Abstract
Objectives:
Individual placement and support (IPS) is an evidence-based form of vocational rehabilitation that aims to help people with mental illness obtain and remain in competitive employment. The objective of this study is to quantify the national growth of IPS over an 8-year period in Norway.
Methods:
Using a combination of qualitative and registry data, we map how IPS was implemented in Norway between 2012 and 2019, both in terms of geographic availability and intensity of service provision.
Results:
In 2012 IPS was available in 4 out of 19 counties, with 14.9% of the population living in an area where IPS was present. By 2019 this had increased to all 19 counties in Norway, and more than 70% of the population lived in an area of Norway where IPS was available. The results are presented in eight heat maps that visually display how the intensity and availability of the service have expanded.
Conclusion:
This study has identified when and where IPS became available in Norway, which is key to future effectiveness studies of IPS in the IPSRON project.
Introduction
As Aristotle said, “virtues are formed in man by his doing actions” [1]. As adults in any human society work is an essential part of our lives. Work is not only a means to provide for oneself and one’s relatives; it is also important for social inclusion, empowerment, self-esteem and recovery from illness [2, 3]. The right to work is a fundamental human right for those who wish to do so [4, 5]; however, individuals with mental health conditions are disproportionately affected by labor market exclusion, as these conditions are associated with disability and welfare dependency [6]. For individuals diagnosed with severe mental illness (SMI), gaining and retaining competitive employment is a challenge and is often a key goal [7–9]. Individual Placement and Support (IPS) is a supported employment model developed for individuals with mental illness. This model seeks to support individuals in gaining competitive employment while simultaneously providing the necessary mental health, social, and employment support to help them remain in employment. In essence, IPS is a “place-and-train” model, rather than the “train-and-place” approach that has dominated vocational rehabilitation for many years [10]. For individuals with mental illness, IPS has proven to be an effective approach to obtain and remain in competitive employment [11, 12] and the model is now available in more than 20 countries [13]. It is based on eight key principles, and IPS vocational units are subject to fidelity reviews to ensure adherence to these [14].
IPS first became available in Norway around 2010 and was gradually implemented across the country [15]. Funding transitioned gradually from project- and pilot-based allocations to more stable, institutional funding provided by the Norwegian Labour and Welfare Administration (Nav) [16]. According to Moe et al. [16], it took clinicians 15 years from first becoming aware of the concept to implementing it at scale. IPS is now part of the Norwegian national guidelines for the treatment of individuals diagnosed with psychosis who seek employment [17]. IPS is thus a policy, reflected in national strategies, plans and funding [18, 19]. With respect to the target group for the model, the recently published Norwegian guidelines state that IPS should be prioritized for individuals with SMI and/or substance abuse [20]. In addition, the guidelines also state that IPS should be made available for subjects with moderate mental illness requiring long-term and comprehensive work rehabilitation. In a Norwegian study on IPS conducted in 2014 [21], approximately 45% of patients had SMI and 55% had moderate mental illness. Key actors in the provision of Norwegian IPS services are the client’s clinician from mental health services, a welfare sector counsellor from Nav, Employment Specialists (ESs) and the IPS supervisors. The ES works closely with the IPS clients, supporting them in obtaining and maintaining competitive employment. To this end, the ES is expected to collaborate with the client’s potential employers, the client’s clinicians and public employment agencies [16], and thus play a coordinating role in the vocational rehabilitation process of their clients. IPS supervisors, on the other hand, ensure that IPS vocational units adhere to the eight principles of IPS, which are key to the successful delivery and efficacy of the service, and also perform fidelity reviews [22].
To achieve the policy ambition of helping more individuals with mental health conditions gain competitive employment, it is integral to public service resource planning to quantify the availability of the service that will achieve this. As an example, public services such as healthcare and education are often planned on a per capita basis (e.g., the number of general practitioners, teachers, etc. per 100,000 individuals), and per geographic unit (e.g., municipality level). IPS guidance from England suggests that an ES will work with 40–50 clients over the course of 1 year [23]. Accordingly, the number of clients who may receive IPS in a region depends in part on the number of ESs in that region. Developing an IPS workforce is a challenge [16, 24, 25], and an overview of how the ES workforce develops throughout the stages of IPS implementation is lacking. There is an abundance of trials demonstrating the superior efficacy [26, 27] and cost-effectiveness [28] of IPS compared to traditional vocational rehabilitation. Despite these merits little is known about whether the efficacy of IPS in controlled settings translates into societal effectiveness once it has been fully implemented. A difference-in-difference study examining the effect of IPS implementation on employment outcomes in a municipality showed promising results regarding societal effectiveness; however, the study was based on implementation in one municipality only and needs to be replicated on a larger scale [29].
Our study is part of the IPSRON project, which is led by the Centre for Work and Mental Health (CWMH) at Nordland Hospital in Bodø. The IPSRON project will investigate the societal and economic consequences of IPS implementation in Norway. Specifically, the project aims to investigate whether the implementation of IPS has had effects on outcomes such as employment, sickness absence (SA), disability benefits (DB), work assessment allowance (WAA), healthcare utilization, housing, loneliness, and crime among individuals with mental illness aged between 18 and 45. This age group was selected as it corresponded with the age of the majority of IPS clients [30]. In the present study, we examine the availability of IPS in Norwegian municipalities between 2012 and 2019. Our study is a unique opportunity to capture and develop knowledge about how the large-scale expansion of a new service develops. At the same time, we provide a means to illustrate how the service has evolved from being a limited resource to near-population coverage in Norway.
Methods
Setting
Our study is set in Norway, a country with a population of approximately 5.5 million inhabitants. The country is administratively organized into 15 counties, which are further divided into 357 municipalities. In 2015, the Norwegian parliament unanimously agreed on a reform of the municipalities and counties, with several merging to form new and larger units. Nevertheless, in 2024 the number of inhabitants in municipalities ranged from 215 in the smallest to 717,710 in the largest [31].
Norway is a wealthy country, with a more equal distribution of wealth than many other OECD countries [32]. Healthcare is public, free and financed through taxation. The healthcare service is organized as a two-tier, publicly funded system free at the point of access, with specialist mental health services prioritizing individuals with the most severe conditions. The specialist healthcare sector is organized into five regional health authorities. IPS ESs, however, is presently organized through local Nav offices, although this was not necessarily the case during our study period. The IPS vocational unit (ESs) is supervised by IPS supervisors who are also employed in Nav. When IPS was first implemented in Norway, it was primarily driven by clinicians working in the specialist healthcare sector who were looking for new and promising treatments for individuals with mental illness [16]. This engagement led to considerable efforts being made to gain knowledge about the IPS model, secure funds, and incorporate employment support into treatment teams. Crucially, this approach aligned with the policy ambition to prioritize functional recovery in the rehabilitation of individuals with mental illness, particularly by fostering cross-sectoral collaboration and integrating services, making IPS especially well-suited to achieving this goal [16, 33]. The national implementation of IPS in Norway has been supported by a structured system of coordination and capacity-building. The Norwegian Labour and Welfare Directorate has facilitated a national project group, regular online forums, and training initiatives, while regional IPS coordinators in each county work to sustain program fidelity locally [34].
Design and Data Collection
This study quantified the presence and intensity of IPS service provision in Norway. To this end we first obtained from the Norwegian Directorate of Health a list of all services that had received funding for positions as ESs in the period 2012–2018. This was supplemented with a list of every service that had conducted fidelity reviews, which we obtained from a senior IPS trainer at the county level. The project was introduced in a digital briefing for all the county-level IPS trainers. Then, the trainers were sent a list of all the IPS services that we were aware of in their respective counties. The trainers were asked to quality check the list and expand it with any other known IPS services in the county, whether currently active or not. We also asked the trainers to provide a contact person for each service. Our final list included 73 IPS vocational units. The IPS supervisors were contacted and asked to participate in a semi-structured qualitative interview about the implementation of IPS. The interview guide was developed by the IPSRON research team, and is attached in Supplementary File S1. The interviews were conducted by two staff members from CWMH between 2021 and 2023.
Data Analyses
Following the interviews, we extracted and quantified key variables for each vocational unit by year of operation. Variables derived from the interviews included the number of ESs, their locations, and the municipalities served by the health services where the ESs were integrated. We retrieved a list of all municipalities, their unique municipality numbers, and the annual populations per municipality for the years 2012–2019 from Statistics Norway [31]. We then summarized the total population served by each IPS vocational unit (for each year in our study period) and calculated the intensity of IPS, operationalized as the number of ESs per 100,000 individuals per year. After a national reform of municipalities between 2013 and 2021, the number of municipalities in Norway was reduced from 428 to 356 [35]. Since point of contact described IPS provision per vocational unit based on the municipal structure at the time of the interview, this influenced how municipal coverage was determined for each year. Specifically, if municipalities “x” and “z” were merged into municipality “y” in 2018, we considered IPS to have been available in both municipalities “x” and “z” in 2017 if our informant reported on municipality “y” at the time of the interview.
We were unable to obtain data on the number of ESs from four IPS vocational units for some of the years, either because the informant in question did not possess this data or because we were unable to obtain an informant from the vocational unit. To impute a reliable estimate of the expected number of ESs, we used a regression imputation technique. We included data on population size and the number of ESs from each vocational unit with complete data in linear regression models, treating the number of ESs as the dependent variable and the population size of the municipality where the IPS vocational units were located as the independent variable. For each of the four vocational units with missing ES data we calculated the expected number of ESs, using the constant and beta coefficients from the regressions, along with the population size of the vocational units with missing ES data (Supplementary File S2).
The data on the number of ESs was extrapolated to the population data for all Norwegian municipalities each year, enabling the calculation of the intensity of IPS for each municipality each year. For municipalities served by more than one IPS vocational unit, the intensity of each unit serving the municipality was summarized. These tables provide the underlying data for the annual heat maps showing IPS expansion across Norway. The heat maps were produced using Flourish, an online graphical software tool (Canva UK Operations Ltd, Hoxton Square London N1 6NN). Heat maps provide a means to illustrate incremental changes in the implementation of IPS over an 8-year period in a manner more easily interpreted than tables, not least since the number of municipalities in Norway during the study period was more than 400. Finally, we also aggregated data on geographical coverage of IPS, population coverage of IPS, intensity of IPS and population density to the county level to give an indication of how IPS was implemented at the regional level during the study period.
Results
Table 1 provides an overview of the aggregated characteristics of the 73 IPS vocational units. In 2012, there were five operational IPS vocational units. On average, the number of ESs per vocational unit was 1.7 (SD 1.3). By 2019 the number of vocational units had increased to 55, and the number of ESs was on average 3.6 (SD 2.0).
TABLE 1
| Number of IPS vocational units per year | n | Mean (sd) |
|---|---|---|
| Number of IPS vocational units per year | ||
| 2012 | 5 | |
| 2013 | 11 | |
| 2014 | 12 | |
| 2015 | 14 | |
| 2016 | 19 | |
| 2017 | 21 | |
| 2018 | 37 | |
| 2019 | 55 | |
| Average number of employment specialists per vocational unit in 2012 | 1.7 (1.3) | |
| Average number of employment specialists per vocational unit in 2019 | 3.6 (2.0) | |
Characteristics of individual placement and support vocational units in 2012–2019 (Nordland, Norway, 2025).
Geographical and population coverage of IPS, along with its intensity at the county level is provided in Supplementary File S3. In 2012, 4 out of 19 counties had IPS vocational units, covering between 3.9% and 69.7% of the municipalities within the counties. Population coverage was generally higher (14.8%), and the intensity of service provision was 1.0 ES/100,000. By 2019, IPS was present in all counties, with 49.4% of all municipalities having access to it. Population coverage was substantially higher, with 70.9% of the Norwegian population living in a municipality where IPS was provided. By 2019, the intensity of IPS had increased to 6.1 ES/100,000.
Figure 1 shows eight annual heat maps for IPS intensity per municipality. These maps illustrate the general pattern shown in Supplementary File S3 at a more detailed level. As can be seen in the early years, IPS was not available in the majority of municipalities. Over the years, IPS became available in new areas, but the intensity of service provision also increased substantially in areas where it was already established. By the end of our observation period, IPS had expanded to all major populated areas of Norway, and the intensity of service provision had increased to a substantially higher level than was the case initially.
FIGURE 1
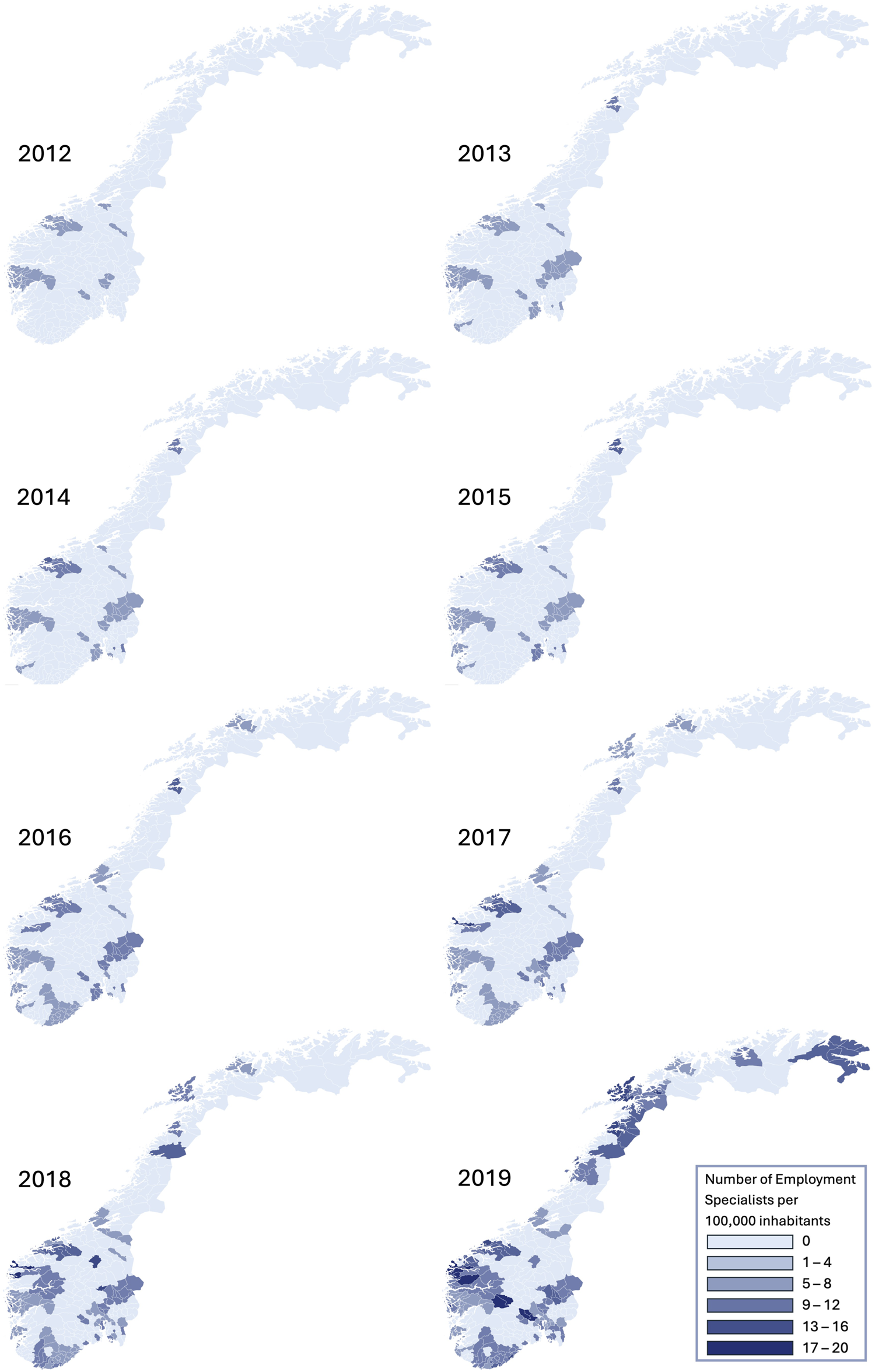
Intensity of individual placement and support in Norway from 2012 to 2019 (Nordland, Norway, 2025).
Discussion
Using a combination of qualitative and quantitative data we have presented the scaling up of IPS in Norway over a period of 8 years. To our knowledge, this is the first study to simultaneously present the nationwide growth of IPS over an 8-year period in terms of both geographic availability and intensity of provision. Our findings demonstrate that the process from proven efficacy, clinical initiatives and policy ambition to full scale implementation of a new service takes time and involves challenging processes. The efficacy of IPS has been demonstrated in several clinical trials and the service is now available on a large scale in Norway. The next logical step is to evaluate IPS in naturalistic effectiveness studies, which the present study has now paved the way for.
The link between geography and health is fundamental to epidemiology and has long been recognized as an important area for health service research and public planning. Perhaps the most famous example of how the concentration of events in a given geographical area can be used to understand a health problem is John Snow’s identification of the Broad Street pump as the epicenter of a cholera epidemic in 19th-century London [36]. More recently heat maps have been put to use for several purposes, with examples including studies of geographical differences in medication [37], access to invasive care in rural Canada [38] and mental health and education [39]. Although this is the first heat map of IPS growth to be published, there are some notable studies that are comparable and can provide context to our results. Mascayano and colleagues recently examined how IPS has expanded in the United States over the last decades and reported that the number of IPS programs now exceeds 1,000 [40]. Pogue et al. [41] conducted telephone interviews with mental health representatives from all 50 states in the United States, and examined the growth of IPS over a three-year period. They observed a substantial expansion of IPS services and found that IPS was available in 80% of states by 2019. Johnson-Kwochka et. al [42] calculated the state IPS program penetration rate as the number of IPS programs per 1 million inhabitants in the 50 US states. The authors observed rates ranging from 0.05 to 16.62 per 1 million individuals, which converts to 0.005-1.7 ES per 100,000 individuals. In England, national guidance states an aspiration of 1 IPS ES per 50,000 individuals in the general population, or 2 ES per 100,000 individuals in the general population [23]. These figures are calculations of service provision using the general population as the denominator. Applying a more specific target group as the denominator will of course have an impact on the ratio. As an example, Cram et. al calculated that the average intensity of ES was 3.7 per 10,000 individuals seen by a district health board’s specialist mental health and addiction services in New Zealand nationally. This would amount to 37 ESs per 100,000 individuals, but as the denominator is a more specific group than the general population the intensity of service provision is naturally higher [43]. Service intensity must also account for population density, as it reflects the geographical challenges of providing IPS in certain areas where ESs spend more time traveling to meet with clients. This is especially important in a country such as Norway, where distances, topography and weather conditions can obstruct access to support. The maps provided indicate that geographically, IPS is not present everywhere, but as is evident in Supplementary File S3, the service is available to the majority of the population, collectively illustrating how population density affects service provision. In terms of need versus capacity, the prevalence of individuals with mental illness at any given time varies according to the level of affluence and deprivation between regions [44]. As an example the prevalence of certain SMIs in Norway has been estimated to range between 1,200 and 2,300 per 100,000 individuals [45]. As eligibility for IPS is not only determined by age or diagnosis, it is challenging to extrapolate these figures to calculate the sufficient intensity of IPS service provision. Our results indicate that at a national level, the average IPS intensity was 6.1 ES per capita in 2019. Applying the England estimates for caseload per ES [23], this intensity corresponds to approximately 240–300 clients seen by an ES annually in a population of 100,000 individuals. Data from the Netherlands suggest that 2% of individuals using mental health services accessed IPS [46]. This rate is consistent with previous studies from the United States that found similar results within mental health services [47, 48]. However, as countries have expanded and scaled up IPS services, we now find access rates of around 9% in England [30] and Norway [29].
Several randomized controlled trials have been conducted on the effects of IPS, and the efficacy of the service is well documented [26]. It is however less certain whether a clinical service provided in a controlled setting will extend to a societal footprint when implemented in real-world settings. Consequently, understanding how the funding, scaling up and implementation of services unfold is imperative. Our results demonstrate substantial variation in the two key variables: the geographical availability of the service and the intensity of its provision. In any system where variance develops inequalities are naturally created, and in the case of IPS such inequalities undermine health equity. The practical consequence is that access to evidence-based care is highly dependent on area of residence, despite the service’s proven effectiveness and policy ambitions. It is difficult to pinpoint why such variation occurs, but prioritization within health services and funding schemes may be important factors. It is commonly recognized that implementation efforts are complex. How policies, stakeholders and processes interact can result in unpredictability, uncertainty and unintended consequences. A further challenge in scaling up services is balancing the goal of reaching the highest number of individuals with prioritizing those most in need. There are several obstacles to the successful implementation of IPS [24, 49, 50]. In the case of IPS implementation in Norway, funding for IPS became available in different formats and from different sources, leading to a case of organic stepwise growth rather than a planned and equal distribution across the country [16]. While IPS implementation was clearly anchored in policy ambition, it lacked a clear mandate and an official directive until recently. The development and growth of IPS in Norway has been detailed elsewhere, highlighting change agents, government use of research, funding, clarifications of sectoral interfaces and legal issues [16]. The empirical data collected in our study will enable us to study the consequences of this stepwise and organic form of growth, and the societal footprint of IPS in Norway.
Limitations
This study has several strengths that contribute to the significance of our results and their implications. First, we conducted structured interviews with key IPS personnel to collect comprehensive data on the implementation of IPS throughout Norway. This ensured a nearly complete overview of every IPS vocational unit active during the study period, despite the absence of a central government funding scheme supporting their establishment. It should be noted that this form of data collection entails a risk of recall bias; however, the majority of the interviews took place within less than 5 years of the establishment of the vocational unit. We therefore believe that this risk is minimal. The number of ESs per capita is quite consistent across IPS vocational units, serving as a validation of the data extrapolated from the interviews. Population data was obtained from national population registries, which are reliable and complete. Finally, the visual display of results which combined both time and intensity allows readers to comprehend the gradual increase and growth of IPS across an entire country and how access to care expanded with increasing investments.
Our study also has some limitations. The intensity of IPS was quantified as the number of ESs per capita per geographical region, but the majority of the population will never be candidates for IPS support. In regions where a large proportion of inhabitants are not in the target group for IPS a low number of ESs may appear to indicate low service provision intensity, when in reality the service is adequately staffed. However, presenting healthcare resources on a per capita basis is common practice [51], and other alternatives such as limiting the denominator to individuals considered as the key target group for IPS are more difficult for resource planning as more detailed data are required. Finally, we would ideally have complemented the number of ESs with IPS fidelity as an indicator of the quality of IPS service provision. The majority of vocational units had indeed been subject to fidelity reviews, but we were unable to obtain them. However, according to a report on Norwegian IPS services from 2024, 95% of responding vocational units stated that they had been subject to an internal or external fidelity review [52].
Conclusion
This study has quantified the geographic expansion and the increased intensity of IPS in Norway over an 8-year period, illustrating the journey from first initiatives to near population coverage. IPS expanded both geographically and in terms of intensity during the study period. Initially, 14.9% of the population lived in an area where IPS had been implemented, but by 2019 IPS was provided across the majority of Norway and 70.9% of the population lived in an area where IPS was available. Our study illustrates that the establishment and expansion of integrated employment support within mental health services is a gradual process: progressing from decision and ambition to full-scale implementation requires time and effort.
Statements
Ethics statement
This study was approved by the regional medical research ethics committee (REC North, #134553) and performed in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all informants in the study.
Author contributions
The study was conceived by AM, BB, and EK. NA drafted the paper and performed all analyses with assistance from LT. UK and KS performed the interviews. NA and KS extracted the quantitative data from the interviews. The interview guide was developed by BB and MR. LT produced the heat maps. MR, BB, AM, NA, CM, MB, TL, DM, A-LP, and EK are senior members in the IPSRON project, and have contributed significantly in decisions regarding methods and defining the exposure of IPS, as well as critically revising the manuscript in preparation. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the Research Council of Norway under project number #273665.
Conflict of interest
The authors declare that they do not have any conflicts of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2025.1608739/full#supplementary-material
SUPPLEMENTARY FILE S1Interview guide individual placement and support method supervisor (Nordland, Norway, 2025).
SUPPLEMENTARY FILE S2Imputation of individual placement and support intensity per year (Nordland, Norway, 2025).
SUPPLEMENTARY FILE S3Individual placement and support service provision per county during 2012–2019 (Nordland, Norway, 2025).
References
1.
Thomson JAK Tredennick H Barnes J . The Nicomachean Ethics. Penguin Publishing Group (2004). p. 400.
2.
Modini M Joyce S Mykletun A Christensen H Bryant RA Mitchell PB et al The Mental Health Benefits of Employment: Results of a Systematic Meta-Review. Australas Psychiatry (2016) 24(4):331–6. 10.1177/1039856215618523
3.
Boardman J Rinaldi M . Work, Unemployment and Mental Health. In: IkkosG, editor. Social History of Psychiatry and Mental Health in Britain 1960–2010. Cambridge University Press (2021). p. 326–35.
4.
United Nations General Assembly. The Universal Declaration of Human Rights. New York: United Nations General Assembly (1948).
5.
United Nations. Convention on the Rights of Persons with Disabilities. New York: United Nations (2006).
6.
Latimer E Ray-Chaudhuri S Waters T . The Role of Changing Health in Rising Health-Related Benefit Claims. London: Institute for Fiscal Studies (2025).
7.
Ramsay CE Broussard B Goulding SM Cristofaro S Hall D Kaslow NJ et al Life and Treatment Goals of Individuals Hospitalized for First-Episode Nonaffective Psychosis. Psychiatry Res (2011) 189(3):344–8. 10.1016/j.psychres.2011.05.039
8.
Iyer SN Mangala R Anitha J Thara R Malla AK . An Examination of Patient-Identified Goals for Treatment in a First-Episode Programme in Chennai, India. Early Interv Psychiatry (2011) 5(4):360–5. 10.1111/j.1751-7893.2011.00289.x
9.
Adamus C Richter D Sutor K Zürcher SJ Mötteli S . Preference for Competitive Employment in People with Mental Disorders: A Systematic Review and Meta-Analysis of Proportions. J Occ Rehab (2024) 35:143–58. 10.1007/s10926-024-10192-0
10.
Ernst W . Work, Psychiatry and Society, C. 1750-2015. Manchester, United Kingdom: Manchester University Press (2016). p. 398.
11.
Suijkerbuijk YB Schaafsma FG van Mechelen JC Ojajärvi A Corbière M Anema JR . Interventions for Obtaining and Maintaining Employment in Adults with Severe Mental Illness, a Network Meta-Analysis. Cochrane Database Syst Rev (2017) 9(9). 10.1002/14651858.CD011867.pub2
12.
Kinoshita Y Furukawa TA Kinoshita K Honyashiki M Omori IM Marshall M et al Supported Employment for Adults with Severe Mental Illness. Cochrane Database Syst Rev (2013) 2013:CD008297. 10.1002/14651858.CD008297.pub2
13.
Drake RE Becker DR Bond GR . Growth and Sustainment of Individual Placement and Support. Psychiatr Serv (2020) 71(10):1075–7. 10.1176/appi.ps.201900544
14.
Bond GR Peterson AE Becker DR Drake RE . Validation of the Revised Individual Placement and Support Fidelity Scale (IPS-25). Psychiatr Serv (2012) 63(8):758–63. 10.1176/appi.ps.201100476
15.
Sveinsdottir V Bull HC Evensen S Reme SE Knutzen T Lystad JU . A Short History of Individual Placement and Support in Norway. Psychiatr Rehabil J (2020) 43(1):9–17. 10.1037/prj0000366
16.
Moe C Brinchmann B Rasmussen L Brandseth OL McDaid D Killackey E et al Implementing Individual Placement and Support (IPS): The Experiences of Employment Specialists in the Early Implementation Phase of IPS in Northern Norway. The IPSNOR Study. BMC Psychiatry (2021) 21(1):632. 10.1186/s12888-021-03644-x
17.
Norwegian Directorate of Health. Nasjonal Faglig Retningslinje for Utredning, Behandling Og Oppfølging Av Personer Med Psykoselidelser. In: Department of Psychiatric Care and Substance Abuse. Oslo, Norway (2013).
18.
Norwegian Ministry of Health and Care Services and the Norwegian Ministry of Labour and Social Inclusion. National Strategic Plan for Work and Mental Health 2007-2012 (2009). Available online at: https://www.regjeringen.no/globalassets/upload/hod/vedlegg/planer/i-1127eweb.pdf (Accessed June 24, 2024).
19.
Norwegian Ministry of Health and Care. Parliament Proposition Nr. [Om Opptrappingsplan for Psykisk Helse 1999 – 2006] (1997). Available online at: https://www.regjeringen.no/no/dokumenter/stprp-nr-63-1997-98-/id201915/ (Accessed June 24, 2024).63
20.
Norwegian Directorate of Health. National Guidelines: Individual Placement and Support (IPS) (2025). Available online at: https://www.helsedirektoratet.no/faglige-rad/individuell-jobbstotte-ips-og-helseiarbeid/individuell-jobbstotte-ips (Accessed August 13, 2025).
21.
Reme SE Monstad K Fyhn T Sveinsdottir V Løvvik C Lie SA et al A Randomized Controlled Multicenter Trial of Individual Placement and Support for Patients with Moderate-To-Severe Mental Illness. Scand J Work Environ Health (2019) 45(1):33–41. 10.5271/sjweh.3753
22.
Drake RE Bond GR Becker DR . Individual Placement and Support: An Evidence-Based Approach to Supported Employment. Oxford University Press (2012).
23.
NHS England. Individual Placement and Support for Severe Mental Illness. Guidance for Integrated Care Systems (2023). Available online at: https://www.england.nhs.uk/long-read/individual-placement-and-support-for-severe-mental-illness/ (Accessed March 24, 2025).
24.
Butenko D Rinaldi M Brinchmann B Brandseth OL Killackey E Mykletun A . The Personality Profile of IPS Employment Specialists, and How It Relates to Job Satisfaction: A Longitudinal Cohort Study. Scand J Psychol (2023) 64(1):71–9. 10.1111/sjop.12864
25.
Butenko D Rinaldi M Moe C Brinchmann B Wittlund S Killackey E et al “What I Thought Was the Dream Job Was a Little Different Than I Had Expected”: A Qualitative Study Exploring the Turnover of IPS Employment Specialists. J Voc Rehab (2024) 61(1):79–91. 10.3233/jvr-240027
26.
Brinchmann B Widding-Havneraas T Modini M Rinaldi M Moe CF McDaid D et al A Meta-Regression of the Impact of Policy on the Efficacy of Individual Placement and Support. Acta Psychiatr Scand (2020) 141(3):206–20. 10.1111/acps.13129
27.
de Winter L Couwenbergh C van Weeghel J Sanches S Michon H Bond GR . Who Benefits from Individual Placement and Support? A Meta-Analysis. Epidemiol Psychiatr Sci (2022) 31:e50. 10.1017/S2045796022000300
28.
Park AL Rinaldi M Brinchmann B Killackey E Aars NAP Mykletun A et al Economic Analyses of Supported Employment Programmes for People with Mental Health Conditions: A Systematic Review. Eur Psychiatry (2022) 65(1):e51. 10.1192/j.eurpsy.2022.2309
29.
Brinchmann B Wittlund S Lorentzen T Moe C McDaid D Killackey E et al The Societal Impact of Individual Placement and Support Implementation on Employment Outcomes for Young Adults Receiving Temporary Health-Related Welfare Benefits: A Difference-In-Differences Study. Psychol Med (2024) 54(8):1787–95. 10.1017/S0033291723003744
30.
Rinaldi M Perkins R Baxter R Dorrington P Saville K . Individual Placement and Support (IPS): Duration of Employment Support and Equity of Access and Outcome in Routine Clinical Practice. B J Psych Bull (2024) 1–8. 10.1192/bjb.2024.68
31.
Statistics Norway. Population Per Municipality in Norway in 2024. Available online at: https://www.ssb.no/statbank/table/07459/tableViewLayout1/ (Accessed July 7, 2024).
32.
World Bank Data. Washington DC: World Bank (2019). Available online at: https://data.worldbank.org/indicator/SI.POV.GINI?locations=NO (Accessed June 25, 2024).
33.
Brinchmann B . Can Individual Placement and Support (IPS) Contribute to Change the Life of Individuals Experiencing Mental Health Problems? Challenges Related to Efficacy, Effectiveness, and Implementation. [dissertation]. Tromsø (Norway): UiT-The Arctic University of Norway (2025).
34.
Malmberg-Heimonen I Tøge AG Bråthen M Frøyland K Spjelkavik Ø Bond G et al Assessing Program Fidelity Patterns within the IPS for Young Adults in Norway. J Evid Based Soc Work (2025) 1–16. 10.1080/26408066.2025.2528910
35.
Norwegian Government. Reform of Municipalities (2025). Available online at: https://www.regjeringen.no/no/dokument/dep/kdd/sak/saksgang-kommunereformen/id2607187/ (Accessed March 3, 2025).
36.
Newsom SW . Pioneers in Infection Control: John Snow, Henry Whitehead, the Broad Street Pump, and the Beginnings of Geographical Epidemiology. J Hosp Infect (2006) 64(3):210–6. 10.1016/j.jhin.2006.05.020
37.
Almonacid C Fitas E Sánchez-Covisa J Gutiérrez H Rebollo P . Geographical Differences in the Use of Oral Corticosteroids in Patients with Severe Asthma in Spain: Heat Map Based on Existing Databases Analyses. BMC Pulm Med (2023) 23(1):3. 10.1186/s12890-022-02295-2
38.
Boyd JC Cox JL Hassan A Lutchmedial S Yip AM Légaré JF . Where You Live in Nova Scotia Can Significantly Impact Your Access to Lifesaving Cardiac Care: Access to Invasive Care Influences Survival. Can J Cardiol (2018) 34(2):202–8. 10.1016/j.cjca.2017.11.021
39.
Gao CX Clarke E Nicholas J Teo SM Koppe C Peter G et al Changes in Rates of Special Considerations in Higher Education Applications Pre- and during the COVID-19 Pandemic in Victoria, Australia. Early Interv Psych (2025) 19(1):e13603. 10.1111/eip.13603
40.
Mascayano F Swanson S Florence AC Patel SR Amsalem D Pope LG et al Scaling up Evidence-Based Supported Employment in the United States. Psychiatr Serv (2025) 76(5):486–96. 10.1176/appi.ps.20240083
41.
Pogue JA Bond GR Drake RE Becker DR Logsdon SM . Growth of IPS Supported Employment Programs in the United States: An Update. Psychiatr Serv (2021) 73(5):533–8. 10.1176/appi.ps.202100199
42.
Johnson-Kwochka A Bond GR Becker DR Drake RE Greene MA . Prevalence and Quality of Individual Placement and Support (IPS) Supported Employment in the United States. Adm Policy Ment Health (2017) 44(3):311–9. 10.1007/s10488-016-0787-5
43.
Cram F Jury S Kokaua J Ku B Lockett H Wilson M . Individual Placement and Support (IPS) in Aotearoa New Zealand – New Insights from Linked Administrative Data. New Zealand: Ministry of Social Development (2020).
44.
Reilly S Olier I Planner C Doran T Reeves D Ashcroft DM et al Inequalities in Physical Comorbidity: A Longitudinal Comparative Cohort Study of People with Severe Mental Illness in the UK. BMJ Open (2015) 5(12):e009010. 10.1136/bmjopen-2015-009010
45.
Norwegian Directorate of Health. Styringsinformasjon Til Helsefelleskapene. Del III: Pasienter Med Alvorlige Psykiske Lidelser. Oslo, Norway (2022).
46.
Vukadin M Zwinkels W Schaafsma F Spijkerman M de Graaf-Zijl M Delespaul P et al Effectiveness, Cost-Effectiveness and Return on Investment of Individual Placement and Support Compared with Traditional Vocational Rehabilitation for Individuals with Severe Mental Illness in the Netherlands: A Nationwide Implementation Study. BMJ Pub Health (2024) 2(1):e000393. 10.1136/bmjph-2023-000393
47.
Bruns EJ Kerns SE Pullmann MD Hensley SW Lutterman T Hoagwood KE . Research, Data, and Evidence-Based Treatment Use in State Behavioral Health Systems, 2001-2012. Psychiatr Serv (2016) 67(5):496–503. 10.1176/appi.ps.201500014
48.
Twamley EW Baker DG Norman SB Pittman JO Lohr JB Resnick SG . Veterans Health Administration Vocational Services for Operation Iraqi Freedom/Operation Enduring Freedom Veterans with Mental Health Conditions. J Rehabil Res Dev (2013) 50(5):663–70. 10.1682/jrrd.2012.08.0137
49.
Khalifa N Hadfield S Thomson L Talbot E Bird Y Schneider J et al Barriers and Facilitators to the Implementation of Individual Placement and Support (IPS) for Patients with Offending Histories in the Community: The United Kingdom Experience. Br J Occ Ther (2020) 83(3):179–90. 10.1177/0308022619879334
50.
Boardman J Rinaldi M . Difficulties in Implementing Supported Employment for People with Severe Mental Health Problems. Br J Psychiatry (2013) 203(3):247–9. 10.1192/bjp.bp.112.121962
51.
Saunes IS Karanikolos M Sagan A . Norway: Health System Review. Health Syst Transit (2020). 22, 1, 163. Available online at: https://eurohealthobservatory.who.int/publications/i/norway-health-system-review-20 (Accessed June 25, 2024).
52.
Samfunnsanalyse PROBA . Status for Individual Placement and Support (IPS) in Norway [Status for Individuell Jobbstøtte (IPS) I Norge] (2024). Oslo. Available online at: https://proba.no/rapporter/status-for-individuell-jobbstotte-ips-i-norge/ (Accessed: August 15, 2025).
Summary
Keywords
individual placement and support, implementation, geographical variation, mental health, health service accessibility
Citation
Aars NAP, Brinchmann B, Rinaldi M, Trichet LO, Kolstad U, Steen KS, Moe CF, Lorentzen T, Borg M, McDaid D, Park A-L, Killackey E and Mykletun A (2025) Mapping the Growth of Individual Placement and Support Services in Norway. Int. J. Public Health 70:1608739. doi: 10.3389/ijph.2025.1608739
Received
28 May 2025
Accepted
11 September 2025
Published
29 September 2025
Volume
70 - 2025
Edited by
Susan R. McGurk, Boston University, United States
Reviewed by
Torill Ueland, Oslo University Hospital, Norway
Gary Bond, Westat, United States
Updates
Copyright
© 2025 Aars, Brinchmann, Rinaldi, Trichet, Kolstad, Steen, Moe, Lorentzen, Borg, McDaid, Park, Killackey and Mykletun.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nils Abel Prestegård Aars, nils.abel.aars@nordlandssykehuset.no
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.