Abstract
Objectives: We investigated the associations of mean levels of leisure-time physical activity (LTPA) and latent LTPA trajectories with all-cause mortality risk.
Methods: Trajectories of LTPA were established using group-based trajectory analysis with a latent class growth model in a population-based cohort between 1996 and 2014. A Cox-proportional hazard model was conducted to examine the associations of LTPA quintiles and LTPA trajectories with all-cause mortality.
Results: A total of 21,211 participants (age 18–90 years) were analyzed (median follow-up 16.8 years). The study participants were divided into five groups according to percentiles of LTPA (<20th, 20th–<40th, 40th–<60th, 60th–<80th, ≥80th) and LTPA trajectories (low/stable, medium/stable, increasing, decreasing, and fluctuating), respectively. Participants with a decreasing trajectory did not have a significantly lower risk of all-cause mortality despite having the highest baseline level of LTPA. In contrast, participants with a medium/stable (HR 0.84, 95% CI 0.72–0.98, p = 0.031) or an increasing (HR 0.57, 95% CI 0.33–0.97, p = 0.037) trajectory had a significantly lower risk of all-cause mortality.
Conclusion: Promotion of maintaining stable LTPA is beneficial for public health and survival.
Introduction
Adopting a healthy lifestyle has been associated with longevity [1]. Physical activity is an important part of healthy lifestyles [1, 2], whereas physical inactivity has been shown to be associated with various non-communicable diseases, which are major burdens of public health worldwide [3]. Unfortunately, levels of physical activity have declined in most developed countries in recent decades [4, 5]. This decline may have contributed, at least in part, to the decrease in life expectancy [3–6]. According to a previous report [3], physical inactivity accounted for 9% of premature mortality worldwide in 2008. The authors estimated that if inactivity were decreased by 10%, more than 533 thousand deaths could be averted every year [3].
Evidence supporting the importance of maintaining physical activity to promote health has been found in a number of studies, which have reported an association of leisure-time physical activity (LTPA) with risk of mortality [7–13]. Nevertheless, the assessment of physical activity was conducted only at baseline in most of these investigations [9–13]. As lifestyle and physical activity might change during the follow-up period, this could constitute an important confounding factor when investigating the association between baseline LTPA and risk of all-cause mortality. To address this issue, levels of physical activity were assessed at several time points (mostly at two time points) in some studies [7, 8, 14–16] investigating their effects on risk of mortality.
In this study, we collected data on LTPA at several time points in a general population to establish LTPA trajectories using a validated method [17, 18] and investigated the associations of mean levels of LTPA and LTPA trajectories with risk of all-cause and cardiovascular/cancer mortality. The joint effects of LTPA levels and LTPA trajectories on all-cause and cardiovascular/cancer mortality were also examined.
Methods
This study was conducted in accordance with the Declaration of Helsinki. We analyzed data from a population-based cohort established by the MJ Health Management Institution, Taipei, Taiwan. All participants had undergone a health check-up between 1996 and 2014, and provided informed consent to authorize the MJ Health Management Institution to process data for research use. To apply the data, we firstly had our study protocol approved by an Institutional Review Board. We then applied for data from the MJ Health Database/MJ Health Survey Data with the approval of our study protocol. The MJ Health Management Institution approved our application and we have the data for analyses. The check-ups of each participant included anthropometric measurements, physical examination, laboratory tests (including fasting plasma glucose, serum creatinine, lipids profile, …), and questionnaires on medical history and assessment of LTPA. We selected participants who were at least 18 years old and had received more than 5 health check-ups in an 8-year period between 1996 and 2014 to establish their trajectories of LTPA for analyses.
Using information from the validated questionnaires [9, 19, 20], we determined the intensity, duration, and frequency of LTPA for each participant. The intensity was assessed using metabolic equivalent (MET) [9, 21]. A MET value was assigned [21] according to the intensity of physical activity (2.5 for light, 4.5 for moderate, 6.5 for medium-vigorous, and 8.5 for high-vigorous exercise). The MET value was multiplied by duration and frequency, and was expressed as MET-h per week. Repeated measures of the MET value were used to establish trajectories of LTPA (MET-h per week) using group-based trajectory analysis with a latent class growth model [17, 18]. We decided the number of trajectories according to the Information of Bayesian Information Criterion (BIC) [22]. Then the study participants were assigned to distinct trajectory groups by posterior probabilities from the trajectory model. This method allowed us to group study participants by “naturally occurring” LTPA trajectories [23]. The use of a censored normal model was appropriate due to the continuous outcomes of MET. The models were fitted using the SAS ProcTraj procedure [22]. Finally, five trajectories of LTPA were established (Figure 1; Supplementary Table S1).
FIGURE 1
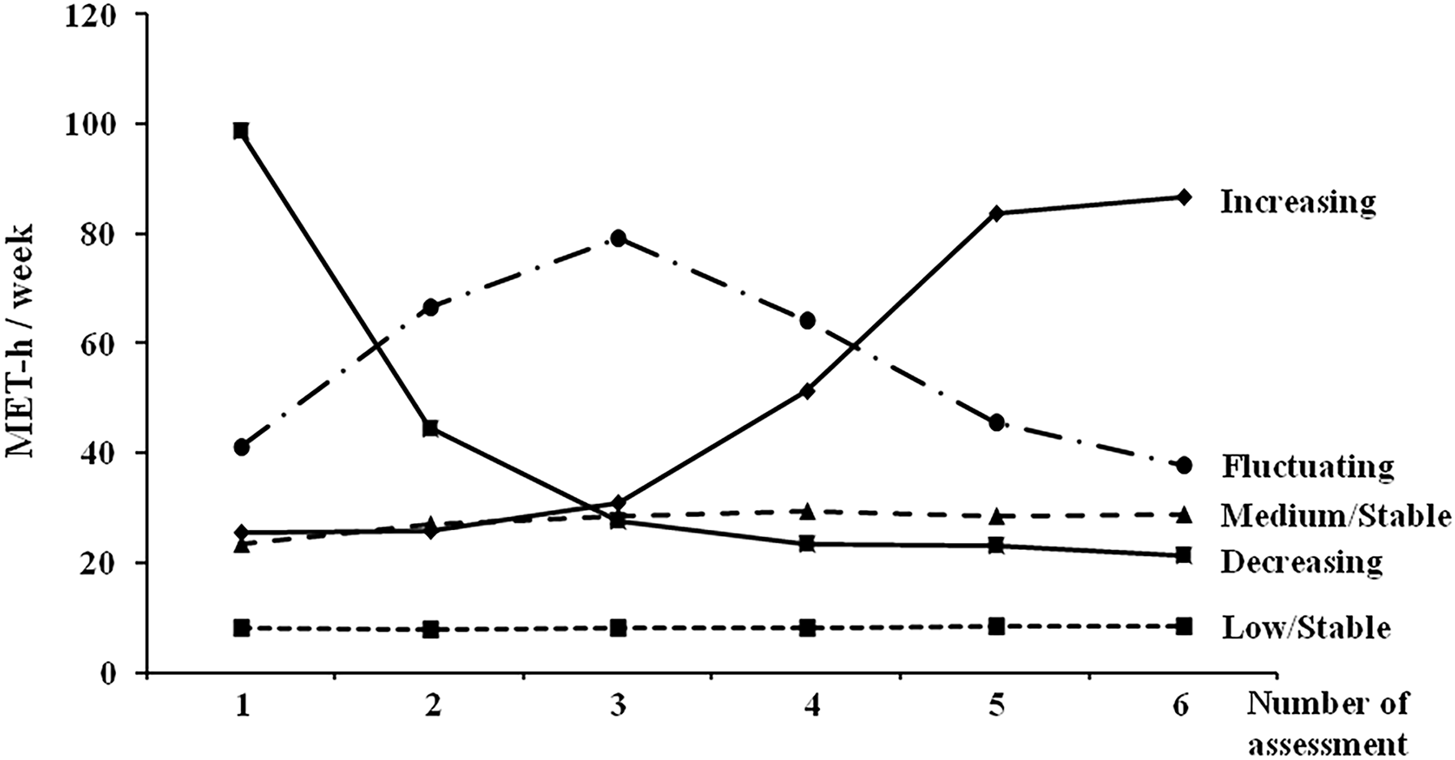
Latent trajectories of leisure-time physical activity levels (MJ cohort, Taiwan, 1996–2014). The time interval between each assessment was at least 1 year. MET, metabolic equivalent.
The study participants were divided into five groups according to percentiles (<20th, 20th–<40th, 40th–<60th, 60th–<80th, ≥80th) of their mean MET-h per week and their trajectories of LTPA (low/stable, medium/stable, increasing, decreasing, and fluctuating, Figure 1), respectively. The primary outcome was all-cause mortality. Data on mortality up to May 2021 were obtained. The associations of quintiles of LTPA and LTPA trajectories with all-cause and cause specific (cardiovascular and cancer) mortality were examined.
All of the statistical analyses were conducted using SAS software (Version 9.4; SAS Institute, Inc., Cary, NC, United States). The statistical significance of the differences in categorical and continuous variables among the LTPA percentiles and LTPA trajectory groups were examined using the Chi-square test and one-way ANOVA, respectively. To examine the associations of LTPA quintiles and LTPA trajectories with all-cause mortality, a Cox-proportional hazard model was used with adjustments for age, sex, body mass index, systolic blood pressure, smoking, history of cardiovascular disease, fasting plasma glucose, total cholesterol, and renal function. For cause-specific mortality, we considered cardiovascular death a competing event for cancer death, and vice versa. We conducted an extended Cox’s proportional hazards model to determine the subdistribution hazard ratio (SHR) [24] of cardiovascular and cancer mortality among the quintiles of LTPA and LTPA trajectory groups. To examine the joint effects of mean levels of LTPA and LTPA trajectories on all-cause and cause-specific mortality, we regrouped the study population according to quintiles of LTPA and LTPA trajectories. In all of the analyses, a two-sided p-value of <0.05 was considered statistically significant.
Results
A total of 21,211 participants were analyzed, and the median follow-up time was 16.8 years. Table 1 shows the baseline characteristics of the study participants according to percentile of their mean MET-h per week during the study period. Participants in the highest quintile were older and more likely to be male, had a higher body mass index and blood pressure, and had a worse lipid profile (higher total and low-density lipoprotein cholesterol and triglyceride, and lower high-density lipoprotein cholesterol) than those in the lower quintiles.
TABLE 1
| Variable (number of participants with miss data) | Percentile of mean MET-h per week | p-value | ||||
|---|---|---|---|---|---|---|
| 20th percentile | 20th–40th percentile | 40th–60th percentile | 60th–80th percentile | ≥80th percentile | ||
| N | 4242 | 4233 | 4249 | 4244 | 4243 | |
| MET-h, per week | 1.84 ± 3.17 | 5.67 ± 5.93 | 10.02 ± 8.94 | 16.05 ± 12.93 | 32.63 ± 27.48 | <0.001 |
| Age, years | 34.8 ± 9.1 | 36.4 ± 10.4 | 38.3 ± 11.4 | 41.6 ± 13.4 | 43.9 ± 14.3 | <0.001 |
| Male, n (%) | 1930 (45.5) | 2134 (50.4) | 2395 (56.4) | 2537 (59.8) | 2767 (65.2) | <0.001 |
| Body mass index, kg/m2 (3) | 22.5 ± 3.7 | 22.8 ± 3.5 | 23.1 ± 3.4 | 23.3 ± 3.3 | 23.5 ± 3.3 | <0.001 |
| Systolic BP, mm Hg (635) | 115 ± 15 | 117 ± 16 | 119 ± 16 | 121 ± 17 | 123 ± 18 | <0.001 |
| Diastolic BP, mm Hg (635) | 69 ± 11 | 70 ± 11 | 72 ± 11 | 73 ± 11 | 74 ± 12 | <0.001 |
| Smoking, n (%) (1495) | 984 (24.3) | 915 (23.1) | 886 (22.5) | 873 (22.5) | 859 (22.1) | 0.136 |
| History of CVD, n (%) (1) | 48 (1.1) | 51 (1.2) | 67 (1.6) | 72 (1.7) | 115 (2.7) | <0.001 |
| FPG, mmol/L (25) | 5.36 ± 0.92 | 5.39 ± 0.90 | 5.45 ± 0.92 | 5.48 ± 0.97 | 5.54 ± 1.01 | <0.001 |
| eGFR, ml/min/1.73 m2 (9) | 88.8 ± 16.2 | 87.2 ± 15.7 | 85.8 ± 18.0 | 84.1 ± 18.4 | 83.2 ± 21.3 | <0.001 |
| Total cholesterol, mmol/L (22) | 4.90 ± 0.88 | 4.92 ± 0.87 | 4.99 ± 0.92 | 5.06 ± 0.94 | 5.09 ± 0.95 | <0.001 |
| LDL cholesterol, mmol/L (1200) | 2.90 ± 0.79 | 2.96 ± 0.78 | 3.02 ± 0.82 | 3.10 ± 0.85 | 3.13 ± 0.86 | <0.001 |
| HDL cholesterol, mmol/L (1125) | 1.46 ± 0.40 | 1.42 ± 0.39 | 1.40 ± 0.39 | 1.38 ± 0.39 | 1.38 ± 0.38 | <0.001 |
| Triglyceride, mmol/L (11) | 1.22 ± 1.04 | 1.24 ± 0.97 | 1.28 ± 1.02 | 1.34 ± 1.05 | 1.30 ± 0.97 | <0.001 |
Baseline characteristics of the study participants according to percentile of mean physical activity levels (MJ cohort, Taiwan, 1996–2014).
Data are presented as mean (95% CI) or n (%). CVD, cardiovascular disease; BP, blood pressure; eGFR, estimated glomerular filtration rate; FPG, fasting plasma glucose; HDL, high-density lipoprotein; LDL, low-density lipoprotein; MET, metabolic equivalent.
Table 2 shows the baseline characteristics according to the study participants’ latent trajectory of LTPA during the study period. Participants with a low/stable trajectory had the lowest mean MET-h per week (8.01 ± 9.60), while those with a decreasing trajectory had the highest mean MET-h per week (98.77 ± 33.99). The two groups were younger, had a lower body mass index and blood pressure, and had a better lipid profile (lower total and low-density lipoprotein cholesterol and triglyceride, and higher high-density lipoprotein cholesterol) than the other three groups.
TABLE 2
| Variable | Latent trajectory of physical activity levels | p-value | ||||
|---|---|---|---|---|---|---|
| Low/Stable | Medium/Stable | Increasing | Decreasing | Fluctuating | ||
| N (%) | 16,100 (75.9%) | 3913 (18.4%) | 436 (2.1%) | 294 (1.4%) | 468 (2.2%) | |
| MET-h, per week | 8.01 ± 9.60 | 23.38 ± 15.87 | 25.53 ± 21.24 | 98.77 ± 33.99 | 41.00 ± 26.62 | <0.001 |
| Age, years | 37.5 ± 11.2 | 44.2 ± 14.1 | 42.8 ± 14.2 | 38.4 ± 14.3 | 44.8 ± 14.0 | <0.001 |
| Male, n (%) | 8469 (52.6) | 2447 (62.5) | 301 (69.0) | 208 (70.8) | 338 (72.2) | <0.001 |
| Body mass index, kg/m2 | 22.9 ± 3.5 | 23.5 ± 3.2 | 23.7 ± 3.7 | 23.0 ± 3.4 | 23.6 ± 3.1 | <0.001 |
| Systolic BP, mm Hg | 118 ± 16 | 123 ± 18 | 122 ± 16 | 121 ± 17 | 123 ± 18 | <0.001 |
| Diastolic BP, mm Hg | 71 ± 11 | 74 ± 11 | 73 ± 12 | 73 ± 11 | 74 ± 12 | <0.001 |
| Smoking, n (%) | 3481 (23.2) | 779 (21.8) | 102 (25.5) | 63 (23.3) | 92 (21.3) | 0.266 |
| History of CVD, n (%) | 224 (1.4) | 96 (2.5) | 10 (2.3) | 8 (2.7) | 15 (3.2) | <0.001 |
| FPG, mmol/L | 5.42 ± 0.93 | 5.54 ± 0.98 | 5.57 ± 0.89 | 5.5 ± 0.98 | 5.57 ± 1.26 | <0.001 |
| eGFR, ml/min/1.73 m2 | 86.6 ± 17.1 | 82.9 ± 19.9 | 86.9 ± 29.7 | 87.0 ± 22.5 | 80.5 ± 18.7 | <0.001 |
| Total cholesterol, mmol/L | 4.96 ± 0.91 | 5.11 ± 0.94 | 5.08 ± 0.91 | 4.94 ± 0.98 | 5.08 ± 0.94 | <0.001 |
| LDL cholesterol, mmol/L | 2.99 ± 0.81 | 3.15 ± 0.85 | 3.11 ± 0.85 | 2.99 ± 0.93 | 3.07 ± 0.81 | <0.001 |
| HDL cholesterol, mmol/L | 1.41 ± 0.40 | 1.37 ± 0.38 | 1.40 ± 0.39 | 1.48 ± 0.36 | 1.41 ± 0.41 | <0.001 |
| Triglyceride, mmol/L | 1.27 ± 1.03 | 1.33 ± 0.98 | 1.28 ± 0.78 | 1.06 ± 0.61 | 1.34 ± 1.20 | <0.001 |
Baseline characteristics of the study participants according to latent trajectory of physical activity levels (MJ cohort, Taiwan, 1996–2014).
Data are presented as mean (95% CI) or n (%). CVD, cardiovascular disease; BP, blood pressure; eGFR, estimated glomerular filtration rate; FPG, fasting plasma glucose; HDL, high-density lipoprotein; LDL, low-density lipoprotein; MET, metabolic equivalent.
During the follow-up period, a total of 960 participants died (morality rate 264.9 per 100,000 person-years). The numbers for cardiovascular and cancer death were 177 and 399, respectively. The associations of baseline characteristics and physical activity levels with all-cause mortality are shown in Supplementary Table S2. Table 3 shows the associations of quintiles of LTPA and distinct LTPA trajectories with all-cause and cardiovascular/cancer mortality. Compared with participants who had the lowest quintile (<20th percentile), only those with the highest quintile (≥80th percentile) had a significantly lower risk of all-cause mortality (HR 0.76, 95% CI 0.58–0.99, p = 0.041) after multivariate adjustment. With regard to LTPA trajectories (using the low/stable trajectory as the reference group), participants with a decreasing trajectory did not have a significantly lower risk of all-cause mortality (HR 0.58, 95% CI 0.27–1.22, p = 0.151) despite having the highest mean MET-h per week. In contrast, participants with a medium/stable (HR 0.84, 95% CI 0.72–0.98, p = 0.031) or an increasing (HR 0.57, 95% CI 0.33–0.97, p = 0.037) trajectory had a significantly lower risk of all-cause mortality, compared with the reference group. Similar findings were noted with respect to cancer mortality.
TABLE 3
| All-cause mortality | Cardiovascular mortality | Cancer mortality | ||||||
|---|---|---|---|---|---|---|---|---|
| Univariate | p | Multivariatea | p | Multivariateb | p | Multivariateb | p | |
| HR (95% CI) | HR (95% CI) | SHR (95% CI) | SHR (95% CI) | |||||
| Percentile | ||||||||
| <20th | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | ||||
| 20th–<40th | 1.10 (0.83–1.46) | 0.495 | 0.84 (0.62–1.15) | 0.271 | 1.39 (0.63–3.06) | 0.410 | 0.79 (0.50–1.23) | 0.291 |
| 40th–<60th | 1.48 (1.14–1.92) | 0.003 | 0.96 (0.72–1.27) | 0.760 | 1.01 (0.47–2.17) | 0.979 | 1.18 (0.79–1.74) | 0.419 |
| 60th–<80th | 2.12 (1.66–2.71) | <0.001 | 0.84 (0.64–1.10) | 0.198 | 0.98 (0.47–2.03) | 0.957 | 0.88 (0.59–1.30) | 0.523 |
| ≥80th | 2.51 (1.97–3.19) | <0.001 | 0.76 (0.58–0.99) | 0.041 | 1.15 (0.57–2.33) | 0.703 | 0.69 (0.46–1.04) | 0.078 |
| Trajectory | ||||||||
| Low/Stable | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | ||||
| Medium/Stable | 1.76 (1.53–2.02) | <0.001 | 0.84 (0.72–0.98) | 0.031 | 1.03 (0.72–1.48) | 0.854 | 0.68 (0.52–0.89) | 0.005 |
| Increasing | 1.14 (0.72–1.79) | 0.588 | 0.57 (0.33–0.97) | 0.037 | 0.82 (0.26–2.54) | 0.729 | 0.71 (0.34–1.51) | 0.377 |
| Decreasing | 0.65 (0.31–1.38) | 0.262 | 0.58 (0.27–1.22) | 0.151 | 1.48 (0.47–4.62) | 0.501 | 0.40 (0.10–1.65) | 0.206 |
| Fluctuating | 2.07 (1.51–2.83) | <0.001 | 0.99 (0.70–1.39) | 0.947 | 1.35 (0.68–2.67) | 0.394 | 1.05 (0.62–1.77) | 0.852 |
Cox proportional hazards models for all-cause and cardiovascular/cancer mortality by percentile of mean physical activity levels and latent trajectory groups (MJ cohort, Taiwan, 1996–2014).
Adjusted for age, sex, body mass index, systolic blood pressure, smoking, history of cardiovascular disease, fasting plasma glucose, estimated glomerular filtration rate, and total cholesterol.
Considering competing risk of mortality in addition to multivariate adjustment. MET, metabolic equivalent; SHR, subdistribution hazard ratio.
Table 4 shows the distribution of study participants by quintiles of LTPA and LTPA trajectories. It is interesting to note that participants with an increasing (group 7), decreasing (group 8), and fluctuating (group 9) trajectory had a mean LTPA level in the highest quintile (≥80th percentile). Nevertheless, their risks of all-cause mortality might be different. Using group 1 as the reference group, the joint effects of mean levels of LTPA and LTPA trajectories on all-cause and cardiovascular/cancer mortality are shown in Table 5. After multivariate adjustment, group 7 (≥80th percentile of LTPA with an increasing trajectory) had a significantly lower risk of all-cause mortality (HR 0.52, 95% CI 0.29–0.92, p = 0.024). A similar finding (HR 0.77, 95% CI 0.59–1.02, p = 0.066) was noted for group 6 (≥80th percentile of LTPA with a medium/stable trajectory).
TABLE 4
| Percentile of mean MET-h | Latent trajectory of physical activity levels | Total | ||||
|---|---|---|---|---|---|---|
| Low/Stable | Medium/Stable | Increasing | Decreasing | Fluctuating | ||
| <20th | 4242 (20.0) (Group 1) | 0 | 0 | 0 | 0 | 4,242 (20.0) |
| 20th–<40th | 4233 (20.0) (Group 2) | 0 | 0 | 0 | 0 | 4,233 (20.0) |
| 40th–<60th | 4249 (20.0) (Group 3) | 0 | 0 | 0 | 0 | 4,249 (20.0) |
| 60th–<80th | 3376 (15.9) (Group 4) | 854 (4.0) (Group 5) | 1 (0.0) | 13 (0.1) | 0 | 4,244 (20.0) |
| ≥80th | 0 | 3059 (14.4) (Group 6) | 435 (2.1) (Group 7) | 281 (1.3) (Group 8) | 468 (2.2) (Group 9) | 4,243 (20.0) |
| Total | 16,100 (75.9) | 3913 (18.5) | 436 (2.1) | 294 (1.4) | 468 (2.2) | 21,211 (100) |
Distribution of study participants by percentile of mean physical activity levels and latent trajectory groups (MJ cohort, Taiwan, 1996–2014).
Data are presented as n (%). MET, metabolic equivalents.
TABLE 5
| Groups | All-cause mortality | Cardiovascular mortality | Cancer mortality | |||||
|---|---|---|---|---|---|---|---|---|
| Univariate | p | Multivariatea | P | Multivariateb | p | Multivariateb | p | |
| HR (95% CI) | HR (95% CI) | SHR (95% CI) | SHR (95% CI) | |||||
| 1: <20th percentile; Low/Stable | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | ||||
| 2: 20th–<40th percentile; Low/Stable | 1.10 (0.83–1.46) | 0.491 | 0.84 (0.62–1.15) | 0.274 | 1.39 (0.64–3.06) | 0.408 | 0.79 (0.50–1.23) | 0.293 |
| 3: 40th–<60th percentile; Low/Stable | 1.48 (1.14–1.92) | 0.003 | 0.96 (0.73–1.27) | 0.769 | 1.01 (0.47–2.17) | 0.977 | 1.18 (0.79–1.74) | 0.417 |
| 4: 60th–<80th percentile; Low/Stable | 2.13 (1.65–2.74) | <0.001 | 0.87 (0.66–1.15) | 0.332 | 0.97 (0.46–2.05) | 0.942 | 0.93 (0.62–1.39) | 0.707 |
| 5: 60th–<80th percentile; Medium/Stable | 2.13 (1.52–3.00) | <0.001 | 0.73 (0.50–1.07) | 0.104 | 1.01 (0.39–2.60) | 0.990 | 0.73 (0.41–1.30) | 0.283 |
| 6: ≥80th percentile; Medium/Stable | 2.66 (2.08–3.40) | <0.001 | 0.77 (0.59–1.02) | 0.066 | 1.11 (0.54–2.30) | 0.771 | 0.66 (0.43–1.01) | 0.055 |
| 7: ≥80th percentile; Increasing | 1.64 (1.00–2.70) | 0.051 | 0.52 (0.29–0.92) | 0.024 | 0.87 (0.24–3.17) | 0.835 | 0.70 (0.31–1.58) | 0.389 |
| 8: ≥80th percentile; Decreasing | 0.98 (0.45–2.11) | 0.954 | 0.53 (0.24–1.16) | 0.111 | 1.58 (0.43–5.78) | 0.491 | 0.40 (0.09–1.72) | 0.218 |
| 9: ≥80th percentile; Fluctuating | 3.00 (2.07–4.35) | <0.001 | 0.90 (0.60–1.35) | 0.602 | 1.43 (0.57–3.59) | 0.442 | 1.03 (0.56–1.90) | 0.917 |
Joint effects of mean physical activity level and physical activity trajectory on all-cause and cardiovascular/cancer mortality (MJ cohort, Taiwan, 1996–2014).
Adjusted for age, sex, body mass index, systolic blood pressure, smoking, history of cardiovascular disease, fasting plasma glucose, estimated glomerular filtration rate, and total cholesterol.
Considering competing risk of mortality in addition to multivariate adjustment. MET, metabolic equivalent; SHR, subdistribution hazard ratio.
Discussion
In this study on a large general population with long-term follow-up, we demonstrated that LTPA trajectories (medium/stable or increasing) were associated with a decrease in all-cause and cancer mortality (Table 3). Although the study participants with LTPA ≥80th percentile had a significantly lower risk of all-cause mortality with a modest decrease in cancer mortality (Table 3), the benefit in survival was only observed in those with a medium/stable (group 6) or increasing (group 7) trajectory of LTPA (Table 5). Our findings highlight the importance of maintaining a stable amount of physical activity, in terms of survival in a general population.
Maintaining a physically active lifestyle has been associated with a lower risk of all-cause mortality. In contrast to most previous studies [7-16, 25] in which levels of physical activity were assessed only at baseline or at two time points, we used several assessments of LTPA to establish latent trajectories of physical activity levels during the study period. This method allowed us to categorize the study population into several groups according to naturally occurring trajectories [23, 26-28] rather than artificially defined cutoff values. Our findings were consistent with previous results [7-16, 25-29] that showed maintaining (medium/stable) or increasing physical activity levels was associated with a lower risk of all-cause mortality. In contrast, those who had decreasing or fluctuating LTPA trajectory did not have a significantly lower risk of mortality (Table 3) despite having a higher mean MET-h per week (Table 2) during the study period. These results indicate that LTPA trajectory is important with regard to the benefit in survival [1, 2] in the general population.
We further examined the joint effects of mean levels of LTPA and LTPA trajectories on all-cause mortality. Although participants who had ≥80th percentile of LTPA in our study had a lower risk of all-cause mortality (adjusted HR 0.76, 95% CI 0.58–0.99, p = 0.041, Table 3), the benefit was only observed in those who also had an increasing LTPA trajectory (group 7 in Tables 4, 5). Group 5, group 6, and group 8 had a modest, but non-significant, decrease in all-cause mortality risk compared with the least active group (group 1, Tables 4, 5). It is interesting to note that group 8 (281 of 294 participants with a decreasing LTPA trajectory) had a mean MET-h per week of about 100 (Table 2). The values in group 5/group6 and group 7 were around 23 and 25, respectively. These findings support the notion that maintaining an active lifestyle confers a survival advantage. Similar to our findings, a previous cohort study reported that a change from being active at baseline to being sedentary during follow-up in women aged 65 years or older was associated with a similar risk of all-cause mortality compared with those who stayed sedentary [7].
The decrease of all-cause mortality risk in the medium/stable and increasing LTPA trajectory was likely due to a lower risk of cancer mortality, rather than cardiovascular mortality (Table 3). This finding was similar to some previous studies [30-32], although there were inconsistent results [33-35]. In the aforementioned studies [30-35], cancer mortality was not considered a competing event for cardiovascular mortality (and vice versa) [24]. This may help explain the inconsistent findings. Since cancer and cardiovascular diseases share common risk factors (such as obesity, sedentary lifestyle, diabetes) [36], it is not surprising that maintaining physical activity was associated with a lower risk of either cardiovascular or cancer mortality. We speculate that the non-significantly lower risk of cardiovascular and cancer mortality in our study participants with an increasing LTPA trajectory might be due to the relatively small sample size. The decrease in cancer mortality risk in the study population with a medium/stable LTPA trajectory supports previous findings [30-32], and underlines the importance of adopting a healthy lifestyle in reducing cancer mortality [37], which has become one of the main causes of death worldwide [38].
This study has some limitations. First, this was a cohort study rather than a randomized controlled trial. Although we adjusted for multiple relevant variables in the statistical models, we cannot exclude the possibility that our findings were confounded by between-group differences in baseline characteristics. Nevertheless, long-term follow-up is needed to investigate the effects of physical activity on mortality risk. There would likely be considerable variation among study participants in the persistence of physical activity over time. Hence, randomizing study participants to different levels of physical activity for a long period of time might be impractical. As the persistence of physical activity is important in terms of its effects on outcomes [14-16, 25-29], our method of establishing latent physical activity trajectories [17-18, 23] could help address this issue despite its limitations. Second, data on LTPA were collected through self-reported questionnaires. We analyzed data from participants with more than 5 LTPA assessments within an 8-year period to establish the latent trajectories of LTPA. We acknowledge that there might have been bias in the information collected through questionnaires, and this issue should be taken into account when interpreting our results.
In conclusion, using data from a large cohort with long-term follow-up, we demonstrated that a medium/stable or increasing LTPA trajectory was independently associated with a lower risk of all-cause mortality in a general population. The association was independent of mean levels of LTPA during the study period. Our findings suggest that promotion of maintaining a stable LTPA level in a general population is benefit for public health and survival.
Statements
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Review Board of Taichung Veterans General Hospital, Taichung, Taiwan. The patients/participants provided their written informed consent to participate in this study.
Author contributions
C-LL and J-SW designed and conducted the research; C-LL, C-HC, and W-JL analyzed data; C-LL and J-SW wrote the first draft of the manuscript; and C-HC and W-JL revised the manuscript critically for important intellectual content. All authors approved the final draft of the manuscript.
Funding
The authors declare that this study received funding from Taichung Veterans General Hospital, Taichung, Taiwan (TCVGH-1093504C, TCVGH-1097316C, TCVGH-1097327D, TCVGH-1103502C, and TCVGH-1113502C). The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Conflict of interest
The authors declare that they do not have any conflicts of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2023.1605332/full#supplementary-material
References
1
Li Y Pan A Wang DD Liu X Dhana K Franco OH et al Impact of Healthy Lifestyle Factors on Life Expectancies in the US Population. Circulation (2018) 138:345–55. 10.1161/CIRCULATIONAHA.117.032047
2
Barone Gibbs B Hivert MF Jerome GJ Kraus WE Rosenkranz SK Schorr EN et al American Heart Association Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular and Stroke Nursing; and Council on Clinical Cardiology. Physical Activity as a Critical Component of First-Line Treatment for Elevated Blood Pressure or Cholesterol: Who, what, and How?: A Scientific Statement from the American Heart Association. Hypertension (2021) 78:e26–37. 10.1161/HYP.0000000000000196
3
Lee IM Shiroma EJ Lobelo F Puska P Blair SN Katzmarzyk PT et al Effect of Physical Inactivity on Major Non-communicable Diseases Worldwide: an Analysis of burden of Disease and Life Expectancy. Lancet (2012) 380:219–29. 10.1016/S0140-6736(12)61031-9
4
Katzmarzyk PT Mason C . The Physical Activity Transition. J Phys Act Health (2009) 6:269–80. 10.1123/jpah.6.3.269
5
Brownson RC Boehmer TK Luke DA . Declining Rates of Physical Activity in the United States: what Are the Contributors?Annu Rev Public Health (2005) 26:421–43. 10.1146/annurev.publhealth.26.021304.144437
6
Olshansky SJ Passaro DJ Hershow RC Layden J Carnes BA Brody J et al A Potential Decline in Life Expectancy in the United States in the 21st century. N Engl J Med (2005) 352:1138–45. 10.1056/NEJMsr043743
7
Gregg EW Cauley JA Stone K Thompson TJ Bauer DC Cummings SR et al Relationship of Changes in Physical Activity and Mortality Among Older Women. JAMA (2003) 289:2379–86. 10.1001/jama.289.18.2379
8
Talbot LA Morrell CH Fleg JL Metter EJ . Changes in Leisure Time Physical Activity and Risk of All-Cause Mortality in Men and Women: the Baltimore Longitudinal Study of Aging. Prev Med (2007) 45:169–76. 10.1016/j.ypmed.2007.05.014
9
Wen CP Wai JP Tsai MK Yang YC Cheng TY Lee MC et al Minimum Amount of Physical Activity for Reduced Mortality and Extended Life Expectancy: a Prospective Cohort Study. Lancet (2011) 378:1244–53. 10.1016/S0140-6736(11)60749-6
10
Moore SC Patel AV Matthews CE Berrington de Gonzalez A Park Y Katki HA et al Leisure Time Physical Activity of Moderate to Vigorous Intensity and Mortality: a Large Pooled Cohort Analysis. Plos Med (2012) 9:e1001335. 10.1371/journal.pmed.1001335
11
Chudasama YV Khunti KK Zaccardi F Rowlands AV Yates T Gillies CL et al Physical Activity, Multimorbidity, and Life Expectancy: a UK Biobank Longitudinal Study. BMC Med (2019) 17:108. 10.1186/s12916-019-1339-0
12
Matthews CE Keadle SK Troiano RP Kahle L Koster A Brychta R et al Accelerometer-measured Dose-Response for Physical Activity, Sedentary Time, and Mortality in US Adults. Am J Clin Nutr (2016) 104:1424–32. 10.3945/ajcn.116.135129
13
Liu Y Shu XO Wen W Saito E Rahman MS Tsugane S et al Association of Leisure-Time Physical Activity with Total and Cause-specific Mortality: a Pooled Analysis of Nearly a Half Million Adults in the Asia Cohort Consortium. Int J Epidemiol (2018) 47:771–9. 10.1093/ije/dyy024
14
Balboa-Castillo T Guallar-Castillón P León-Muñoz LM Graciani A López-García E Rodríguez-Artalejo F . Physical Activity and Mortality Related to Obesity and Functional Status in Older Adults in Spain. Am J Prev Med (2011) 40:39–46. 10.1016/j.amepre.2010.10.005
15
Petersen CB Grønbæk M Helge JW Thygesen LC Schnohr P Tolstrup JS . Changes in Physical Activity in Leisure Time and the Risk of Myocardial Infarction, Ischemic Heart Disease, and All-Cause Mortality. Eur J Epidemiol (2012) 27:91–9. 10.1007/s10654-012-9656-z
16
Dwyer T Pezic A Sun C Cochrane J Venn A Srikanth V et al Objectively Measured Daily Steps and Subsequent Long Term All-Cause Mortality: The Tasped Prospective Cohort Study. PLoS One (2015) 10:e0141274. 10.1371/journal.pone.0141274
17
Nagin DS Odgers CL . Group-based Trajectory Modeling in Clinical Research. Ann Rev Clin Psychol (2010) 6:109–38. 10.1146/annurev.clinpsy.121208.131413
18
Nagin DS Odgers CL . Group-Based Trajectory Modeling (Nearly) Two Decades Later. J Quant Criminol (2010) 26:445–53. 10.1007/s10940-010-9113-7
19
Wu X Tsai SP Tsao CK Chiu ML Tsai MK Lu PJ et al Cohort Profile: The Taiwan MJ Cohort: Half a Million Chinese with Repeated Health Surveillance Data. Int J Epidemiol (2017) 46:1744–g. 10.1093/ije/dyw282
20
Martinez-Gomez D Esteban-Cornejo I Lopez-Garcia E García-Esquinas E Sadarangani KP Veiga OL et al Physical Activity Less Than the Recommended Amount May Prevent the Onset of Major Biological Risk Factors for Cardiovascular Disease: a Cohort Study of 198 919 Adults. Br J Sports Med (2020) 54:238–44. 10.1136/bjsports-2018-099740
21
Carlson SA Densmore D Fulton JE Yore MM Kohl HW 3rd . Differences in Physical Activity Prevalence and Trends from 3 U.S. Surveillance Systems: NHIS, NHANES, and BRFSS. J Phys Act Health (2009) 6(1):S18–27. 10.1123/jpah.6.s1.s18
22
Andruff H Carraro N Thompson A Gaudreau P Louvet B . Latent Class Growth Modelling: a Tutorial. Tutorials Quant Methods Psychol (2009) 5:11–24. 10.20982/tqmp.05.1.p011
23
Mori M Krumholz HM Allore HG . Using Latent Class Analysis to Identify Hidden Clinical Phenotypes. JAMA (2020) 324:700–1. 10.1001/jama.2020.2278
24
Dignam JJ Zhang Q Kocherginsky M . The Use and Interpretation of Competing Risks Regression Models. Clin Cancer Res (2012) 18:2301–8. 10.1158/1078-0432.CCR-11-2097
25
Huang Y Jiang C Xu L Zhang W Zhu F Jin Y et al Mortality in Relation to Changes in Physical Activity in Middle-Aged to Older Chinese: An 8-year Follow-Up of the Guangzhou Biobank Cohort Study. J Sport Health Sci (2021) 10:430–8. 10.1016/j.jshs.2020.08.007
26
Mok A Khaw KT Luben R Wareham N Brage S . Physical Activity Trajectories and Mortality: Population Based Cohort Study. BMJ (2019) 365:l2323. 10.1136/bmj.l2323
27
Saint-Maurice PF Coughlan D Kelly SP Keadle SK Cook MB Carlson SA et al Association of Leisure-Time Physical Activity across the Adult Life Course with All-Cause and Cause-specific Mortality. JAMA Netw Open (2019) 2:e190355. 10.1001/jamanetworkopen.2019.0355
28
Aggio D Papachristou E Papacosta O Lennon LT Ash S Whincup P et al Trajectories of Physical Activity from Midlife to Old Age and Associations with Subsequent Cardiovascular Disease and All-Cause Mortality. J Epidemiol Community Health (2020) 74:130–6. 10.1136/jech-2019-212706
29
Byberg L Melhus H Gedeborg R Sundström J Ahlbom A Zethelius B et al Total Mortality after Changes in Leisure Time Physical Activity in 50 Year Old Men: 35 Year Follow-Up of Population Based Cohort. Br J Sports Med (2009) 43:482. 10.1136/bmj.b688
30
Willey JZ Moon YP Sherzai A Cheung YK Sacco RL Elkind MS . Leisure-time Physical Activity and Mortality in a Multiethnic Prospective Cohort Study: the Northern Manhattan Study. Ann Epidemiol (2015) 25:475–9. 10.1016/j.annepidem.2015.04.001
31
Arem H Moore SC Park Y Ballard-Barbash R Hollenbeck A Leitzmann M et al Physical Activity and Cancer-specific Mortality in the NIH-AARP Diet and Health Study Cohort. Int J Cancer (2014) 135:423–31. 10.1002/ijc.28659
32
Li T Wei S Shi Y Pang S Qin Q Yin J et al The Dose-Response Effect of Physical Activity on Cancer Mortality: Findings from 71 Prospective Cohort Studies. Br J Sports Med (2016) 50:339–45. 10.1136/bjsports-2015-094927
33
Gunnell AS Knuiman MW Divitini ML Cormie P . Leisure Time Physical Activity and Long-Term Cardiovascular and Cancer Outcomes: the Busselton Health Study. Eur J Epidemiol (2014) 29:851–7. 10.1007/s10654-014-9963-7
34
Cheung YK Moon YP Kulick ER Sacco RL Elkind MS Willey JZ . Leisure-Time Physical Activity and Cardiovascular Mortality in an Elderly Population in Northern Manhattan: A Prospective Cohort Study. J Gen Intern Med (2017) 32:168–74. 10.1007/s11606-016-3884-y
35
Bennett DA Du H Clarke R Guo Y Yang L Bian Z et al Association of Physical Activity with Risk of Major Cardiovascular Diseases in Chinese Men and Women. JAMA Cardiol (2017) 2:1349–58. 10.1001/jamacardio.2017.4069
36
Koene RJ Prizment AE Blaes A Konety SH . Shared Risk Factors in Cardiovascular Disease and Cancer. Circulation (2016) 133:1104–14. 10.1161/CIRCULATIONAHA.115.020406
37
Molina-Montes E Ubago-Guisado E Petrova D Amiano P Chirlaque MD Agudo A et al The Role of Diet, Alcohol, BMI, and Physical Activity in Cancer Mortality: Summary Findings of the EPIC Study. Nutrients (2021) 13:4293. 10.3390/nu13124293
38
Global Burden of Disease 2019 Cancer Collaboration, KocarnikJMComptonKDeanFEFuWGawBLHarveyJDet alCancer Incidence, Mortality, Years of Life Lost, Years Lived with Disability, and Disability-Adjusted Life Years for 29 Cancer Groups from 2010 to 2019: A Systematic Analysis for the Global Burden of Disease Study 2019. JAMA Oncol (2022) 8:420–44. 10.1001/jamaoncol.2021.6987
Summary
Keywords
mortality, trajectory, physical activity, metabolic equivalent, population
Citation
Lee C-L, Liu W-J, Chen C-H and Wang J-S (2023) Associations of Long-Term Physical Activity Trajectories With All-Cause Mortality in a General Population. Int J Public Health 68:1605332. doi: 10.3389/ijph.2023.1605332
Received
21 August 2022
Accepted
06 January 2023
Published
16 January 2023
Volume
68 - 2023
Edited by
Milo Puhan, University of Zurich, Switzerland
Reviewed by
Ossi Rahkonen, University of Helsinki, Finland
Updates
Copyright
© 2023 Lee, Liu, Chen and Wang.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jun-Sing Wang, jswang@vghtc.gov.tw
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.