Abstract
Objectives: We report results of a systematic review on the health effects of long-term traffic-related air pollution (TRAP) and diabetes in the adult population.
Methods: An expert Panel appointed by the Health Effects Institute conducted this systematic review. We searched the PubMed and LUDOK databases for epidemiological studies from 1980 to July 2019. TRAP was defined based on a comprehensive protocol. Random-effects meta-analyses were performed. Confidence assessments were based on a modified Office for Health Assessment and Translation (OHAT) approach, complemented with a broader narrative synthesis. We extended our interpretation to include evidence published up to May 2022.
Results: We considered 21 studies on diabetes. All meta-analytic estimates indicated higher diabetes risks with higher exposure. Exposure to NO2 was associated with higher diabetes prevalence (RR 1.09; 95% CI: 1.02; 1.17 per 10 μg/m3), but less pronounced for diabetes incidence (RR 1.04; 95% CI: 0.96; 1.13 per 10 μg/m3). The overall confidence in the evidence was rated moderate, strengthened by the addition of 5 recently published studies.
Conclusion: There was moderate evidence for an association of long-term TRAP exposure with diabetes.
Introduction
Diabetes is a major metabolic disease characterized by persistent hyperglycemia if untreated [1]. According to the International Diabetes Federation (IDF), 537 million adults are living with diabetes worldwide with an estimated 45% who are undiagnosed. By 2045, 783 million adults are projected to have diabetes. The most common form of diabetes, type 2, accounts for approximately 90% of cases. Type 2 diabetes is characterized by insulin resistance, a diminished response to insulin of cells in the muscles, liver and fat [2]. Apart from genetic factors that contribute to diabetes risk, the most familiar risk factors include behaviors such as lack of physical activity and diet. Environmental exposures, such as air pollution are also expected to play a role [3].
In 2019, 19.9% of diabetes-related deaths and 19.6% of the diabetes-related disability-adjusted life-years (DALY) were attributed to particulate air pollution [4]. Several systematic reviews have concluded that ambient air pollution is associated with diabetes mellitus [5, 6], diabetes type 1 [7] or gestational diabetes mellitus [8]. Understanding how diabetes risk is affected by air pollution from specific sources informs useful air quality policies and other interventions. Automotive vehicular traffic is a prevalent source of air pollution, especially in cities. In animal studies, traffic-related air pollution (TRAP) was shown to elicit oxidative stress and subclinical inflammation, resulting in impaired insulin signaling and insulin resistance [9]. The sole systematic review to date evaluating the association of TRAP exposure with diabetes concluded there was a positive association between the two [10]. TRAP is a complex mixture and includes tailpipe and non-tailpipe emissions. Tailpipe emissions, from combustion of fossil fuels, contain particulate matter (PM), particularly as elemental carbon (EC) or soot, and nitrogen oxides. Non-tailpipe emissions originate from brake, tire, and road surface abrasion, and re-suspension of dust [11] and include PM trace metals such as copper (Cu), iron (Fe) and zinc (Zn). In high-income countries, non-tailpipe emissions comprise over half of the PM from traffic [12].
The Health Effects Institute (HEI) appointed an expert Panel to systematically evaluate the epidemiological evidence on the associations between TRAP and selected health outcomes including mortality, respiratory diseases, birth outcomes, and cardiometabolic health effects including diabetes. The resulting HEI Special Report was published in 2022 [13], along with a short communication paper of the main findings [14].
Here, we elaborate in depth on the findings and confidence assessment on TRAP in relation to effects on diabetes in adults, and in supplemental analyses we extend our interpretation to include evidence published after completion of the original literature search.
Methods
The 2022 review was led by an expert Panel of 13 experts in environmental sciences, epidemiology, exposure assessment and statistics, supported by an external team and HEI staff. We used a systematic approach to search and select the literature for inclusion in the review, assess study quality, summarize results, and assess the confidence in the association between TRAP and diabetes. The methods were based on standards set by Cochrane Collaboration [15], the World Health Organization [16], and the National Institute of Environmental Health Sciences Office of Health Assessment and Translation (NIEHS OHAT) [17] and are described in more detail in the special report [13]. The protocol was published [18] and registered in PROSPERO 2019 CRD42019150642 available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42019150642.
Exposure Framework for TRAP
Pollutants emitted by motorized traffic are also emitted by other (combustion) sources. A novel framework to formalize the process of determining whether the air pollution exposure contrast in a study was dominated by traffic, we developed a novel framework [18]. In brief, the framework combined three aspects of TRAP assessment and results from a study had to entail all three aspects to be included: 1) Included studies used measures of defined traffic-related pollutants and/or indirect traffic measures, such as distance to major roads or traffic density. Eligible pollutants were NO2, NOx, NO, carbon monoxide (CO), EC (including related metrics such as black carbon, black smoke, and PM absorbance), ultrafine particles (UFP), non-tailpipe PM trace metals [e.g., copper (Cu), iron (Fe) and Zinc (Zn)], polycyclic aromatic hydrocarbons (PAHs), benzene, PM10, PM2.5 and PMcoarse (Supplementary Table S1). 2) Both the pollution surface and participants’ addresses in the included studies had to meet the framework’s thresholds for spatial resolution (e.g., 5 km grid). 3) Eligible exposure assessment methods included appropriate models or surface monitoring at sufficient spatial resolutions (Supplementary Table S2).
Following this framework, we excluded studies on short-term (minutes to months) effects or self-reported exposures to TRAP. We included studies that assigned individual-level exposure based on models exploiting within-city (i.e., neighborhood) contrasts, that were considered to stem primarily from traffic. Studies that exclusively used between-city contrasts were excluded. In general, the larger the study area, the less likely a measured or modelled contrast in pollution stems primarily from traffic emissions. Therefore, epidemiological studies in larger regions (e.g., state- or country-wide studies) were only included when they adjusted for area in their analysis. PM is generally not specific to traffic. We included results pertaining to PM measures (aerodynamic diameter ≤10 µm [PM10] or ≤2.5 µm [PM2.5]) in certain settings, e.g., urban areas, so long as they met more stringent requirements for inclusion. For example, PM studies based exclusively on surface monitoring were excluded, but studies using chemical transport models, dispersion models or land-use regression models with a resolution finer or equal to 5 km were included.
To specify how well the studies met the multiple criteria of the exposure framework, we defined an indicator for high traffic specificity based on even stricter criteria. We used this indicator for sensitivity analyses. High traffic specificity was mainly assigned to models with finer resolution (<1 km) or PM models considering only traffic-specific sources/emissions also with a resolution <1 km.
We converted effect estimates for pollutants expressed as ppb or ppm to μg/m³, or mg/m³ using standard WHO scaling factors (standardization of units). For example, 1 ppb NO2 = 1.88 μg/m³, assuming an ambient pressure of 1 atm and a temperature of 25°C [19]. Effect estimates for black carbon (BC), black smoke (BS) and PM2.5 absorption (soot) were converted into EC-equivalent estimates [20, 21].
Search Strategy
We performed a systematic literature search in PubMed and the specialized LUDOK (Literature database and services on Health Effects of Ambient Air Pollution https://www.swisstph.ch/en/projects/ludok/datenbanksuche/) database matching the PECOS (Population, Exposure, Comparator, Outcome and Study) question [15] for epidemiologic studies:
“In the adult population (P), what is the increase in risk of prevalence and incidence of diabetes (O) per unit increase (C) of long-term exposure to traffic-related air pollution (E), observed in studies relevant for the health outcome and exposure duration of interest (S).”
We searched the databases from 1 January 1980 through 31 July 2019. This end date was chosen a priori for the comprehensive HEI special report comprising dozens of exposures and health outcomes. The search strategy was based on a review protocol developed by the NIEHS OHAT (OHAT) and further refined using a combination of medical subheadings (MeSH) and keywords (Supplementary Table S3). The search strategy was supplemented with hand-searches of references in recent reviews. These were identified by the original search, an additional search in the LUDOK database or individual bibliographic databases curated by HEI and Panel members.
Eligibility Criteria
We applied the following inclusion and exclusion criteria according to the predefined PECOS statement. Studies needed to be published in English in a peer-reviewed journal.
Population
We included studies reporting on the general human adult population, aged 18 and older, from all geographical areas were included. We excluded studies reporting on occupational exposure or exclusively indoor settings as they would be difficult to compare with general population outdoor exposures.
Exposure
Studies that assessed long-term exposure (months to years) to TRAP as defined in the exposure framework were included.
Comparator
Studies analyzing health effects of TRAP either on a continuous scale or in exposure categories and reporting a quantitative measure of association plus a measure of precision were included.
Outcome
Eligible studies evaluated the incidence or prevalence of diabetes, and defined diabetes as fasting blood glucose levels above a threshold, self-reported physician-diagnosed diabetes, clinical diagnosis (ICD-9: 250, ICD-10: E10–E14) in medical records or claims, or the use of blood glucose-lowering medication.
Study Design
We included original epidemiologic studies with individual level data adopting a cohort, case–cohort, case–control, cross-sectional, or intervention design.
We excluded studies that: analyzed only area-level data, evaluated effects of short-term exposure (e.g., time-series or case cross-over studies), reported only unadjusted results, showed clear evidence of an analytical error, were strictly methodological of focused on gene-environment interactions.
Study Selection
We used DistillerSR, a web–based, systematic review software program version 2.29.8 [22], for screening, data extraction and risk of bias assessment. Initial screening based on title and abstract was done by two independent reviewers. Secondary screenings of study eligibility, especially regarding the exposure criterion, were conducted by two independent reviewers based on the full-text, supplements and related exposure assessment papers. At this full-text review stage, the reviewers documented reasons for excluding any given study (Supplementary Table S4). Any disagreement on inclusion was resolved by discussion.
Risk of Bias
We assessed risk of bias (RoB) in the estimation of all exposure–outcome associations that were included in the meta-analyses. We used a modified version of the tool developed for the risk of bias assessment in systematic reviews for the WHO Air Quality Guidelines [16, 23]. In brief, the risk of bias tool guides the assessment of each study’s potential for bias from six domains and related subdomains of systematic error sources: 1) confounding; 2) selection bias; 3) exposure assessment; 4) outcome measurement; 5) missing data; and 6) selective reporting. Most domains have subdomains. The risk of bias for each subdomain and for each domain overall was given a rating of low, moderate or high. No summary classification was derived across the domains.
Meta-Analysis
We conducted meta-analysis for each exposure-outcome pair where three or more studies reported results; we separately analysed findings from incidence and prevalence studies. Effect estimates from single-pollutant models were selected for the meta-analysis. For presenting results on each pollutant, we applied a uniform pollutant contrast to all contributing estimates and the resulting meta-analytic summary estimate (e.g., RR per 10 μg/m3 increment in NO2), which necessitated converting some contributing estimates (see Supplementary Eq. S1). We chose the contrast of a given pollutant to reflect a realistic range of exposures in most studies, by using the pollutant concentration increments from a large European ESCAPE study [24]. Meta-analysis was not conducted for the exposure metrics related to distance and density of traffic, because the varying definitions across the studies precluded such analyses. We computed summary effect estimates with random effects models, using restricted maximum likelihood to estimate the between study variance [25]. Random effects models were chosen a priori because of the expected differences in effect estimates related to differences in populations and pollution mixtures. Statistical heterogeneity was assessed using primarily I2, where I2 values of <50% were interpreted as low; between 50% and 75% as moderate; and >75% as high degree of heterogeneity [26]. The risk estimates hazard ratio (HR), relative risk (RR), incidence rate ratio (IRR) and odds ratio (OR) were considered to approximate the risk ratio [27] and were therefore analysed together as done previously [28]. We use the general term RR to indicate any of the ratio measures.
If a sufficient number of studies were available, we performed additional meta-analyses to assess consistency of the association by: geographic regions; level of risk of bias (selection bias, missing data, confounding, exposure assessment, outcome assessment); smoking adjustment; traffic specificity; and adjustment for the co-exposure noise. All analyses and plots were done with the statistical program R (version 3.6.0), using the libraries “metafor” (v.2.4‐0), “meta,” (v. 4.16‐2), “forestplot” (v.1.10.1), “ggplot” (v. 3.3.3).
Assessment of the Evidence
We assessed: 1) the quality of the body of evidence using a modified OHAT protocol [17], which itself is based on the GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach; and 2) the confidence in an association between TRAP and diabetes in a “narrative” assessment. These complementary methods are described fully in the HEI Special Report, Additional Materials 5.3 [13]. We also reflect on the confidence assessment in a separate paper (under review).
For studies included in meta-analyses, we conducted the quality assessments separately for each pollutant and study design. Starting with a confidence rating depending on study design (moderate for cohort studies and low for cross-sectional studies), the rating was then downgraded for factors that decrease confidence (high RoB, unexplained inconsistency, imprecision, and publication bias) and upgraded for factors that increase confidence in the body of evidence (monotonic exposure-response, consistency across populations, and consideration of residual confounding). We did not consider the downgrading factor “indirectness” because we included only studies of human exposure to TRAP in direct association with diabetes. Furthermore, we did not use the upgrading factor “large magnitude of effect,” because this factor was unlikely to be meaningful. This a priori decision was based on experiences in the WHO systematic reviews of air pollution, where large or very large effect sizes (i.e., large RR > 2 or very large RR > 5 as defined in OHAT) never occurred [30, 31]. Large RRs were also not observed in our review (Supplementary Figure S1). Next, evaluations per pollutant were combined across study designs, and then across pollutants which was informed by the pollutant with the highest rating.
Since the OHAT assessment is geared toward studies entering a meta-analysis and focusses on the quality of the body of evidence rather than the presence of an association, the Panel also conducted a more inclusive “narrative” assessment. This additionally considered, e.g., pollutants with less than three studies reporting results or those studying indirect traffic measures. While many of the same aspects relevant to evidence synthesis were included in both assessments, there were some subtle differences, most notably regarding the magnitude and direction of the association, and the consistency across pollutants and indirect traffic measures.
In both assessments we rated the level of confidence as high, moderate, low or very low. The two approaches were considered complementary and combined into an overall confidence assessment.
Updated Search and Supplemental Analyses
To interpret results of our original review (indicated in tables and figures as “Global 2022”) in light of evidence published after the ending date of this review’s literature search, we repeated the search for eligible studies, starting from June 2019 up to May 2022. Studies identified in this new search were not incorporated into the risk of bias and confidence assessment. However, we incorporated their findings into supplemental meta-analyses to investigate the robustness of our original meta-analytic results to the inclusion of recently published evidence (indicated in tables and figures as “Global 2023”).
Results
Study Selection
The search strategy for all health outcomes considered for the comprehensive review yielded 13,660 unique articles. After initial screening, exclusion of studies not meeting the inclusion criteria, and restricting to articles on diabetes outcomes, we identified 45 studies, 21 of which entered this review after full-text assessment (Table 1, Supplementary Figure S2: PRISMA flow chart). Most studies were excluded, because the spatial scale of the pollution surface or participants’ address did not meet the criteria (Supplementary Table S4).
TABLE 1
| References | Study name | Location | Study period | Study design in analysis | Sample size N (% women) | Age at baseline | Ascertainment of diabetes | Confounder adjusted for | Results (estimatea, 95% CI, increment) |
|---|---|---|---|---|---|---|---|---|---|
| [45] | DDCH | Copenhagen and Aarhus, Denmark | 1993–2006 | Cohort | 51,818 (53%) | 56 | Disease register | Age, sex, iSES, smoking, behaviorb, BMI | Incidence |
| NO2 1.04 (1.00, 1.08) per 4.9 μg/m3c | |||||||||
| NOx 1.02 (1.00, 1.04) per 11.4 μg/m3c | |||||||||
| Distance 1.07 (0.95, 1.21) <50 vs. >50 m | |||||||||
| Density 1.02 (1.00, 1.04) per 1,200 vehicle-km/day | |||||||||
| [40] | ONPHEC | Toronto, Canada | 1996–2012 | Cohort | 1,056,012 (53%) | 51 | Administrative data from hospital and insurance registries | Age, sex, nSES, comorbiditiesd | IncidenceNO2 1.06 (1.05, 1.07) per 4.0 ppbcPNC 1.06 (1.05, 1.08) per 9948.4 particles/cm3 |
| [41] | British Columbia Diabetes Cohort | Vancouver, British Columbia, Canada | 1994–2002 | Cohort | 380,738 (54%) | 58 | Administrative data from insurance registry | Age, sex, nSES | Incidence |
| NO2 1.00 (0.98, 1.02) per 8.4 μg/m3c | |||||||||
| NO 1.04 (1.01, 1.05) per 13.13 μg/m3 | |||||||||
| PM2.5abs 1.03 (1.01, 1.04) per 0.9 1e-5/mc | |||||||||
| PM2.5 1.03 (1.01, 1.05) per 1.6 μg/m3c | |||||||||
| [35] | BWHS | Los Angeles, California, United States | 1995–2005 | Cohort | 39,922 (100%) | 39 | Doctor-diagnosed | Age, iSES, nSES, smoking, behavior, BMI, familial diabetes | IncidenceNOx 1.25 (1.07, 1.46) per 12.4 ppbc |
| [36] | BWHS | United States | 1995–2013 | Cohort | 430,032 (100%) | 39 | Doctor-diagnosed | Age, iSES, nSES, smoking, behavior, BMI, area, questionnaire cycle | IncidenceNO2 0.90 (0.82, 1.00) per 9.7 ppbc |
| [63] | Hoorn Diabetes Screening | West Friesland, Netherlands | 1998–2000 | Cross sectional | 8018 (51%) | Range: 50–75 | Multimodale | Age, sex, nSES, (BMI)f | Prevalence |
| NO2 1.03 (0.82, 1.31) 14.2–15.2 vs. 8.8–14.2 μg/m3 | |||||||||
| NO2 1.25 (0.99, 1.56) 15.2–16.5 vs. 8.8–14.2 μg/m3 | |||||||||
| NO2 0.80 (0.63, 1.02) 16.5–26 vs. 8.8–14.2 μg/m3 | |||||||||
| Distance 0.88 (0.70, 1.13) 2–74 vs. 220–1,610 m | |||||||||
| Distance: 1.17 (0.93, 1.48) 74–140 vs. 220–1,610 m | |||||||||
| Distance: 1.12 (0.88, 1.42) 140–220 vs. 220–1,610 m | |||||||||
| Density: 1.09 (0.85, 1.38) 882–2007 vs. 63–516 thousand vehicles/day | |||||||||
| Density: 1.13 (0.89, 1.44) 680–882 vs. 63–516 thousand vehicles/day | |||||||||
| Density: 1.25 (0.99, 1.59) 516–680 vs. 63–516 thousand vehicles/day | |||||||||
| [44] | Plovdiv Diabetes Survey | Plovdiv, Bulgaria | 2014–2014 | Cross sectional | 513 (61%) | 36 | Doctor-diagnosed | Age, sex, iSES, smoking, behavior, BMI, familial diabetes, noise | PrevalencePM2.5 1.32 (0.28, 6.24) >25 vs. <25 μg/m3PAH (BaP) 1.76 (0.52, 5.98) >6 vs. <6 ng/m3 |
| [34] | SAPALDIA | Multiple cities, Switzerland | 2002–2002 | Cross sectional | 6,392 (52%) | 52 | Multimodal | Age, sex, iSES, nSES, smoking, behavior, BMI, area | PrevalenceNO2 1.21 (1.05, 1.39) per 10 μg/m3cPM10 1.44 (1.21, 1.71) per 10 μg/m3c |
| [33] | SAPALDIA | Multiple cities, Switzerland | 2002–2011 | Cohort | 2,631 (52%) | 53 | multimodal | Age, sex, iSES, nSES, smoking, behavior, BMI, area | IncidenceNO2 0.92 (0.67, 1.26) per 15 μg/m3c |
| [42] | CANHEART | Ontario, Canada | 2008–2008 | Cross sectional | 2,496,458 (52%) | 53 | Disease register | Age, sex, iSES, nSES, area | PrevalenceNO2 1.16 (1.14, 1.17) per 10 ppbc |
| [37] | SALIA | North Rhine-Westphalia, Germany | 1985–2006 | Cohort | 17,752 (100%) | 54 | Multimodal | Age, sex, smoking, BMI | IncidenceNO2 1.42 (1.16, 1.73) per 15 μg/m3cPM2.5abs 1.27 (1.09, 1.48) per 0.39 1e-5/mcDistance 2.54 (1.31, 4.91) (low education) < 100 vs. >100 mDistance 0.92 (0.58, 1.47) (high education) < 100 vs. >100 m |
| [38] | ALSWH | Australia | 2006–2011 | Cross sectional | 269,912 (100%) | Range: 31–90 | Doctor-diagnosed | Age, smoking, behavior, BMI, area | Prevalence |
| NO2 1.04 (0.91, 1.20) per 3.7 ppbc | |||||||||
| Distance: 0.99 (0.95, 1.04) 3 per 1 km | |||||||||
| [64] | CAFEH | Boston, Massachusetts, United States | 2009–2012 | Cross sectional | 653 (58%) | 60 | Doctor-diagnosed | Age, iSES | PrevalencePNC 0.71 (0.46, 1.10) per 1 particles/cm3; log-transformed |
| [65] | CHAMPIONS | Leicestershire, United Kingdom | 2004–2011 | Cross sectional | 10,443 (47%) | 59 | Clinical examination | Age, sex, iSES, nSES, smoking, behavior, BMI, area | Prevalence |
| NO2 1.10 (0.92, 1.32) per 10 μg/m3c | |||||||||
| PM10 1.3 (0.5, 2.9) per 10 μg/m3c | |||||||||
| PM2.5 1.6 (0.4, 4.6) per 10 μg/m3c | |||||||||
| [66] | MESA | Multiple cities, United States | 2000–2012 | Cohort | 5,135 (53%) | 62–64 (with diabetes) | Clinical examination | Age, sex. iSES, nSES, smoking, behavior, BMI, familial diabetes, area | Incidence |
| NOx 1.04 (0.77, 1.40) per 47.1 ppba | |||||||||
| PM2.5 1.05 (0.87, 1.26) per 2.43 μg/m3a | |||||||||
| Distance 0.96 (0.80, 1.16) <100 vs. >100 m | |||||||||
| Prevalence | |||||||||
| NOx 1.29 (0.94, 1.76) per 47.1 ppb | |||||||||
| PM2.5 1.16 (0.94, 1.42) per 2.43 μg/m3c | |||||||||
| Distance 1.10 (0.91, 1.34) <100 vs. >100 m | |||||||||
| [67] | Nurses’ Health Health Professionals Follow-Up | United States | 1989–2002 | Cohort | 89,460 (83%) | 55 | Multimodal | Age, sex, iSES, smoking, behavior, BMI, familial diabetes, hypertension, year, area | IncidenceDistance 1.11 (1.01, 1.23) 0–49 vs. >200 mDistance 0.96 (0.63, 1.48) 50–99 vs. >200 mDistance 0.96 (0.87, 1.06) 100–199 vs. >200 m |
| [32] | Rome Longitudinal | Rome, Italy | 2008–2013 | Cohort | 1,319,193 (55%) | Range: 35–70 | Administrative data from hospital and insurance registries | Age, sex, iSES | Incidence |
| NO2 1.00 (1.00, 1.01) per 10 μg/m3c | |||||||||
| NOx 1.01 (1.00, 1.01) per 20 μg/m3c | |||||||||
| PM2.5abs 1.00 (0.98, 1.02) per 1 × 10−5/mc | |||||||||
| PM10 1.00 (0.99, 1.02) per 10 μg/m3 | |||||||||
| PM2.5 1.00 (0.98, 1.02) per 5 μg/m3c | |||||||||
| PMcoarse 0.99 (0.97, 1.02) per 10 μg/m3 | |||||||||
| Prevalence | |||||||||
| NO2 1.00 (1.00, 1.01) per 10 μg/m3c | |||||||||
| NOx 1.01 (1.00, 1.01) per 20 μg/m3 | |||||||||
| PM2.5abs 0.98 (0.96, 0.99) per 1 × 10−5/m | |||||||||
| PM10 0.99 (0.98, 1.00) per 10 μg/m3c | |||||||||
| PM2.5 0.98 (0.96, 1.00) per 5 μg/m3c | |||||||||
| PMcoarse 0.96 (0.94, 0.98) per 10 μg/m3 | |||||||||
| [68] | ELISABET | Lille and Dunkirk, France | 2011–2013 | Cross sectional | 2,797 (53%) | 53 | Clinical examination | Age, sex, iSES, smoking, behavior, BMI, area | Prevalence |
| NO2 1.06 (0.90, 1.25) per 5 μg/m3cPM10 1.04 (0.86, 1.25) per 2 μg/m3c | |||||||||
| [39] | HNR | Ruhr Areas, Germany | 2000–2008 | Cohort | 3,607 (52%) | 59 | Clinical examination | Age, sex, iSES, nSES, smoking, behavior, BMI, area | Incidence |
| PM10 1.05 (1.00, 1.10) per 1 μg/m3 | |||||||||
| PM2.5 1.03 (0.95, 1.12) per 1 μg/m3c traffic PM2.5 1.36 (0.97, 1.89) per 1 μg/m3 | |||||||||
| Distance 1.37 (1.04, 1.81) <100 vs. 100–200 m | |||||||||
| [69] | 33 CCHS | Multiple cities, China | 2009–2009 | Cross sectional | 15,477 (47%) | 45 | Clinical examination | Age, sex, iSES, smoking, behavior, BMI, familial diabetes, area | PrevalenceNO2 1.22 (1.12, 1.33) per 9 μg/m3 |
| [43] | 33 CCHS | Multiple cities, China | 2009–2009 | Cross sectional | 15,477 (47%) | 45, both | Clinical examination | Age, sex, iSES, nSES, smoking, behavior, (BMI)e, familial CVD, co-pollutants | PrevalenceNO2 1.20 (1.08, 1.32) per 10 μg/m3c |
Characteristics of the studies reporting on the association of traffic-related air pollution and diabetes incidence or prevalence (Global 2022).
Abbreviations: CI, confidence interval; iSES, measures of individual socioeconomic status such as education; income; nSES, measures of neighborhood socioeconomic status such as neighborhood household income; BMI, body mass index; area, area level adjustments such as city DDCH.
Effect estimates can be ORs, RRs, HRs, or IRRs, depending on the analysis.
Adjusted for other behavioral factors other than smoking such as diet, alcohol consumption or physical activity.
Effect estimates included in meta-analysis.
Adjusted for hypertension, COPD, asthma, congestive heart failure, acute myocardial infarction, and cancer.
Multimodal strategies to identify diabetes cases include a combination of self-reported doctor-diagnosed cases, clinical examinations of blood sugar levels or use of medication for glycaemic control.
BMI was not included but considered.
Study Description
All studies were published after 2010. Nine studies estimated the association of TRAP with incidence of diabetes, 10 with diabetes prevalence, and two with both incidence and prevalence (the Rome Longitudinal [32] and the SAPALDIA study [33, 34]). The majority of the studies were conducted in Europe (10) or North America (8), followed by China (2) and Australia (1). Three studies were exclusively of women (BWHS [35, 36], SALIA [37], ALSWH [38]). NO2 or NOx were the most commonly studied pollutants (17), 11 studies investigated at least one particle metric, and seven included proximity metrics. Exposure levels ranged from very low (e.g., Australia, Canada) to high (e.g., Rome, Italy, China), with ranges in annual means of 5–42 µg NO2/m3 and 4–25 µg PM2.5/m3. The 11 cohort studies, all conducted in Europe or North America, included 2,931 to over 1 million participants with a range of follow-up of 4–16 years. The ten cross-sectional studies had 513 up to 2.5 million participants.
Diabetes definitions varied, and included self-report of physician-diagnosed diabetes (five studies), disease registers (two studies), administrative data (e.g., insurance claims) indicating diabetes diagnosis or prescription of hypoglycemic medications (three studies), clinical examinations at study centers, measuring blood glucose (five studies), or using a combination of different data sources (blood glucose measurements, questionnaire, medication, data linkage, six studies). Most smaller cohort studies (n < 10,000 participants) used clinical examinations (SAPALDIA, HNR, MESA, CHAMPIONS) or self-reported physician-diagnosed diabetes, whereas larger administrative cohort or cross-sectional studies typically relied on linkage to administrative databases or registers (e.g., ONPHEC, Rome longitudinal, Table 1).
Results of Meta-Analysis
Meta-analyses indicated positive associations of all traffic-related air pollutants with diabetes incidence and prevalence, though estimates were imprecise (Figure 1). For example, higher exposure to NO2, the TRAP for which there were the most studies (seven studies), corresponded to higher diabetes prevalence (RR 1.09; 95% CI: 1.02; 1.17 per 10 μg/m3); the individual estimates were highly heterogeneous, especially for the NO2 results (Figure 2). The association was less pronounced for diabetes incidence (RR 1.04; 95% CI: 0.96; 1.13 per 10 μg/m3; Figure 3). The summary estimates for EC, PM2.5 and PM10 were also positive but even less precise and based on fewer individual studies.
FIGURE 1
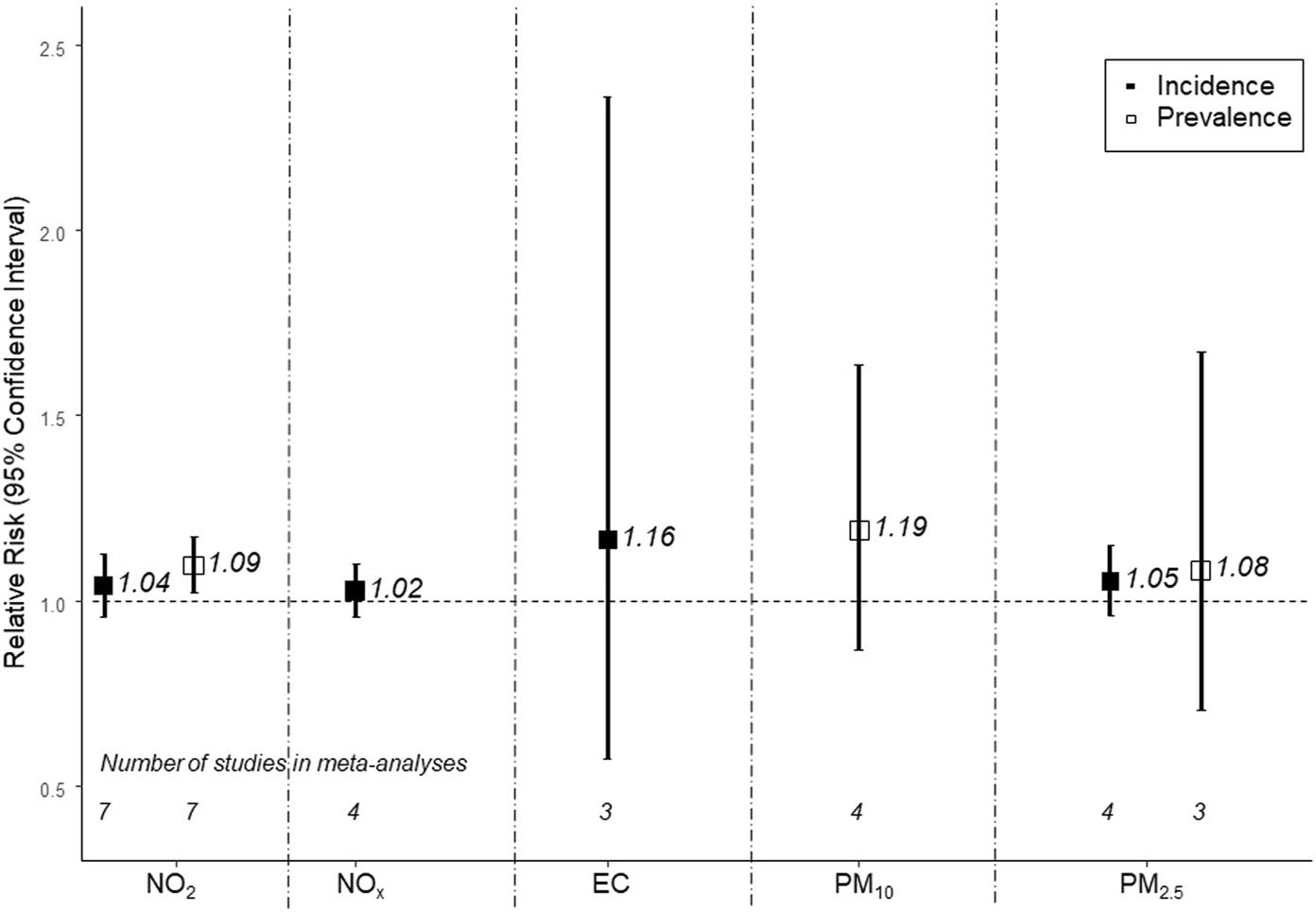
Meta-analysis of associations between traffic-related air pollutants and diabetes prevalence (empty squares) and incidence (filled squares) (Global 2022). The following increments were used: 10 µg/m3 for NO2, 20 μg/m3 for NOx, 1 μg/m3 for EC, 10 μg/m3 for PM10, and 5 μg/m3 for PM2.5. Effect estimates cannot be directly compared across the different traffic-related pollutants because the selected increments do not necessarily represent the same contrast in exposure.
FIGURE 2
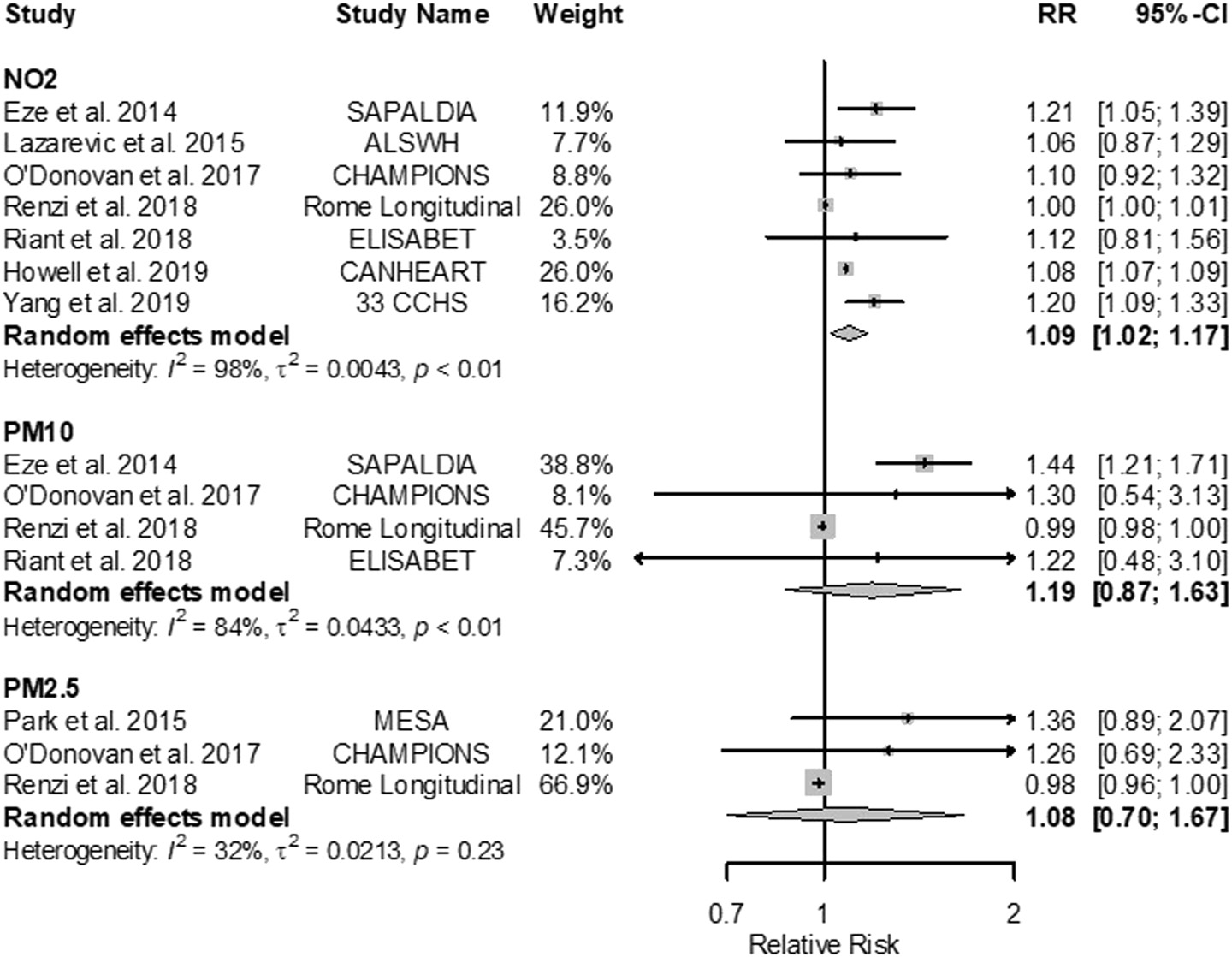
Forest plots of adjusted RRs (95% CIs) for diabetes prevalence with NO2, PM10, and PM2.5 (Global 2022). The size of the grey squares represents the weight of the study in the meta-analysis. The following increments were used: 10 μg/m3 for NO2, 20 μg/m3 for NOx, 1 μg/m3 for EC, 10 μg/m3 for PM10, and 5 μg/m3 for PM2.5. Effect estimates cannot be directly compared across the different traffic-related pollutants because the selected increments do not necessarily represent the same contrast in exposure.
FIGURE 3
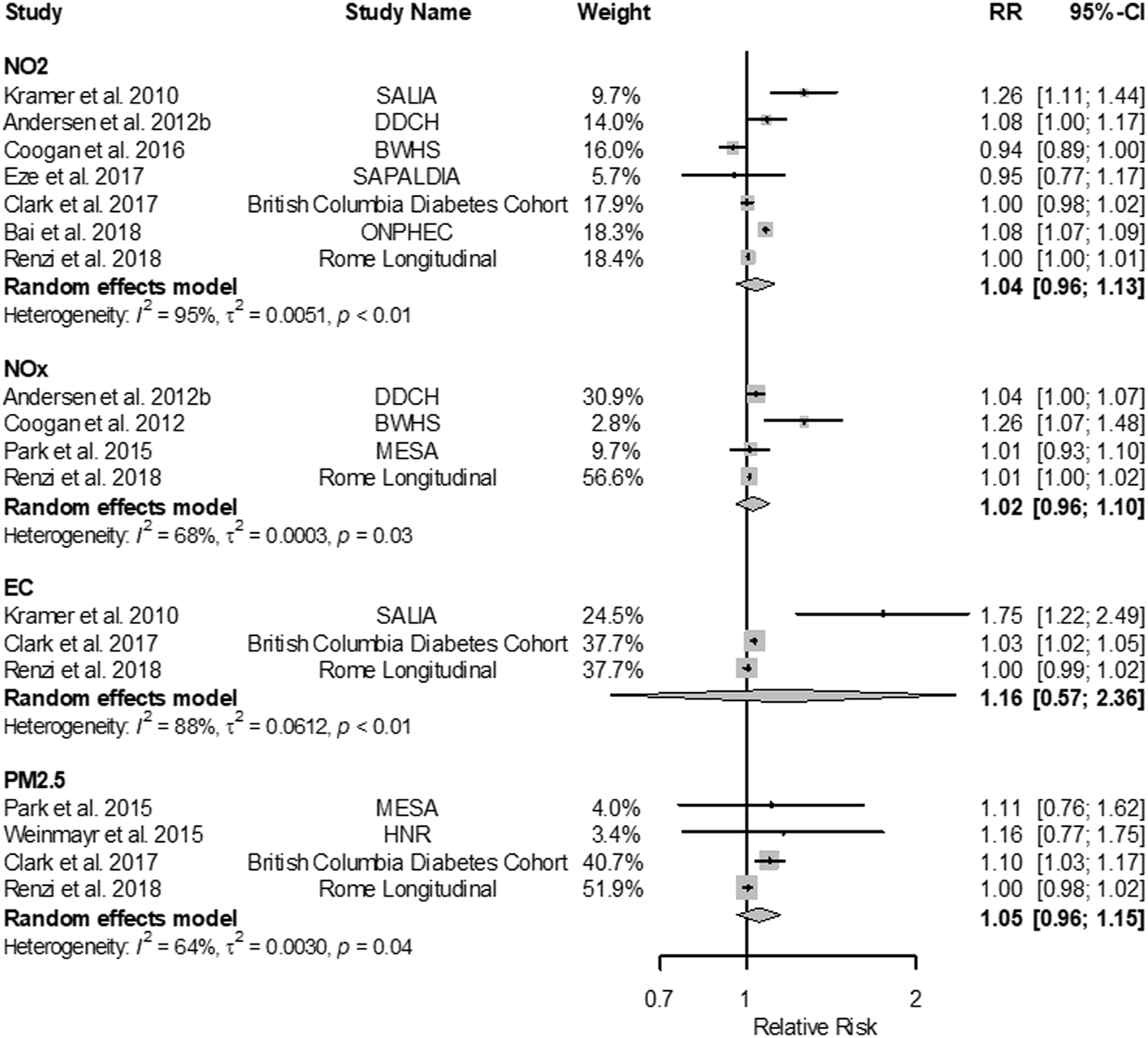
Forest plots of adjusted RRs (95% CIs) for diabetes incidence with NO2, NOx, EC and PM2.5 (Global 2022). The size of the grey squares represents the weight of the study in the meta-analysis. The following increments were used: 10 µg/m3 for NO2, 20 µg/m3 for NOx, 1 µg/m3 for EC, 10 µg/m3 for PM10, and 5 µg/m3 for PM2.5. Effect estimates cannot be directly compared across the different traffic-related pollutants because the selected increments do not necessarily represent the same contrast in exposure.
Results From Studies Not Entering Meta-Analysis
For pollutants not included in the meta-analyses (such as ultrafine particles PNC or NO, marked in Table 1 without c) elevated risks were observed for measures of NOx but not the various measures of PM in the prevalence analyses. The incidence analyses showed elevated risks for diabetes with NO and PNC. Notably, the traffic-specific PM2.5 in the HNR cohort [39] yielded a substantially larger association compared to the total PM2.5 mass estimates (RR 1.36 vs. 1.03 or 1.05 per 1 μg/m3). All but one study (MESA) showed positive (though imprecise) associations with distance and density of traffic (Table 1, Supplementary Figures S3, S4).
Risk of Bias and Subgroup and Sensitivity Analysis
The ONPHEC [40], British Columbia Diabetes Cohort [41], CANHEART [42], and Rome Longitudinal study [32] were considered to have high RoB due to incomplete confounder control (missing adjustment for smoking or socioeconomic status). The SAPALDIA cohort [33, 34] was considered to have high potential for selection bias due to long survival in a cohort before inclusion into the analysis and the 33 CCHS study had extensive missing data [43] (Supplementary Table S5).
In subgroup analyses excluding these studies, association magnitudes were similar or larger (Supplementary Tables S6, S7). For example, restricting to prevalence studies with smoking adjustment eliminated heterogeneity entirely and yielded meta-analytic estimates for NO2 of 1.09 [95% CI: 1.02; 1.17] (from 1.17 [1.09; 1.25]), and for PM10 of 1.19 [0.87; 1.63] (from 1.43 [1.28; 1.59]).
Five studies evaluated confounding by concurrent noise exposure (British Columbia Diabetes Cohort, Plovdiv Diabetes Survey, both SAPALDIA analyses, Rome longitudinal [32–34, 41, 44], Supplementary Table S8). Most TRAP effect estimates were attenuated upon noise adjustment, but still showed elevated risks. For example, the NO2 prevalence results in the SAPALDIA study were reduced from 1.21 [1.05; 1.39] to 1.19 [1.03, 1.38] when adjusting for noise [34].
Confidence Assessments
The modified OHAT assessment was conducted for the 16 studies entering meta-analyses (Table 2). Among factors reducing the quality of the evidence, the most common factor was imprecision (wide CI and including unity despite sufficient sample size). For NO2 and diabetes incidence, the confidence was upgraded due to monotonic exposure-response functions reported in two studies [40, 45]. We upgraded the evidence on NO2 and prevalence due to potential downward bias. We arrived at a moderate confidence assessment for overall TRAP based on the moderate confidence for NO2. While the confidence was low for the other pollutants, the associations for these pollutants were suggestive of an association, though imprecise.
TABLE 2
| Pollutant | High ++++ | Factors decreasing confidence “0” if no concern; if serious concern to downgrade confidence | Factors increasing confidence “0” if not present; “+” if sufficient to upgrade confidence | Final confidence rating | Rating across study designs | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Moderate +++ | |||||||||||
| Low ++ | |||||||||||
| Very low + | |||||||||||
| Study design | Initial confidence rating (# studies) | Risk of bias | Unexplained inconsistency | Imprecision | Publication bias | Monotonic exposure-response | Consideration of residual confounding | Consistency across populations | |||
| NO2 | Cohort | +++ (N = 7) | 0 | - | - | 0 | + | 0 | 0 | ++ (Low) | +++ (Moderate) |
| Rationale | Cohort design initially rated as moderate | Four studies with high RoB but results not sensitive to exclusions of those studies | High heterogeneity (I2 = 95%), due to both magnitude and direction | Sample size met, but confidence interval wide and includes unity | No formal evaluation possible | Two influential studies show monotonic ERF (Andersen, 2012b; Bai, 2018) | Confounding in both directions possible | Too few studies to evaluate | The combined rating is based on the higher confidence rating. Both study designs show evidence of a positive association, therefore no reason for a downgrade | ||
| Cross-sectional | ++ (N = 7) | 0 | 0 | 0 | 0 | 0 | + | 0 | +++ (Moderate) | ||
| Rationale | Cross-sectional design initially rated as low | Three studies with high RoB, increased or stable effect estimates after excluding high RoB studies | High heterogeneity (I2 = 98%) due to magnitude not direction | Sample size met, and confidence interval does not include unity | No formal evaluation possible | No evidence of plausible shape of ERF. | Larger estimates in studies with better confounder control suggests residual confounding toward the null | Across different populations robust effect, but too few studies | |||
| NOX | Cohort | +++ (N = 4) | 0 | 0 | - | 0 | 0 | 0 | 0 | ++ (Low) | NA |
| Rationale | Cohort design initially rated as moderate | One study high RoB, but increased estimate after exclusion | Moderate heterogeneity (I2 = 68%) mostly due to magnitude not direction | Sample size met, but confidence interval wide and includes unity | No formal evaluation possible | No evidence of plausible shape of ERF | Confounding in both directions possible | Too few studies to assess robustness across populations | |||
| EC | Cohort | +++ (N = 3) | 0 | 0 | - | 0 | 0 | 0 | 0 | ++ (Low) | NA |
| Rationale | Cohort design initially rated as moderate | Elevated estimate based on one study with moderate RoB. Two studies with high RoB show effect closer to the null | High heterogeneity (I2 = 88%) due to magnitude not direction | Sample size met, but confidence interval wide and includes unity | No formal evaluation possible | No evidence of plausible shape of ERF. | Confounding in both directions possible | Insufficient evidence for robustness across populations | |||
| PM10 | Cross-sectional | ++ (N = 4) | 0 | 0 | - | 0 | 0 | 0 | 0 | + (Very low) | NA |
| Rationale | Cross-sectional design initially rated as low | One of 4 studies high RoB but increased estimate upon exclusion of the high RoB study | High heterogeneity (I2 = 84%) due to magnitude not direction | Sample size met, but confidence interval wide and includes unity | No formal evaluation possible | No evidence of plausible shape of ERF. | Larger estimates in studies with better confounder control, but number of studies considered too small for upgrade | All studies European, no consistency check possible | |||
| PM2.5 | Cohort | +++ (N = 4) | 0 | 0 | - | 0 | 0 | 0 | 0 | ++ (Low) | ++ (Low) |
| Rationale | Cohort design initially rated as moderate | Two studies high RoB, but increased estimate upon exclusion of high RoB studies | Moderate heterogeneity (I2 = 64%) due to magnitude not direction | Sample size met, but confidence interval wide and includes unity | No formal evaluation possible | No evidence of plausible shape of ERF. | Larger estimates in studies with better confounder control, but number of studies considered too small for upgrade | Insufficient evidence for robustness across populations | Both study designs show estimates in the same direction | ||
| Cross-sectional | ++ (N = 3) | 0 | 0 | - | 0 | 0 | 0 | 0 | + (Very low) | ||
| Rationale | Cross-sectional design initially rated as low | One study high RoB, no sensitivity analysis due to low numbers | Low heterogeneity (I2 = 32%) | Sample size met, but confidence interval wide and includes unity | No formal evaluation possible | No evidence of plausible shape of ERF | Larger estimates in studies with better confounder control, but number of studies too small | Insufficient evidence for robustness across populations | |||
Confidence rating for the quality in the body of evidence for traffic-related air pollution and diabetes (Global 2022).
The downgrading factor indirectness and the upgrading factor large magnitude of effect were not considered further.
A confidence rating of moderate was also reached in the narrative assessment that considered all studies. This rating was based on the meta-analytical evidence of an association of NO2 with diabetes prevalence and suggestive evidence of an association of NO2, NOx, traffic-related PM with incident and prevalent diabetes. The confidence in the evidence was further supported by the monotonic exposure-response relationships reported in two studies, positive albeit imprecise associations involving indirect traffic measures, and numerous positive associations from studies that adjusted for likely confounders. Further, associations generally remained positive after adjustment for noise exposure (Supplementary Table S8). Finally, effect estimates were larger among the subgroup of studies with more extensive confounder adjustment, and among studies that used comprehensive outcome ascertainment methods (versus self-report and administrative data) (Supplementary Tables S6, S7).
Study Characteristic and Supplemental Analysis of Studies From the Extended Search
Since our systematic search ending in July 2019, new studies have been published on TRAP and diabetes. We extended our search to May 2022 resulting in 304 hits. Five studies met the inclusion criteria (Table 3) adding estimates to all meta-analyses on diabetes incidence and the PM2.5 prevalence analyses (Supplementary Figures S5–S7). While the pooled estimates did not change dramatically, risk estimates were still elevated and confidence intervals became narrower; especially for the PM2.5-incidence analyses that was borderline significant (Supplementary Figure S5). Additionally, the Danish study [46] with traffic-specific pollutant estimates and the HNR analysis from 2020 [47] with longer follow-up and refined source-specific exposure assessment as compared to the 2015 analysis [39] showed significantly elevated risks related to traffic-specific NO2, EC, and PM2.5. Both also add to the evidence on ultrafine particles. However, measures were not comparable and thus meta-analysis was not possible for the different metrics of UFP. Overall, the results of the HEI 2022 review were strengthened by supplemental analyses of the studies identified in the updated search.
TABLE 3
| Reference | Study name | Location | Study period | Study design in analysis | Sample size N (% women) | Age at baseline | Ascertainment of diabetes | Confounder adjusted for | Results (estimatea, 95% CI, increment) |
|---|---|---|---|---|---|---|---|---|---|
| [47] | HNR | Ruhr Areas, Germany | 2006–2015 | Cohort | 2,451 (52%) | 58 | Self-reported or medication or clinical examination | Age, sex, smoking, behavior, noise (extended models unchanged results iSES, nSES) | Incidence |
| NO2: 1.02 (0.99, 1.05) per 1 μg/m3b traffic NO2: 1.06 (1.01, 1.12) per 1 μg/m3 | |||||||||
| PM10: 1.06 (1.01, 1.12) per 1 μg/m3 traffic PM10: 2.00 (1.19, 3.34) per 1 μg/m3 | |||||||||
| PM2.5: 1.06 (0.98, 1.16) per 1 μg/m3b traffic PM2.5: 2.13 (1.26, 3.61) per 1 μg/m3 | |||||||||
| PNC<1: 1.29 (1.10, 1.53) per 500 particles/mL traffic PNC < 1: 2.11 (1.04, 4.28) per 500 particles/mL | |||||||||
| [46] | National Danish Register | Denmark | 2005–2017 | Prospective cohort | 2,631,488 (51.4%) | 52 | Administrative data from hospital and prescription registers | Age, sex, iSES, nSES | Incidence |
| NO2: 1.056 (1.046, 1.065) per 7.15 μg/m3b traffic NO2: 1.039 (1.031, 1.047) per 5.17 μg/m3 | |||||||||
| EC: 1.022 (1.016, 1.027) per 0.28 μg/m3b traffic EC: 1.037 (1.030, 1.043) per 0.17 μg/m3 | |||||||||
| PM2.5: 1.043 (1.031, 1.056) per 1.85 μg/m3b traffic PM2.5: 1.026 (1.020, 1.031) per 0.37 μg/m3 | |||||||||
| PNC: 1.052 (1.042, 1.063) per 4,248 particles/mL traffic PNC: 1.049 (1.040, 1.058) per 1,698 particles/mL | |||||||||
| [70] | 487 Municipalities | Multiple cities, Indonesia | 2013 | Cross sectional | 647,947 (52%) | 42 | Self-reported | Age, sex, iSES, smoking, behavior, BMI, area, intermediate | PrevalencePM2.5: 1.09 (1.05, 1.14) per 10 μg/m3 |
| [71] | JHS | Jackson, Mississippi, United States | 2000–2008 | Cohort | 5,128 (63%) | 55 | Clinical examination or medication | Age, sex, nSES, smoking, behavior, familial diabetes, BMI, others, area | Incidence |
| PM2.5: 1.09 (0.90, 1.32) per 0.81 μg/m3b | |||||||||
| Prevalence | |||||||||
| PM2.5: 1.08 (1.00, 1.17) per 0.81 μg/m3 | |||||||||
| Distance: 0.91 (0.61, 1.36) <150 vs. 1,000 m | |||||||||
| Distance: 0.94 (0.74, 1.20) 150–299 vs. 1,000 m | |||||||||
| Distance: 1.01 (0.91, 1.12) 300–999 vs. 1,000 m | |||||||||
| [72] | SALSA | Sacramento, California, United States | 1998–2007 | Cohort | 1,075 (59%) | 71 | Self-reported, medication or clinical examination | Age, sex, iSES, nSES, smoking, co-pollutant | Incidence |
| NO2: 1.02 (0.98, 1.05) per 6.1 ppbb | |||||||||
| NOx: 1.13 (0.96, 1.33) per 2.3 ppbb | |||||||||
| PM2.5: 1.20 (1.03, 1.40) per 1.9 μg/m3b | |||||||||
Characteristics of the studies from extended search up to May 2022 reporting on the association of traffic-related air pollution and diabetes incidence or prevalence (Global 2023).
Abbreviations: CI, confidence interval; iSES, measures of individual socioeconomic status such as education; income; nSES, measures of neighborhood socioeconomic status such as neighborhood household income, BMI, body mass index; area, area level adjustments such as city DDCH.
Effect estimates can be ORs, RRs, HRs, or IRRs, depending on the analysis.
Effect estimates included in meta-analysis
Discussion
In this comprehensive systematic review of epidemiologic evidence on the association of TRAP with adult diabetes, we identified 21 pertinent studies. Our summary estimates generally suggested an adverse association of TRAP with diabetes risk, although some of the effect estimates were imprecise and based on small numbers of studies per pollutant-outcome pair. A statistically significant association was reported between NO2 and diabetes prevalence with a summary estimate of 1.09 (95% CI: 1.02; 1.17) per 10 μg/m3, supported by consistently positive but imprecise estimates for the other traffic-related air pollutants. Results were strengthened by the reporting of a monotonic exposure-response function in two studies [40, 45], positive associations in studies examining indirect traffic measures, and robust results correcting for traffic noise. The confidence assessment yielded a moderate confidence in the evidence for an association between long-term exposure to TRAP and diabetes. We noted more consistent associations of TRAP with diabetes prevalence than incidence.
The newly identified five studies, with mostly rigorous outcome assessments strengthened the results. Confidence intervals of meta-analytic estimates in the supplemental analyses were less wide, though estimates were still not significantly elevated.
Findings in Relation to Other Reviews
Recent reviews of ambient air pollution—as opposed to our focus on traffic-related air pollution—in association with diabetes found similar results (Supplementary Table S9). With a larger study base, Lui et al. [6] and Yang et al. [5] not only reported significantly elevated risks for diabetes prevalence with NO2, but also with PM10, and PM2.5 (for example, including 11 studies vs. 3 studies in the PM2.5 prevalence analyses). Diabetes incidence risk was significantly elevated with PM2.5 in both reviews, and additionally with PM10 in the analysis by [5] considering two more studies. As in our analysis, the reviews did not find a significantly elevated risk with NO2 and diabetes incidence. Effect estimates seemed slightly larger in our prevalence analysis, though more imprecise (for example, 1.09 [1.02; 1.17] vs. 1.05 [1.03; 1.08] and 1.07 [1.04; 1.11]) in the NO2 prevalence analysis. Another review reported elevated diabetes risks in association with living close to major roads [48].
Biological Mechanisms
Plausible pathways regarding how TRAP could lead to diabetes are discussed in the literature. Important mechanisms include oxidative stress induced inflammation leading to endothelial and mitochondrial dysfunction, resulting in impaired insulin signalling and insulin resistance [10]. Animal studies provide evidence that exposure to high concentrations of traffic particles may be a risk factor in the development of diabetes [49–51]. Studies evaluating mechanistic pathways underlying such metabolic perturbations induced by urban PM and near roadway air pollution have identified possible contributory roles played by inflammation and altered fatty acid metabolism. Indeed, Lucht et al. [47] observed that diabetes incidence in an adult population was mediated by markers of inflammation (adiponectin and C-reactive protein). While our results build on evidence found especially for the association with NO2, mechanistic studies on NO2 are scarce [52] and NO2 could be an indicator for other highly correlated pollutants from the same source. However, a recent study on Witstar rats was able to demonstrate reactive oxygen species formation and mitochondrial and endothelial dysfunction after 3 weeks of repeated high NO2 exposure [53]. Epidemiologic studies also found TRAP-associated higher risks for glucose homeostasis dysregulation measured as insulin concentration in cord blood, fasting blood glucose, insulin sensitivity, HOMA-IR, HbA1c in newborns [54], children [55, 56], adolescents [57], and adults [58] indicating a role of early-life exposure.
Strengths
The systematic approach to study selection and evaluation using an a priori specified framework for exposure assessment and for a systematic evaluation of the epidemiological evidence are major strengths of this review. Even though none of the pollutants are uniquely traffic-specific, the use of several indicators of TRAP allowed the evaluation of consistency across pollutants and enabled the Panel to base its conclusions on a larger number of studies with diverse exposure metrics. Additionally, the application of two complementary methods (the modified OHAT assessment for studies entering meta-analyses and the narrative assessment considering all studies for the evaluation of the epidemiological evidence maximizes what can be learned from the epidemiologic studies, including evidence from less studied pollutants like UFP and traffic-specific PM fractions.
Limitations
The overall number of studies per pollutant was small, limiting our ability to conduct meta-analysis or subgroup analysis for some exposure-outcome pairs, and to investigate publication bias.
It has been proposed that effects of air pollutants on the metabolic system commence at an early age [54, 55]. Studies entering this review, including the newest available studies, comprised older adult populations (mean age >50 years) and have excluded persons with already manifest pollutant-dependent diabetes at baseline from the incidence analyses. Thus, a selection bias toward a healthier population might have compromised the ability to study associations with diabetes incidence. The subgroup analysis showed more robust results for studies with low risk of selection bias (Supplementary Table S6).
Another limitation refers to the possible underestimation and misclassification of diabetes. This may depend on the age of the study participants regarding results on incidence of diabetes or on study design and available data sources. Cohort studies with individual data or smaller cross-sectional studies show more rigorous outcome ascertainment with less risk of bias as opposed to the larger studies based on administrative data. Reliance on self-report or documented disease would miss 24% up to 50% of cases depending on the region, while in-depth study center examinations will have a much higher sensitivity due to the long oligosymptomatic prediagnostic phase of diabetes [2]. Non-differential outcome misclassification (independent from exposure status) related to incomplete case ascertainment might bias the results to the null [59, 60]. This was seen for prevalence studies in the sub-group analysis regarding risk of bias due to outcome ascertainment, but not incidence studies (Supplementary Tables S6, S7).
We were not able to distinguish between type 1 and type 2 diabetes. Since 90% of adult diabetes cases are type 2, and the vast majority of incident diabetes cases in adults are type 2 diabetes, we conclude that our results primarily refer to type 2 diabetes.
Future Research
In cities, where the majority of the world´s population resides, traffic remains an important source of air pollution. The majority of studies were from high-income countries in Europe and North America with generally lower levels of air pollution than in other world regions. However, the one study from China with mean exposure at the higher end of the exposure range (35.3 μg/m3 NO2) also showed increased risk of diabetes. The available evidence provides overall moderate evidence that TRAP increase diabetes risk. Large studies with rigorous case ascertainment are needed, including in low and middle income countries and other locations with higher exposures. Studies are also needed to assess the change in composition of TRAP due to diesel and gasoline fleet turnover to lower-emission vehicles with a rising share of non-tailpipe emissions in the overall share of traffic-related particulate matter (e.g., from SO2 emissions). The interplay of TRAP with co-exposures in polluted spaces, most notably noise and green space, needs to be better understood for effective intervention [61].
Studies assessing critical windows of exposure, e.g., in younger populations and preclinical outcomes along the mechanistic path to clinically manifest disease are warranted. Evidence suggests that underlying pathology may be underway as early as childhood and adolescence [62]. Future experimental studies should provide more mechanistic evidence for a better understanding of the molecular and cellular actions of long-term exposure to NOx and other TRAP on the cardiometabolic system.
Conclusion
In conclusion, we found moderate confidence in the evidence for an association of long-term exposure to traffic-related air pollution and diabetes, with higher effect estimates observed in prevalence studies. We observed increased risks in populations in various geographical regions and contexts and conclude, that TRAP is a risk factor for diabetes.
Statements
Author contributions
MKJ, BH, and ES were responsible for drafting the article; Panel members, MKJ, RK, and PH as well as AP, HB were responsible for the design and conduct of the broader systematic review on health effects of ambient air pollution, on which this work is based. ES and RA conducted formal analysis. ES conducted the extended analysis and prepared the figures on results of the meta-analyses. All authors were responsible for revising the article critically for important intellectual content. All authors contributed to the article and approved the submitted version.
Funding
Research described in this article was conducted under contract to the HEI, an organization jointly funded by the United States Environmental Protection Agency (EPA) [Assistance Award No. CR-83998101] and certain motor vehicle and engine manufacturers. MKJ work is supported by the Swiss Federal Office for the Environment [Grant No. 17.0094.PJ/R192-0332] as part of its funding for the work of the LUDOK-database. The funders were not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Acknowledgments
The authors would like to thank the consultants to the Panel, external reviewers, HEI staff and contract team members involved in the preparation of the comprehensive review report. Bert Brunekreef, Institute for Risk Assessment Sciences, Environmental Epidemiology, Utrecht University, Netherlands; Dan Crouse, Health Effects Institute, Boston, MA, United States; Alan da Silveira Fleck, Health Effects Institute, Boston, MA, United States; Dan Greenbaum, Health Effects Institute, Boston, MA, United States; Leonie Hoffmann, University of Düsseldorf, Germany; Frank Kelly, School of Public Health, Imperial College, London, United Kingdom; Julia Fussell, School of Public Health, Imperial College, London, United Kingdom; Tim Nawrot, Hasselt University, Hasselt, Flanders, Belgium; Robert O’Keefe, Health Effects Institute, Boston, MA, United States; Martha Ondras, Health Effects Institute, Boston, MA, United States; Zoe Roth, Swiss Tropical and Public Health Institute, University of Basel, Switzerland; Margaux Sadoine, Health Effects Institute, Boston, MA, United States; Rashik Shaikh, Health Effects Institute, Boston, MA, United States; Lara Stucki, Swiss Tropical and Public Health Institute, University of Basel, Switzerland; Eva Tanner, Health Effects Institute, Boston, MA, United States; Annemoon van Erp, Health Effects Institute, Boston, MA, United States; Eleanne van Vliet, Health Effects Institute, Boston, MA, United States; Greg Wellenius, Boston University School of Public Health, Boston, MA, United States; Elina Wüthrich, Swiss Tropical and Public Health Institute, University of Basel, Switzerland.
Conflict of interest
Author FL was employed by the company Sonoma Technology, Inc.
The remaining authors declare that they do not have any conflicts of interest.
Author disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the views of the Health Effects Institute or its sponsors.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2023.1605718/full#supplementary-material
References
1.
GoyalRJialalI. Diabetes Mellitus Type 2. StatPearls. Treasure Island (FL): StatPearls Publishing LLC. (2021). Available at: https://www.ncbi.nlm.nih.gov/books/NBK513253/ (Accessed November 12, 2021).
2.
International Diabetes Federation. IDF Diabetes Atlas. Brussels, Belgium: International Diabetes Federation (2021).
3.
BeulensJWJPinhoMGMAbreuTCden BraverNRLamTMHussAet alEnvironmental Risk Factors of Type 2 Diabetes-An Exposome Approach. Diabetologia (2021) 65(2):263–74. 10.1007/s00125-021-05618-w
4.
WuYFuRLeiCDengYLouWWangLet alEstimates of Type 2 Diabetes Mellitus Burden Attributable to Particulate Matter Pollution and its 30-Year Change Patterns: A Systematic Analysis of Data from the Global Burden of Disease Study 2019. Front Endocrinol (Lausanne) (2021) 12:689079. 10.3389/fendo.2021.689079
5.
YangBYFanSThieringESeisslerJNowakDDongGHet alAmbient Air Pollution and Diabetes: A Systematic Review and Meta-Analysis. Environ Res (2020) 180:108817. 10.1016/j.envres.2019.108817
6.
LiuFChenGHuoWWangCLiuSLiNet alAssociations between Long-Term Exposure to Ambient Air Pollution and Risk of Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis. Environ Pollut (2019) 252(Pt B):1235–45. 10.1016/j.envpol.2019.06.033
7.
MozafarianNHashemipourMYazdiMZavarehMHTHovsepianSHeidarpourMet alThe Association between Exposure to Air Pollution and Type 1 Diabetes Mellitus: A Systematic Review and Meta-Analysis. Adv Biomed Res (2022) 11(1):103. 10.4103/abr.abr_80_21
8.
RenZYuanJLuoYWangJLiY. Association of Air Pollution and fine Particulate Matter (PM2.5) Exposure with Gestational Diabetes: a Systematic Review and Meta-Analysis. Ann Transl Med (2023) 11(1):23. 10.21037/atm-22-6306
9.
GoriniFSabatinoLGagginiMChatzianagnostouKVassalleC. Oxidative Stress Biomarkers in the Relationship between Type 2 Diabetes and Air Pollution. Antioxidants (Basel) (2021) 10(8):1234. 10.3390/antiox10081234
10.
AldereteTLChenZToledo-CorralCMContrerasZAKimJSHabreRet alAmbient and Traffic-Related Air Pollution Exposures as Novel Risk Factors for Metabolic Dysfunction and Type 2 Diabetes. Curr Epidemiol Rep (2018) 5(2):79–91. 10.1007/s40471-018-0140-5
11.
KhreisHNieuwenhuijsenMJZietsmanJRamaniT. Chapter 1 - Traffic-Related Air Pollution: Emissions, Human Exposures, and Health: An Introduction. In: KhreisHNieuwenhuijsenMZietsmanJRamaniT, editors. Traffic-Related Air Pollution. Elsevier (2020). p. 1–21. 10.1016/B978-0-12-818122-5.00001-6
12.
PiscitelloABiancoCCasassoASethiR. Non-exhaust Traffic Emissions: Sources, Characterization, and Mitigation Measures. Sci Total Environ (2021) 766:144440. 10.1016/j.scitotenv.2020.144440
13.
HEI. Systematic Review and Meta-Analysis of Selected Health Effects of Long-Term Exposure to Traffic-Related Air Pollution. Boston, MA, USA: Health Effects Institute (2022).
14.
BoogaardHPattonAPAtkinsonRWBrookJRChangHHCrouseDLet alLong-term Exposure to Traffic-Related Air Pollution and Selected Health Outcomes: A Systematic Review and Meta-Analysis. Environ Int (2022) 164:107262. 10.1016/j.envint.2022.107262
15.
HigginsJThomasJChandlerJCumpstonMLiTPageMet alCochrane Handbook for Systematic Reviews of Interventions. 2nd ed.Chichester (UK): John Wiley & Sons (2019).
16.
WHO. Risk of Bias Assessment Instrument for Systematic Reviews Informing WHO Global Air Quality Guidelines. Geneva, Switzerland: World Health Organization (2020). Contract No.: WHO/EURO:2020-2669-42425-58853.
17.
Office of Health Assessment Translation. Handbook for Conducting a Literature-Based Health Assessment Using OHAT Approach for Systematic Review and Evidence Integration. Washington, D.C: U.S. Department of Health and Human Services (2019).
18.
HEI (Health Effects Institute). Protocol for a Systematic Review and Meta–Analysis of Selected Health Effects of Long–Term Exposure to Traffic–Related Air Pollution. Massachusetts, United States: Health Effects Institute (2019).
19.
Department for Environment Food & Rural Affairs. Air Quality Library-Defra UK: Department for Environment Food & Rural Affairs (2005). Available from: https://uk-air.defra.gov.uk/library/reports?report_id=306 (Accessed February 22, 2023).
20.
CyrysJHeinrichJHoekGMeliefsteKLewnéMGehringUet alComparison between Different Traffic-Related Particle Indicators: Elemental Carbon (EC), PM2.5 Mass, and Absorbance. J Expo Anal Environ Epidemiol (2003) 13(2):134–43. 10.1038/sj.jea.7500262
21.
JanssenNAHHoekGSimic-LawsonMFischerPvan BreeLten BrinkHet alBlack Carbon as an Additional Indicator of the Adverse Health Effects of Airborne Particles Compared with PM10 and PM2.5. Environ Health Persp (2011) 119(12):1691–9. 10.1289/ehp.1003369
22.
Distiller SR. Version 2.29.8 2019 [cited 2021 December 9] (2019). Available from: https://www.evidencepartners.com/ (Accessed February 14, 2019).
23.
WHO. WHO Global Air Quality Guidelines. Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide. Geneva: WHO (2021).
24.
BeelenRRaaschou-NielsenOStafoggiaMAndersenZJWeinmayrGHoffmannBet alEffects of Long-Term Exposure to Air Pollution on Natural-Cause Mortality: an Analysis of 22 European Cohorts within the Multicentre ESCAPE Project. Lancet (2014) 383(9919):785–95. 10.1016/S0140-6736(13)62158-3
25.
VeronikiAAJacksonDViechtbauerWBenderRBowdenJKnappGet alMethods to Estimate the Between-Study Variance and its Uncertainty in Meta-Analysis. Res Synth Methods (2016) 7(1):55–79. 10.1002/jrsm.1164
26.
WoodwardM. Epidemiology: Study Design and Data Analysis. 3rd ed.Boca Raton, Fla: CRC Press (2014).
27.
DaviesHTCrombieIKTavakoliM. When Can Odds Ratios Mislead?BMJ (1998) 316(7136):989–91. 10.1136/bmj.316.7136.989
28.
KhreisHKellyCTateJParslowRLucasKNieuwenhuijsenM. Exposure to Traffic-Related Air Pollution and Risk of Development of Childhood Asthma: a Systematic Review and Meta-Analysis. Environ Int (2017) 100:1–31. 10.1016/j.envint.2016.11.012
29.
BoogaardHAtkinsonRBrookJChangHHoekGHoffmannBet alEvidence Synthesis of Observational Studies in Environmental Health: Lessons Learned from a Systematic Review on Traffic-Related Air Pollution. United States (2023). under review.
30.
ChenJHoekG. Long-term Exposure to PM and All-Cause and Cause-specific Mortality: A Systematic Review and Meta-Analysis. Environ Int (2020) 143:105974. 10.1016/j.envint.2020.105974
31.
HuangfuPAtkinsonR. Long-term Exposure to NO(2) and O(3) and All-Cause and Respiratory Mortality: A Systematic Review and Meta-Analysis. Environ Int (2020) 144:105998. 10.1016/j.envint.2020.105998
32.
RenziMCerzaFGariazzoCAgabitiNCasciniSDi DomenicantonioRet alAir Pollution and Occurrence of Type 2 Diabetes in a Large Cohort Study. Environ Int (2018) 112:68–76. 10.1016/j.envint.2017.12.007
33.
EzeICForasterMSchaffnerEVienneauDHeritierHRudzikFet alLong-term Exposure to Transportation Noise and Air Pollution in Relation to Incident Diabetes in the SAPALDIA Study. Int J Epidemiol (2017) 46(4):1115–25. 10.1093/ije/dyx020
34.
EzeICSchaffnerEFischerESchikowskiTAdamMImbodenMet alLong-term Air Pollution Exposure and Diabetes in a Population-Based Swiss Cohort. Environ Int (2014) 70:95–105. 10.1016/j.envint.2014.05.014
35.
CooganPFWhiteLFJerrettMBrookRDSuJGSetoEet alAir Pollution and Incidence of Hypertension and Diabetes Mellitus in Black Women Living in Los Angeles. Circulation (2012) 125(6):767–72. 10.1161/CIRCULATIONAHA.111.052753
36.
CooganPFWhiteLFYuJBurnettRTMarshallJDSetoEet alLong Term Exposure to NO2 and Diabetes Incidence in the Black Women's Health Study. Environ Res (2016) 148:360–6. 10.1016/j.envres.2016.04.021
37.
KramerUHerderCSugiriDStrassburgerKSchikowskiTRanftUet alTraffic-related Air Pollution and Incident Type 2 Diabetes: Results from the SALIA Cohort Study. Environ Health Perspect (2010) 118(9):1273–9. 10.1289/ehp.0901689
38.
LazarevicNDobsonAJBarnettAGKnibbsLD. Long-term Ambient Air Pollution Exposure and Self-Reported Morbidity in the Australian Longitudinal Study on Women's Health: a Cross-Sectional Study. BMJ Open (2015) 5(10):e008714. 10.1136/bmjopen-2015-008714
39.
WeinmayrGHennigFFuksKNonnemacherMJakobsHMohlenkampSet alLong-term Exposure to fine Particulate Matter and Incidence of Type 2 Diabetes Mellitus in a Cohort Study: Effects of Total and Traffic-specific Air Pollution. Environ Health (2015) 14:53. 10.1186/s12940-015-0031-x
40.
BaiLChenHHatzopoulouMJerrettMKwongJCBurnettRTet alExposure to Ambient Ultrafine Particles and Nitrogen Dioxide and Incident Hypertension and Diabetes. Epidemiology (2018) 29(3):323–32. 10.1097/EDE.0000000000000798
41.
ClarkCSbihiHTamburicLBrauerMFrankLDDaviesHW. Association of Long-Term Exposure to Transportation Noise and Traffic-Related Air Pollution with the Incidence of Diabetes: A Prospective Cohort Study. Environ Health Perspect (2017) 125(8):087025. 10.1289/EHP1279
42.
HowellNATuJVMoineddinRChenHChuAHystadPet alInteraction between Neighborhood Walkability and Traffic-Related Air Pollution on Hypertension and Diabetes: The CANHEART Cohort. Environ Int (2019) 132:104799. 10.1016/j.envint.2019.04.070
43.
YangBYGuoYMarkevychIQianZMBloomMSHeinrichJet alAssociation of Long-Term Exposure to Ambient Air Pollutants with Risk Factors for Cardiovascular Disease in China. JAMA Netw Open (2019) 2(3):e190318. 10.1001/jamanetworkopen.2019.0318
44.
DzhambovAMDimitrovaDD. Exposures to Road Traffic, Noise, and Air Pollution as Risk Factors for Type 2 Diabetes: A Feasibility Study in Bulgaria. Noise Health (2016) 18(82):133–42. 10.4103/1463-1741.181996
45.
AndersenZJRaaschou-NielsenOKetzelMJensenSSHvidbergMLoftSet alDiabetes Incidence and Long-Term Exposure to Air Pollution: a Cohort Study. Diabetes Care (2012) 35(1):92–8. 10.2337/dc11-1155
46.
SørensenMPoulsenAHHvidtfeldtUAFrohnLMKetzelMChristensenJHet alExposure to Source-specific Air Pollution and Risk for Type 2 Diabetes: a Nationwide Study Covering Denmark. Int J Epidemiol (2022) 51(4):1219–29. 10.1093/ije/dyac040
47.
LuchtSHennigFMoebusSOhlweinSHerderCKowallBet alAll-source and Source-specific Air Pollution and 10-year Diabetes Incidence: Total Effect and Mediation Analyses in the Heinz Nixdorf Recall Study. Environ Int (2020) 136:105493. 10.1016/j.envint.2020.105493
48.
ZhaoZLinFWangBCaoYHouXWangY. Residential Proximity to Major Roadways and Risk of Type 2 Diabetes Mellitus: A Meta-Analysis. Int J Environ Res Public Health (2016) 14(1):3. 10.3390/ijerph14010003
49.
ChenMLiangSQinXZhangLQiuLChenSet alPrenatal Exposure to Diesel Exhaust PM(2.5) Causes Offspring β Cell Dysfunction in Adulthood. Am J Physiol Endocrinol Metab (2018) 315(1):E72–E80. 10.1152/ajpendo.00336.2017
50.
ChenMLiangSZhouHXuYQinXHuZet alPrenatal and Postnatal Mothering by Diesel Exhaust PM(2.5)-exposed Dams Differentially Program Mouse Energy Metabolism. Part Fibre Toxicol (2017) 14(1):3. 10.1186/s12989-017-0183-7
51.
YanYHChouCCLeeCTLiuJYChengTJ. Enhanced Insulin Resistance in Diet-Induced Obese Rats Exposed to fine Particles by Instillation. Inhal Toxicol (2011) 23(9):507–19. 10.3109/08958378.2011.587472
52.
ForastiereFPetersA. Invited Perspective: The NO2 and Mortality Dilemma Solved? Almost There. Environ Health Perspect (2021) 129(12):121304. 10.1289/EHP10286
53.
KarouiACrochemoreCHaroukiNCorbiereCPreterreDVendevilleCet alNitrogen Dioxide Inhalation Exposures Induce Cardiac Mitochondrial Reactive Oxygen Species Production, Impair Mitochondrial Function and Promote Coronary Endothelial Dysfunction. Int J Environ Res Public Health (2020) 17(15):5526. 10.3390/ijerph17155526
54.
HeydariHNajafiMLAkbariARezaeiHMiriM. Prenatal Exposure to Traffic-Related Air Pollution and Glucose Homeostasis: A Cross-Sectional Study. Environ Res (2021) 201:111504. 10.1016/j.envres.2021.111504
55.
Toledo-CorralCMAldereteTLHabreRBerhaneKLurmannFWWeigensbergMJet alEffects of Air Pollution Exposure on Glucose Metabolism in Los Angeles Minority Children. Pediatr Obes (2018) 13(1):54–62. 10.1111/ijpo.12188
56.
MannJKLutzkerLHolmSMMargolisHGNeophytouAMEisenEAet alTraffic-related Air Pollution Is Associated with Glucose Dysregulation, Blood Pressure, and Oxidative Stress in Children. Environ Res (2021) 195:110870. 10.1016/j.envres.2021.110870
57.
ThieringEMarkevychIBrüskeIFuertesEKratzschJSugiriDet alAssociations of Residential Long-Term Air Pollution Exposures and Satellite-Derived Greenness with Insulin Resistance in German Adolescents. Environ Health Perspect (2016) 124(8):1291–8. 10.1289/ehp.1509967
58.
ZhangSMwiberiSPickfordRBreitnerSHuthCKoenigWet alLongitudinal Associations between Ambient Air Pollution and Insulin Sensitivity: Results from the KORA Cohort Study. Lancet Planet Health (2021) 5(1):e39–e49. 10.1016/S2542-5196(20)30275-8
59.
ChenQGalfalvyHDuanN. Effects of Disease Misclassification on Exposure-Disease Association. Am J Public Health (2013) 103(5):e67–73. 10.2105/AJPH.2012.300995
60.
CopelandKTCheckowayHMcMichaelAJHolbrookRH. Bias Due to Misclassification in the Estimation of Relative Risk. Am J Epidemiol (1977) 105(5):488–95. 10.1093/oxfordjournals.aje.a112408
61.
RugelEJBrauerM. Quiet, Clean, green, and Active: A Navigation Guide Systematic Review of the Impacts of Spatially Correlated Urban Exposures on a Range of Physical Health Outcomes. Environ Res (2020) 185:109388. 10.1016/j.envres.2020.109388
62.
RaghuveerGWhiteDAHaymanLLWooJGVillafaneJCelermajerDet alCardiovascular Consequences of Childhood Secondhand Tobacco Smoke Exposure: Prevailing Evidence, Burden, and Racial and Socioeconomic Disparities: A Scientific Statement from the American Heart Association. Circulation (2016) 134(16):e336–e359. 10.1161/CIR.0000000000000443
63.
DijkemaMBMallantSFGehringUvan den HurkKAlssemaMvan StrienRTet alLong-term Exposure to Traffic-Related Air Pollution and Type 2 Diabetes Prevalence in a Cross-Sectional Screening-Study in the Netherlands. Environ Health (2011) 10:76. 10.1186/1476-069X-10-76
64.
LiYLaneKJCorlinLPattonAPDurantJLThanikachalamMet alAssociation of Long-Term Near-Highway Exposure to Ultrafine Particles with Cardiovascular Diseases, Diabetes and Hypertension. Int J Environ Res Public Health (2017) 14(5):461. 10.3390/ijerph14050461
65.
O'DonovanGChudasamaYGrocockSLeighRDaltonAMGrayLJet alThe Association between Air Pollution and Type 2 Diabetes in a Large Cross-Sectional Study in Leicester: The CHAMPIONS Study. Environ Int (2017) 104:41–7. 10.1016/j.envint.2017.03.027
66.
ParkSKAdarSDO'NeillMSAuchinclossAHSzpiroABertoniAGet alLong-term Exposure to Air Pollution and Type 2 Diabetes Mellitus in a Multiethnic Cohort. Am J Epidemiol (2015) 181(5):327–36. 10.1093/aje/kwu280
67.
PuettRCHartJESchwartzJHuFBLieseADLadenF. Are Particulate Matter Exposures Associated with Risk of Type 2 Diabetes?Environ Health Perspect (2011) 119(3):384–9. 10.1289/ehp.1002344
68.
RiantMMeirhaegheAGiovannelliJOccelliFHavetACunyDet alAssociations between Long-Term Exposure to Air Pollution, Glycosylated Hemoglobin, Fasting Blood Glucose and Diabetes Mellitus in Northern France. Environ Int (2018) 120:121–9. 10.1016/j.envint.2018.07.034
69.
YangBYQianZMLiSChenGBloomMSElliottMet alAmbient Air Pollution in Relation to Diabetes and Glucose-Homoeostasis Markers in China: a Cross-Sectional Study with Findings from the 33 Communities Chinese Health Study. Lancet Planet Health (2018) 2(2):e64–e73. 10.1016/S2542-5196(18)30001-9
70.
SuryadhiMAHSuryadhiPARAbudureyimuKRumaIMWCalliopeASWirawanDNet alExposure to Particulate Matter (PM(2.5)) and Prevalence of Diabetes Mellitus in Indonesia. Environ Int (2020) 140:105603. 10.1016/j.envint.2020.105603
71.
WeaverAMBidulescuAWelleniusGAHicksonDASimsMVaidyanathanAet alAssociations between Air Pollution Indicators and Prevalent and Incident Diabetes in an African American Cohort, the Jackson Heart Study. Environ Epidemiol (2021) 5(3):e140. 10.1097/EE9.0000000000000140
72.
YuYJerrettMPaulKCSuJShihIFWuJet alOzone Exposure, Outdoor Physical Activity, and Incident Type 2 Diabetes in the SALSA Cohort of Older Mexican Americans. Environ Health Perspect (2021) 129(9):97004. 10.1289/EHP8620
Summary
Keywords
diabetes, particulate matter, traffic-related air pollution, NO2, confidence assessment
Citation
Kutlar Joss M, Boogaard H, Samoli E, Patton AP, Atkinson R, Brook J, Chang H, Haddad P, Hoek G, Kappeler R, Sagiv S, Smargiassi A, Szpiro A, Vienneau D, Weuve J, Lurmann F, Forastiere F and Hoffmann BH (2023) Long-Term Exposure to Traffic-Related Air Pollution and Diabetes: A Systematic Review and Meta-Analysis. Int J Public Health 68:1605718. doi: 10.3389/ijph.2023.1605718
Received
24 December 2022
Accepted
15 May 2023
Published
31 May 2023
Volume
68 - 2023
Edited by
Heresh Amini, Icahn School of Medicine at Mount Sinai, United States
Reviewed by
Pablo Knobel, Icahn School of Medicine at Mount Sinai, United States
Melissa Fiffer, University of Notre Dame, United States
Steffen Loft, University of Copenhagen, Denmark
Updates
Copyright
© 2023 Kutlar Joss, Boogaard, Samoli, Patton, Atkinson, Brook, Chang, Haddad, Hoek, Kappeler, Sagiv, Smargiassi, Szpiro, Vienneau, Weuve, Lurmann, Forastiere and Hoffmann.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Meltem Kutlar Joss, meltem.kutlar@swisstph.ch
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.