
| Work in another institution | 0.445 | ||||
| No | 444 | 80.0 | 220 | 77.7 | |
| Yes | 111 | 20.0 | 63 | 22.3 | |
| Type of institution where you work | 0.491 | ||||
| Mixed | 19 | 3.4 | 8 | 28 | |
| Private | 375 | 67.6 | 182 | 64.3 | |
| Public | 161 | 29.0 | 93 | 32.9 | |
| Level of complexity of the institution | 0.394 | ||||
| First level | 142 | 25.0 | 66 | 23.3 | |
| Second level | 124 | 22.0 | 69 | 24.4 | |
| Third level | 139 | 25.0 | 60 | 21.2 | |
| Fourth level | 150 | 27.0 | 88 | 31.1 | |
| Occupation | 0.181 | ||||
| Professional nursing | 123 | 22.0 | 78 | 28.0 | |
| Nursing assistant | 204 | 37.0 | 84 | 30.0 | |
| General practitioner doctor | 62 | 11.0 | 39 | 14.0 | |
| Specialist doctor | 77 | 14.0 | 36 | 13.0 | |
| Others | 89 | 16.0 | 46 | 15.0 | |
| Service | 0.014** | ||||
| Pediatric and adult emergencies | 138 | 24.9 | 57 | 20.1 | |
| Hospitalization of various specialties (adults and pediatrics) | 60 | 10.8 | 30 | 10.6 | |
| Gynecology and Obstetrics | 21 | 3.8 | 7 | 2.5 | |
| Surgery | 53 | 9.5 | 54 | 19.1 | |
| Adult and pediatric intensive care unit | 96 | 17.3 | 56 | 19.8 | |
| External consultation | 71 | 12.8 | 33 | 11.7 | |
| Home care | 9 | 1.6 | 4 | 1.4 | |
| Pediatrics and neonatology | 15 | 2.7 | 7 | 2.5 | |
| Other services | 92 | 16.6 | 35 | 12.4 | |
Characteristics sociodemographic and specific work of the sample (N = 838) in health institutions of three Colombian regions from 2017 to 2021.
Notes: * Average for quantitative variables and percentage for qualitative variables. p-value with calculated test and Chi-squared. **p-value <0.05, *p-value <0.01.
Subsequently, a bivariate analysis was carried out between the same variables of interest and the acute stress scale in its four levels (good emotional adjustment, emotional distress, medium-high emotional overload, and extreme acute stress), using the Fisher’s exact test to have percentages of each category and to evaluate the possible statistical relationship (p-value <0.05) (Table 3).
TABLE 3
| Variable | Estress acute level | |||||
|---|---|---|---|---|---|---|
| n | Good emotional adjustment | Emotional distress | Medium-high emotional overload | Extreme acute stress | p-value | |
| 838 | n = 520 | n = 168 | n = 135 | n = 15 | ||
| Sex | 0.242 | |||||
| Men | 172 | 22.7 | 18.5 | 15.6 | 13.3 | |
| Women | 666 | 77.3 | 81.6 | 84.4 | 86.7 | |
| Marital status | 0.648 | |||||
| Single | 334 | 41.5 | 38.1 | 37.0 | 26.7 | |
| Married or free union | 464 | 54.2 | 56.6 | 56.3 | 73.3 | |
| Divorced or widowed | 40 | 4.2 | 5.4 | 6.7 | 0.0 | |
| Education level | 0.135 | |||||
| High school | 6 | 0.8 | 1.2 | 0.0 | 0.0 | |
| Postgraduate | 256 | 31.0 | 33.9 | 27.4 | 6.7 | |
| Undergraduate | 246 | 29.0 | 32.1 | 28.2 | 20.0 | |
| Technological or Technical | 330 | 39.2 | 32.7 | 44.4 | 73.3 | |
| Working in more than one place | 0.083 | |||||
| No | 664 | 79.2 | 81.6 | 74.1 | 100.0 | |
| Yes | 174 | 20.8 | 18.5 | 25.9 | 0.0 | |
| Institution type | 0.125 | |||||
| Mixed | 27 | 4.2 | 2.4 | 0.7 | 0.0 | |
| Private | 557 | 66.5 | 61.9 | 69.6 | 86.7 | |
| Public | 254 | 29.2 | 35.7 | 29.6 | 13.3 | |
| Level of attention | 0.001* | |||||
| First level | 208 | 27.5 | 22.0 | 20.0 | 6.7 | |
| Second level | 193 | 22.1 | 28.0 | 22.2 | 6.7 | |
| Third level | 199 | 25.8 | 22.6 | 20.0 | 0.0 | |
| Fourth level | 235 | 24.6 | 27.4 | 37.8 | 86.7 | |
| Occupation | ||||||
| Nursing assistant | 208 | 34.2 | 28.6 | 37.8 | 73.3 | 0.022** |
| Nurse | 201 | 23.1 | 24.4 | 28.9 | 6.7 | |
| Medical general practitioner | 113 | 12.9 | 14.3 | 14.1 | 20.0 | |
| Medical specialist | 101 | 13.5 | 12.5 | 7.4 | 0.0 | |
| Other | 135 | 16.4 | 20.2 | 11.9 | 0.0 | |
| Involved in adverse event | ||||||
| No | 555 | 78.3 | 61.9 | 54.1 | 33.3 | 0.001* |
| Yes | 283 | 28.2 | 38.1 | 45.6 | 66.7 | |
Bivariate analysis between the sample’s main variables (%) and the four stress levels of the Self-applied Acute Stress Scale (EASE) Colombia 2017–2021.
Notes: **p-value <0.05, *p-value <0.01.
Regression Analysis
A multiple regression analysis (Poisson) was performed between the stress score and the variables of interest already mentioned, generating prevalence ratios, confidence intervals, statistically significant p-values, and the overall model p-value. Variables with high collinearity were not included in the model.
The Variance Inflation Factors test (VIF mean) test was performed to evaluate possible collinearity between the model variables, considering a score of <2.5 as low multicollinearity.
Results
Characteristics of Sociodemographic and Specific Work of the Sample in Colombia From 2017 to 2021
A total of 838 health workers responded by applying all EASY scale items. As early results, we can mention that almost 80% were women, 34% were nursing assistants, and nearly 40% were married, and with a technical career as training, approximately 20% worked in more than one institution at the same time (Table 2). It was found that 66.4% work in private institutions and 30.3% in public institutions, and 28.4% in fourth-level institutions. Also reported was an average work experience of 13 years in the field, ranging from 7 to 47 (Table 2).
Levels of the Self-Applied Acute Stress Scale
The bivariate analysis shows that extreme stress was reported more in women (86.7%), married or in a free union (73.3%), with technological or technical training (73.3%), working in private institutions (86.7%), at the fourth level of care (86.7%; p-value <0.01). A small number (3.53%; p-value < 0.01) were involved in an adverse event with a patient in the last 5 years, and the majority were nursing assistants (73.3%; p-value < 0.01) (Table 3).
More detail in Figure 1 shows that the individuals with better emotional adjustment reported working in first- and third-level institutions. Those with worse emotional ajdustment reported having experienced extreme acute stress levels, and working in institutions of level 1.
FIGURE 1
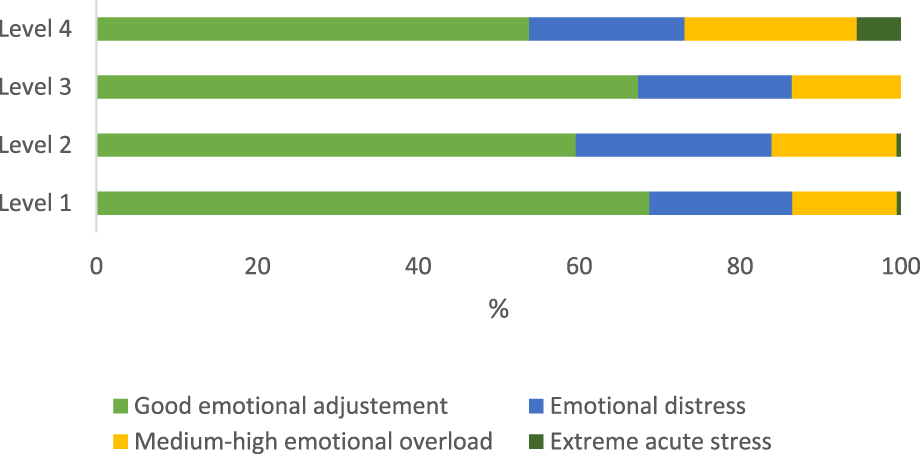
Percentage of emotional acute according to the level of attention of the working environment in Colombia from 2017 to 2021.
Figure 2 shows the level of stress by occupation or position. Medical specialists reported higher percentages of good emotional adjustment and less stress, general practitioners and nursing assistants reported a higher percentage of having experienced extreme stress in Colombia from 2017 to 2021.
FIGURE 2
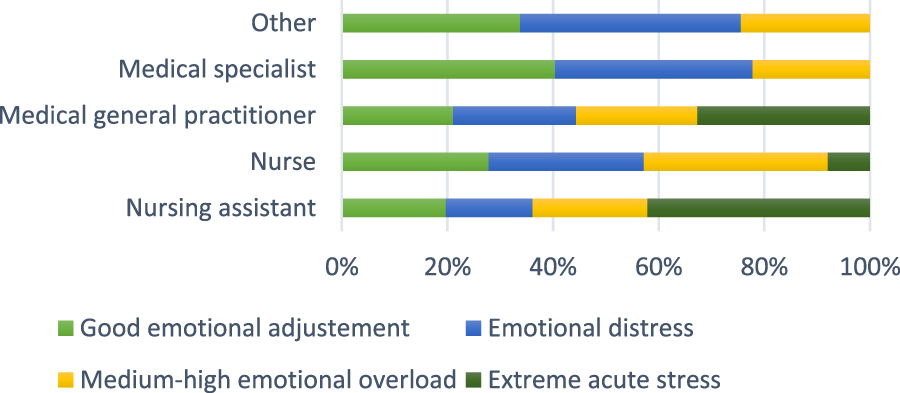
Percentage of emotional acute in the different levels according to the occupation Colombia 2017–2021.
Multiple Poisson regression between the main characteristics of participants and the Acute Stress Scale score in Colombia from 2017 to 2021.
The multiple regression analysis allows us, after adjusting for other co-variables of the model, to identify that being a medical specialist (PR 0.81; p-value = 0.01; CI = 0.74–0.89) and working at the first attention level (PR 0.71; p-value = 0.01; CI 0.66–0.76) were protective factors for presenting high-stress levels during the pandemic (Table 4).
TABLE 4
| Acute stress | PR | p-value | CI 95% | |
|---|---|---|---|---|
| LL | UL | |||
| Occupation | ||||
| Nurse | 0.96 | 0.157 | 0.90 | 1.02 |
| General practitioner | 1.08 | 0.055 | 1.00 | 1.16 |
| Medical specialist | 0.81 | 0.000* | 0.74 | 0.89 |
| Other | 0.96 | 0.312 | 0.90 | 1.04 |
| Nursing auxiliary | 1 ref | |||
| Sex | ||||
| Woman | 1.07 | 0.043** | 1.00 | 1.14 |
| Men | 1 ref | |||
| Marital status | ||||
| Married or free Union | 1.05 | 0.078 | 1.00 | 1.10 |
| Divorced or widowed | 1.15 | 0.013** | 1.03 | 1.28 |
| Single | 1 ref | |||
| Level of institution | ||||
| Second level | 1.18 | 0.000* | 1.10 | 1.27 |
| Third level | 1.19 | 0.000* | 1.10 | 1.28 |
| Fourth level | 1.41 | 0.000* | 1.31 | 0.90 |
| First level | 1 ref | |||
| Involved in a past event | ||||
| Yes | 1.30 | 0.000* | 1.24 | 1.36 |
| No | 1 ref | |||
| Type of institution | ||||
| Private | 1.49 | 0.000* | 1.27 | 1.76 |
| Public | 1.64 | 0.000* | 1.38 | 1.94 |
| Mixed | 1 ref | |||
Multiple Poisson regression between the main characteristics of participants and the Acute Stress Scale (EASE) score Colombia 2017–2021.
Notes: LL, Lower Limit; UL, Upper Limit; *p-value <0.01; **p-value <0.05; Mean VIF collinearity 2.33; Model p < 0.01.
On the other hand, it showed that factors such as being a general physician (PR 1.08; p-value = 0.055; CI 1.00–1.16), being a woman (PR 1.07; p-value = 0.043; CI 1.00–1.14), being divorced or widowed (PR 1.15; p-value = 0.01; CI 1.03–1.28), having been involved in a stressful event previously (PR = 1.30; p-value = 0.01; CI 1.24–1.36), working in private institutions (PR = 1.49; p-value 0.01; CI 1.27–1.76), and working and public institutions (PR = 1.64; p-value = 0.01; CI 1.38–1.94), increased the chance of presenting higher levels of stress (Table 4).
Discussion
The present study showed important results as to how the prevalence of medium-high stress and acute stress was 21.91% and 3.53% respectively in the human talent in institutional health in the three Colombian regions, who reported adverse events in the study period. Equally, it revealed the high prevalence of medium and high stress in medical professionals (14.1%), nursing professionals (28.9%), and nursing assistants (37.8%), with mostly women responding (84.4%).
In this sense, a study that used the same instrument, the Self-applied Acute Stress Scale (EASE) tool, in countries in the Latin Americans (Argentina, Colombia, Chile, and Ecuador), on health providers during the COVID-19 pandemic, but in which it was not compared with the presentation of adverse events, found similar results, wherein medium-high stress had a prevalence of 27% [29]. However, studies are few that have measured the factors related to the presentation of acute stress after an adverse events that use this instrument in the region. Multiple studies have evaluated the prevalence of stress in health personnel in the world before and during the pandemic, which coincides with the high prevalence of stress in this population, being one of the factors associated, with employment dissatisfaction and belonging to occupations such as medicine and nursing [30]. Also, it is important to highlight that around the phenomenon of secondary victims, one of the main negative impacts is acute stress and post-traumatic stress that will coincide with what was found in this study [11, 13, 31, 32].
As a limitation, we can mention that we would have preferred more homogeneity in the professions of the sample, in general. The sample was predominated by nurses and nursing assistants, as well as being predominantly female due to the greater presence of that gender in the human talent in health [27]. The policy of human talent in Colombia health aims that the stratification is balanced and thus closer to the representability of the population of workers, which could not be achieved at all in the samples since participation was free, open, and voluntary.
Among its contributions, this study found the reaffirmation of the reliability of the (EASE) in health providers in the context of Colombia in consonance with the results of other studies made in Iberoamerica, like way measuring tool for acute effective stress in the health population, that before the presentation of an adverse event can be used in a routine way within the interventions protocols for secondary victims around the diagnosis of acute stress as impact-relevant in the phenomenon of secondary victims [26–29]. For another part, this study allows identifying some factors related to the prevalence of acute stress after the presentation of the adverse event in the study population of the country, being one of the first studies in this context.
For another part, due to the limitations of a non-probabilistic sample, the study cannot identify risk factors between the different health issues, ideally future studies should implementprobabilistic sampling and make epidemiological data designs that allow the estimation of risk factors associated with acute stress and the presentation of adverse events in the human talent in health that allow extrapolating the results.
In conclusion, the prevalence of acute stress following an event adverse result is relevant in the studied population, which demonstrates that it is necessary to prioritize diagnosis and secondary victims in health institutions Colombians, in the regions evaluated.
It is also suggested to implement intervention strategies within the framework of management and health and safety systems at work, within actions aimed at mitigating risk social psycho in health providers with professional and auxiliary nursing staff, because they are the largest population in the health institutions and more likely to present adverse events, for most activities related to patient care.
It is important to mention that this study served as an element for the elaboration of the National Guide of Recommendations for the Care of Secondary and Tertiary Victims after an Adverse Event in Colombian Health Institutions.
Statements
Ethics statement
The studies involving humans were approved by Comité de Ética en Investigación-Fundación Universitaria Sanitas Comité Institucional de Ética en Investigación CEBIS- Fundación Universitaria del Área Andina. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MG, ER, and JC designed the study, reviewed the literature, participated in data analysis, and prepared a first draft of this manuscript. JM guided the framework, statistical approach, and the final manuscript’s elaboration. DR prepared a first draft of this manuscript. AS, LA, CV, and JM reviewed the literature. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that they do not have any conflicts of interest.
References
1.
Organización Mundial de la Salud. Seguridad del Paciente (2019). Available from: https://www.who.int/es/news-room/fact-sheets/detail/patient-safety (Accessed March 1, 2023).
2.
Aranaz-Andrés JM Aibar-Remón C Limón-Ramírez R Amarilla A Restrepo FR Urroz O et al IBEAS Design: Adverse Events Prevalence in Latin American Hospitals. Rev Calid Asist (2011) 26(3):194–200. 10.1016/j.cali.2010.12.001
3.
Montserrat-Capella D Suárez M Ortiz L Mira JJ Duarte HG Reveiz L et al Frequency of Ambulatory Care Adverse Events in Latin American Countries: The AMBEAS/PAHO Cohort Study. Int J Qual Heal Care J Int Soc Qual Heal Care (2015) 27(1):52–9. 10.1093/intqhc/mzu100
4.
De Sanidad M Consumo Y . Estudio Nacional Sobre los Efectos Adversos Ligados a la Hospitalización. ENEAS 2005 (2006).
5.
Wu AW Steckelberg RC . Medical Error, Incident Investigation and the Second Victim: Doing Better but Feeling Worse?BMJ Qual Saf (2012) 21:267–70. 10.1136/bmjqs-2011-000605
6.
Seys D Wu AW Van Gerven E Vleugels A Euwema M Panella M et al Health Care Professionals as Second Victims After Adverse Events: A Systematic Review. Eval Health Prof (2013) 36(2):135–62. 10.1177/0163278712458918
7.
Wu AW . Medical error: The Second Victim. The Doctor Who Makes the Mistake Needs Help Too. BMJ (2000) 320:726–7. 10.1136/bmj.320.7237.726
8.
Coughlan B Powell D Higgins MF . The Second Victim: A Review. Eur J Obstet Gynecol Reprod Biol (2017) 213:11–6. 10.1016/j.ejogrb.2017.04.002
9.
Werthman JA Brown A Cole I Sells JR Dharmasukrit C Rovinski-Wagner C et al Second Victim Phenomenon and Nursing Support: An Integrative Review. J Radiol Nurs (2021) 40(2):139–45. 10.1016/j.jradnu.2020.12.014
10.
Vanhaecht K Seys D Russotto S Strametz R Mira J Sigurgeirsdóttir S et al An Evidence and Consensus-Based Definition of Second Victim: A Strategic Topic in Healthcare Quality, Patient Safety, Person-Centeredness and Human Resource Management. Int J Environ Res Public Health (2022) 19(24):16869–10. 10.3390/ijerph192416869
11.
Martens J Van Gerven E Lannoy K Panella M Euwema M Sermeus W et al Serious Reportable Events Within the Inpatient Mental Health Care: Impact on Physicians and Nurses. Rev Calid Asist (2016) 31:26–33. 10.1016/j.cali.2016.04.004
12.
Wu AW Shapiro J Harrison R Scott SD Connors C Kenney L et al The Impact of Adverse Events on Clinicians: What’s in a Name? J Patient Saf (2020) 16(1):65–72. 10.1097/PTS.0000000000000256
13.
Scott SD Hirschinger LE Cox KR McCoig M Brandt J Hall LW . The Natural History of Recovery for the Healthcare Provider "Second Victim" After Adverse Patient Events. Qual Saf Health Care (2009) 18(5):325–30. 10.1136/qshc.2009.032870
14.
Avila J . El Estrés un Problema de Salud del Mundo Actual. Rev Con-ciencia (2014) 2(1):115–24. Available from: http://www.scielo.org.bo/scielo.php?script=sci_arttext&pid=S2310-02652014000100013&lng=es&nrm=iso&tlng=es%0Ahttp://www.scielo.org.bo/scielo.php?script=sci_abstract&pid=S2310-02652014000100013&lng=es&nrm=iso&tlng=es%0Ahttp://www.scielo.org.bo/pdf/rcfb/v2n1 (Accessed March 1, 2023).
15.
Strametz R Koch P Vogelgesang A Burbridge A Rösner H Abloescher M et al Prevalence of Second Victims, Risk Factors and Support Strategies Among Young German Physicians in Internal Medicine (SeViD-I Survey). J Occup Med Toxicol (2021) 16(1):11. 10.1186/s12995-021-00300-8
16.
Dukhanin V Edrees HH Connors CA Kang E Norvell M Wu AW . Case: A Second Victim Support Program in Pediatrics: Successes and Challenges to Implementation. J Pediatr Nurs (2018) 41:54–9. 10.1016/j.pedn.2018.01.011
17.
Gupta K Lisker S Rivadeneira NA Mangurian C Linos E Sarkar U . Decisions and Repercussions of Second Victim Experiences for Mothers in Medicine (SAVE DR MoM). BMJ Qual Saf (2019) 28(7):564–73. 10.1136/bmjqs-2018-008372
18.
Connors CA Dukhanin V Norvell M Wu AW . RISE: Exploring Volunteer Retention and Sustainability of a Second Victim Support Program. J Healthc Manag (2021) 66(1):19–32. 10.1097/JHM-D-19-00264
19.
Wu AW Connors CA Norvell M . Adapting RISE: Meeting the Needs of Healthcare Workers during the COVID-19 Pandemic. Int Rev Psychiatry (2021) 33(8):711–7. 10.1080/09540261.2021.2013783
20.
Edrees H Connors C Paine L Norvell M Taylor H Wu AW . Implementing the RISE Second Victim Support Programme at the Johns Hopkins Hospital: A Case Study. BMJ Open (2016) 6(9):e011708. 10.1136/bmjopen-2016-011708
21.
Prasad K McLoughlin C Stillman M Poplau S Goelz E Taylor S et al Prevalence and Correlates of Stress and Burnout Among U.S. Healthcare Workers During the COVID-19 Pandemic: A National Cross-Sectional Survey Study. EClinicalMedicine (2021) 35:100879. 10.1016/j.eclinm.2021.100879
22.
Salari N Khazaie H Hosseinian-Far A Khaledi-Paveh B Kazeminia M Mohammadi M et al The Prevalence of Stress, Anxiety and Depression Within Front-Line Healthcare Workers Caring for COVID-19 Patients: A Systematic Review and Meta-Regression. Hum Resour Health (2020) 18(1):100–14. 10.1186/s12960-020-00544-1
23.
Yıldırım M Çiçek İ Şanlı ME . Coronavirus Stress and COVID-19 Burnout Among Healthcare Staffs: The Mediating Role of Optimism and Social Connectedness. Curr Psychol (2021) 40(11):5763–71. 10.1007/s12144-021-01781-w
24.
Shahrour G Dardas LA . Acute Stress Disorder, Coping Self-Efficacy and Subsequent Psychological Distress Among Nurses Amid COVID-19. J Nurs Manag (2020) 28(7):1686–95. 10.1111/jonm.13124
25.
Wang X Cheng Z . Cross-Sectional Studies: Strengths, Weaknesses, and Recommendations. Chest (2020) 158(1S):S65–71. 10.1016/j.chest.2020.03.012
26.
Mira JJ Cobos A García OM Domínguez MJB Astier-Peña MP Pérez PP et al An Acute Stress Scale for Health Care Professionals Caring for Patients With Covid-19: Validation Study. JMIR Form Res (2021) 5(3):e27107. 10.2196/27107
27.
Cebrián-Cuenca A Mira JJ Caride-Miana E Fernández-Jiménez A Orozco-Beltrán D . Sources of Psychological Distress Among Primary Care Physicians during the COVID-19 Pandemic’s First Wave in Spain: A Cross-Sectional Study. Prim Heal Care Res Dev (2021) 22:e55. 10.1017/S1463423621000566
28.
Casal J Mateu E . Tamaño de la Muestra Universitat Autònoma de Barcelona (2003). Available from: http://optimierung.mathematik.uni-kl.de/mamaeusch/veroeffentlichungen/ver_texte/sampling_es.pdf.
29.
Martin-Delgado J Poblete R Serpa P Mula A Carrillo I Fernández C et al Contributing Factors for Acute Stress in Healthcare Workers Caring for COVID-19 Patients in Argentina, Chile, Colombia, and Ecuador. Sci Rep (2022) 12(1):8496–10. 10.1038/s41598-022-12626-2
30.
Kwiecień-Jaguś K Mędrzycka-Dąbrowska W Chamienia A Kielaite V . Stress Factors vs. Job Satisfaction Among Nursing Staff in the Pomeranian Province (Poland) and the Vilnius Region (Lithuania). Ann Agric Environ Med (2018) 25(4):616–24. 10.26444/aaem/75801
31.
Flórez F López L Bernal C . Prevalence of Adverse Events and Their Manifestations in Health Professionals as Second Victims. Biomedica (2022) 42(1):184–95. 10.7705/biomedica.6169
32.
Harrison R Lawton R Perlo J Gardner P Armitage G Shapiro J . Emotion and Coping in the Aftermath of Medical Error: A Cross-Country Exploration. J Patient Saf (2015) 11(1):28–35. 10.1097/PTS.0b013e3182979b6f
Summary
Keywords
stress disorders, traumatic, acute, health personnel, psychosocial risk
Citation
Gonzalez Delgado M, Cortes Gil JD, Rodriguez Araujo DL, Mira Solves JJ, Rodriguez Gallo EB, Salcedo Monsalve A, Arrieta Arteta LA, Villalba Toquica CdP and Morales Ruiz JC (2023) Acute Stress in Health Workers in Colombia 2017–2021: A Cross-Sectional Study. Int J Public Health 68:1606274. doi: 10.3389/ijph.2023.1606274
Received
04 June 2023
Accepted
16 August 2023
Published
01 September 2023
Volume
68 - 2023
Edited by
Gabriel Gulis, University of Southern Denmark, Denmark
Reviewed by
Ahsan Ahsan, University of Brawijaya, Indonesia
Rafael Manzanera, Pompeu Fabra University, Spain
Updates
Copyright
© 2023 Gonzalez Delgado, Cortes Gil, Rodriguez Araujo, Mira Solves, Rodriguez Gallo, Salcedo Monsalve, Arrieta Arteta, Villalba Toquica and Morales Ruiz.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mery Gonzalez Delgado, megonzalez2@areandina.edu.co
†These authors have contributed equally to this work and share first authorship
This Original Article is part of the IJPH Special Issue “Public Health and Primary Care, is 1 + 1 = 1?”
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.